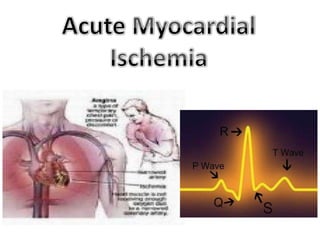
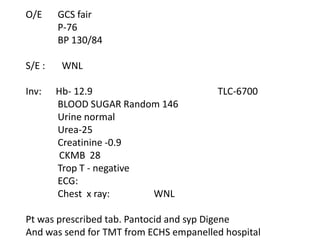
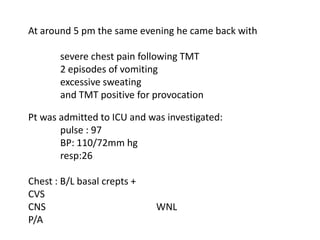
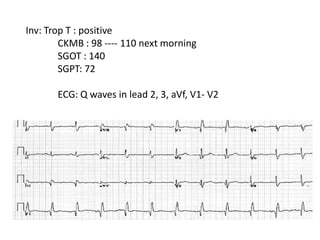
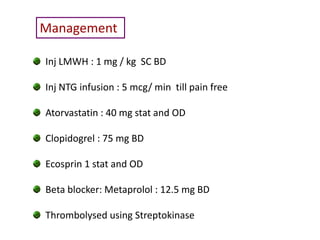
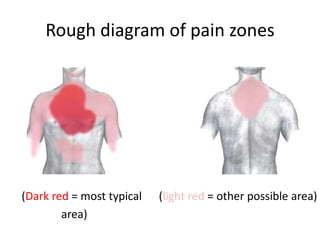
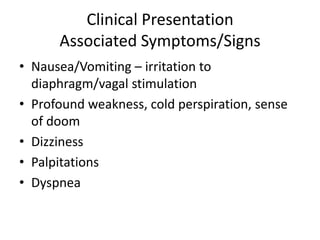
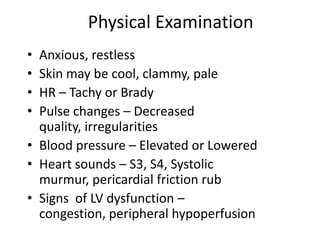
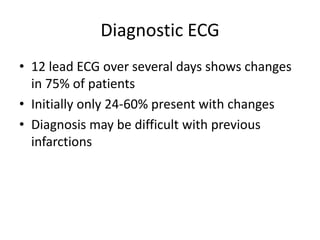
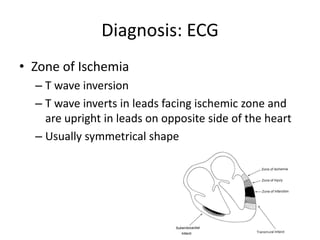
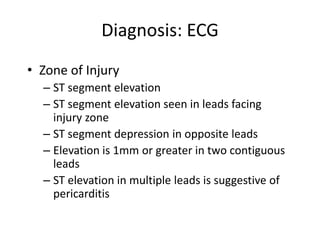
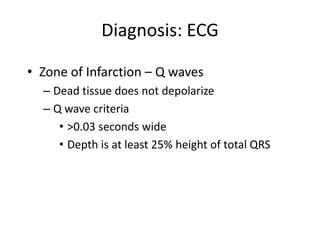
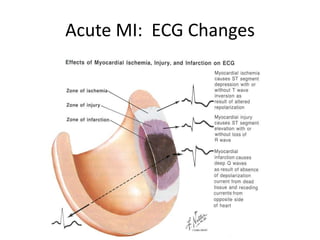
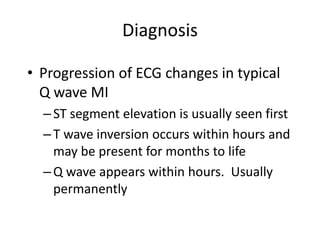
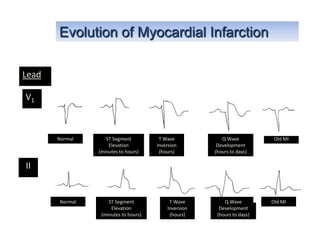
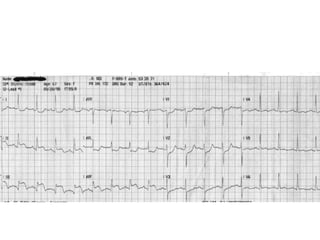
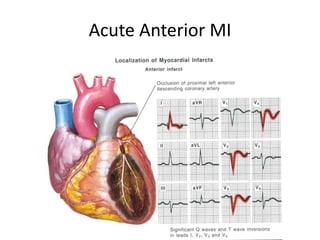
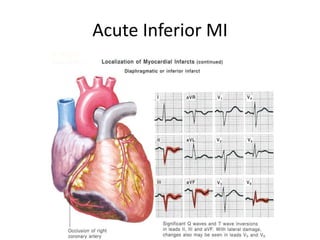
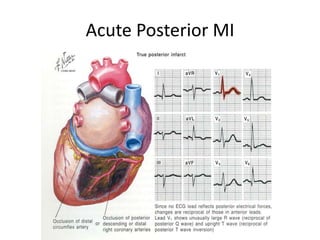
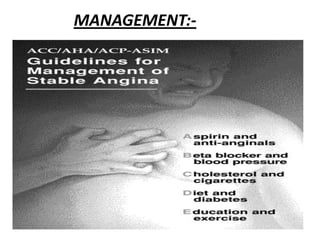
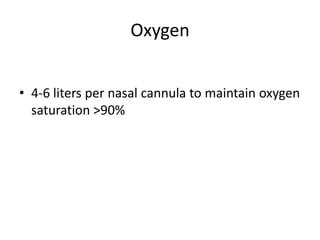
