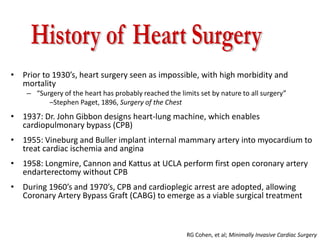
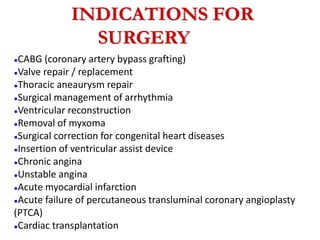
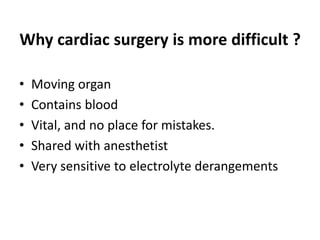
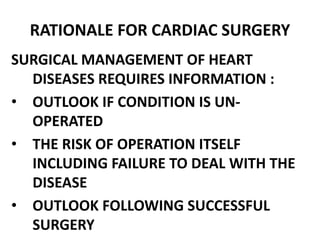
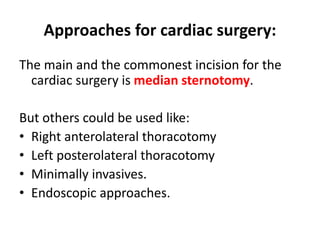
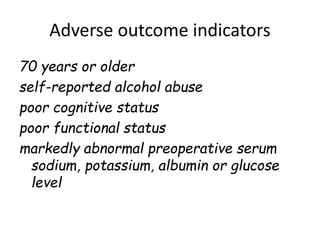
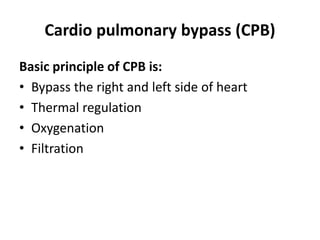
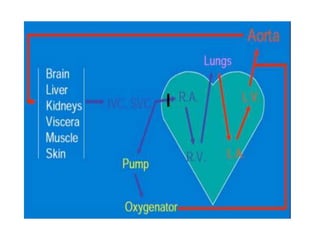
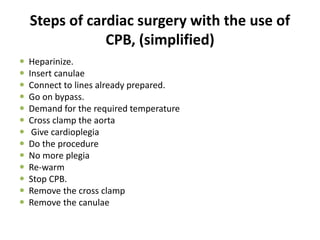
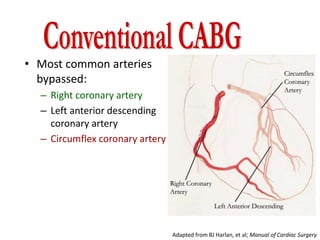
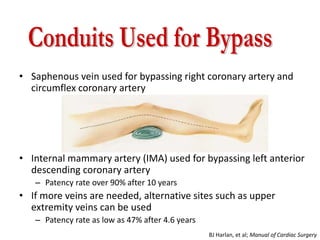
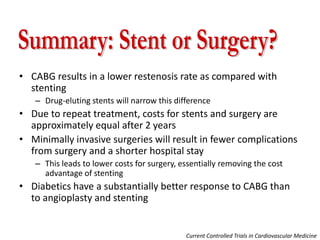
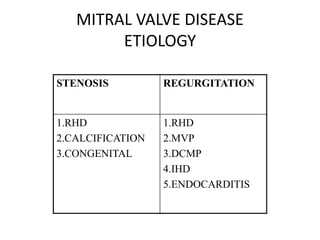
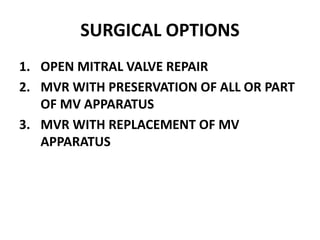
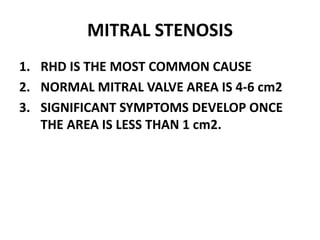
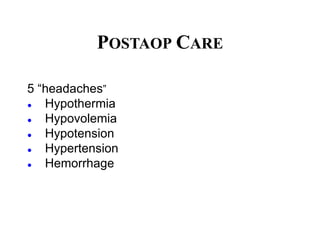
Cardiac surgery is more difficult than other types of surgery due to the moving heart organ containing blood which is vital with no room for mistakes. Historical milestones like the heart-lung machine in 1937 and first coronary artery bypass graft in 1958 allowed cardiac surgery to become viable. Indications for cardiac surgery include CABG, valve repair/replacement, arrhythmia management, and congenital heart defects. Preop preparation assesses patient risk factors. During surgery, a heart-lung machine is used to bypass the heart and oxygenate blood while the surgeon operates. Common procedures like CABG graft arteries to improve blood flow. Postop care focuses on complications like hypothermia, bleeding, and low blood pressure.