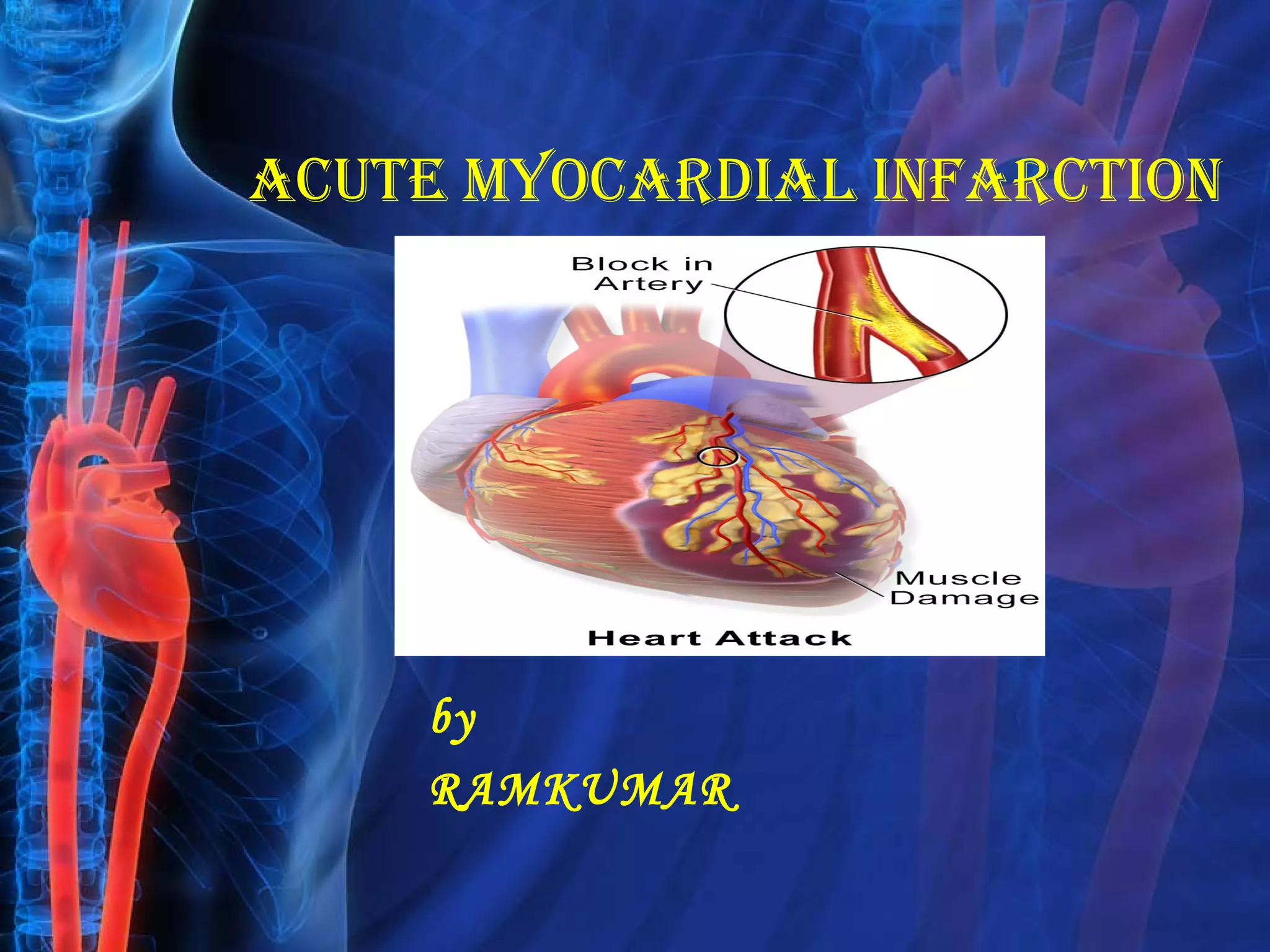
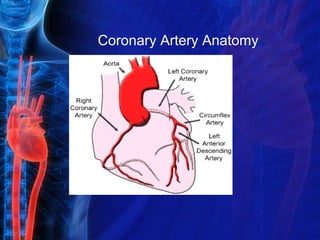
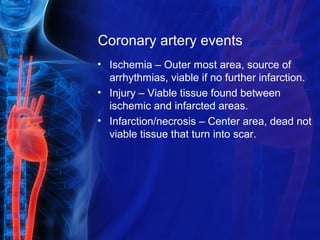
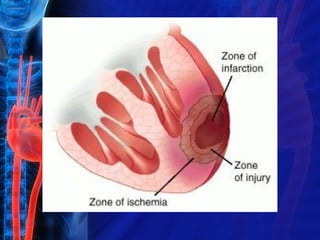
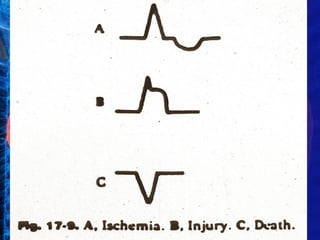
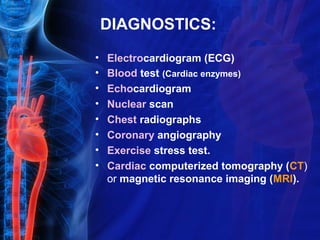
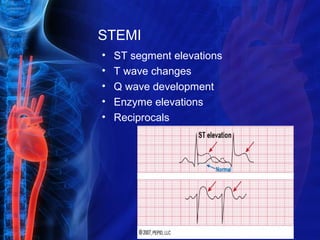
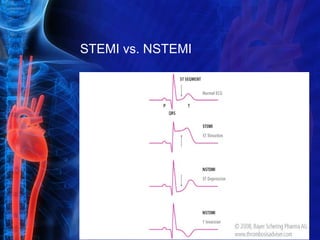
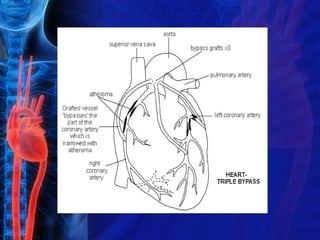
Acute myocardial infarction, or heart attack, occurs when blood supply to the heart is diminished leading to cell damage and death. It is usually caused by a blockage in the coronary arteries from atherosclerotic plaque or a blood clot. Diagnosis involves EKGs, blood tests of cardiac enzymes, and imaging tests. Treatment depends on the type and severity of MI but may include medications to break up clots, angioplasty and stenting, or coronary bypass surgery. Complications can affect the heart muscles and blood vessels if not properly treated.