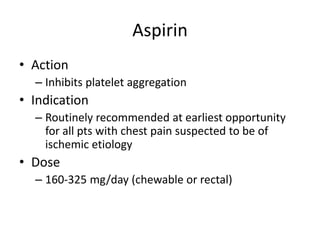
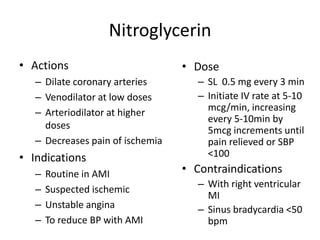
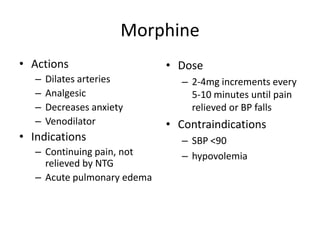
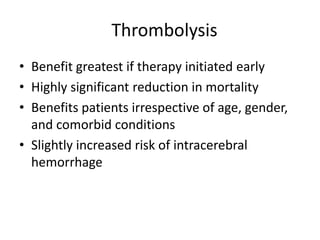
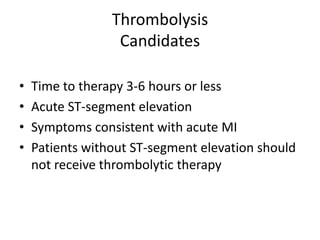
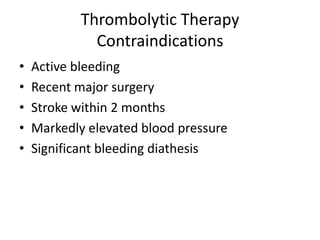
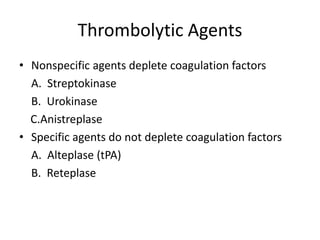
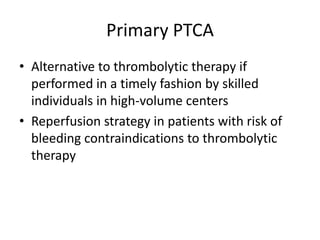
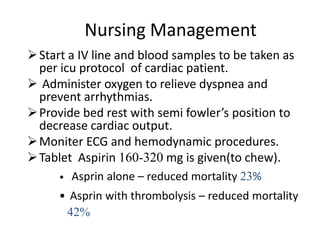
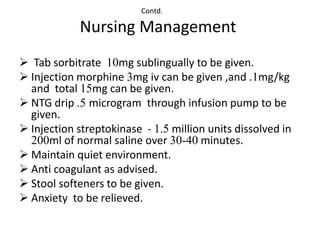
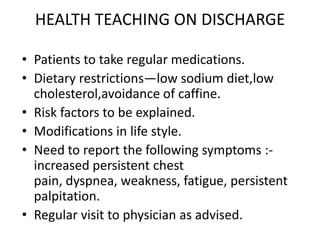
A 55-year-old male smoker and alcoholic presented with chest pain and was diagnosed with a myocardial infarction based on electrocardiogram and cardiac enzyme changes. He received treatment including aspirin, nitroglycerin, morphine, and streptokinase thrombolysis and was admitted to the intensive care unit. Nursing care focused on monitoring, providing pain relief, and health teaching prior to discharge.