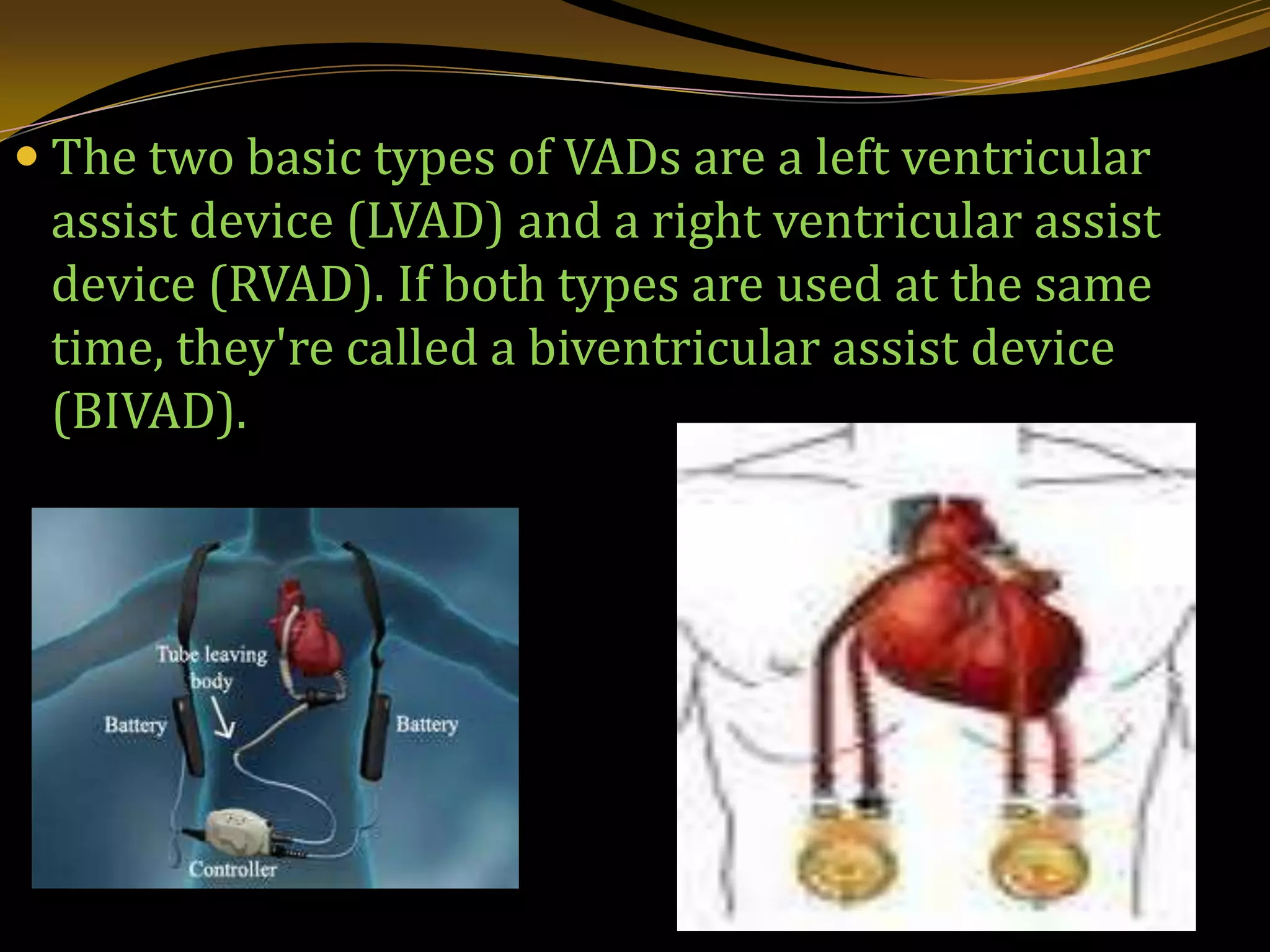
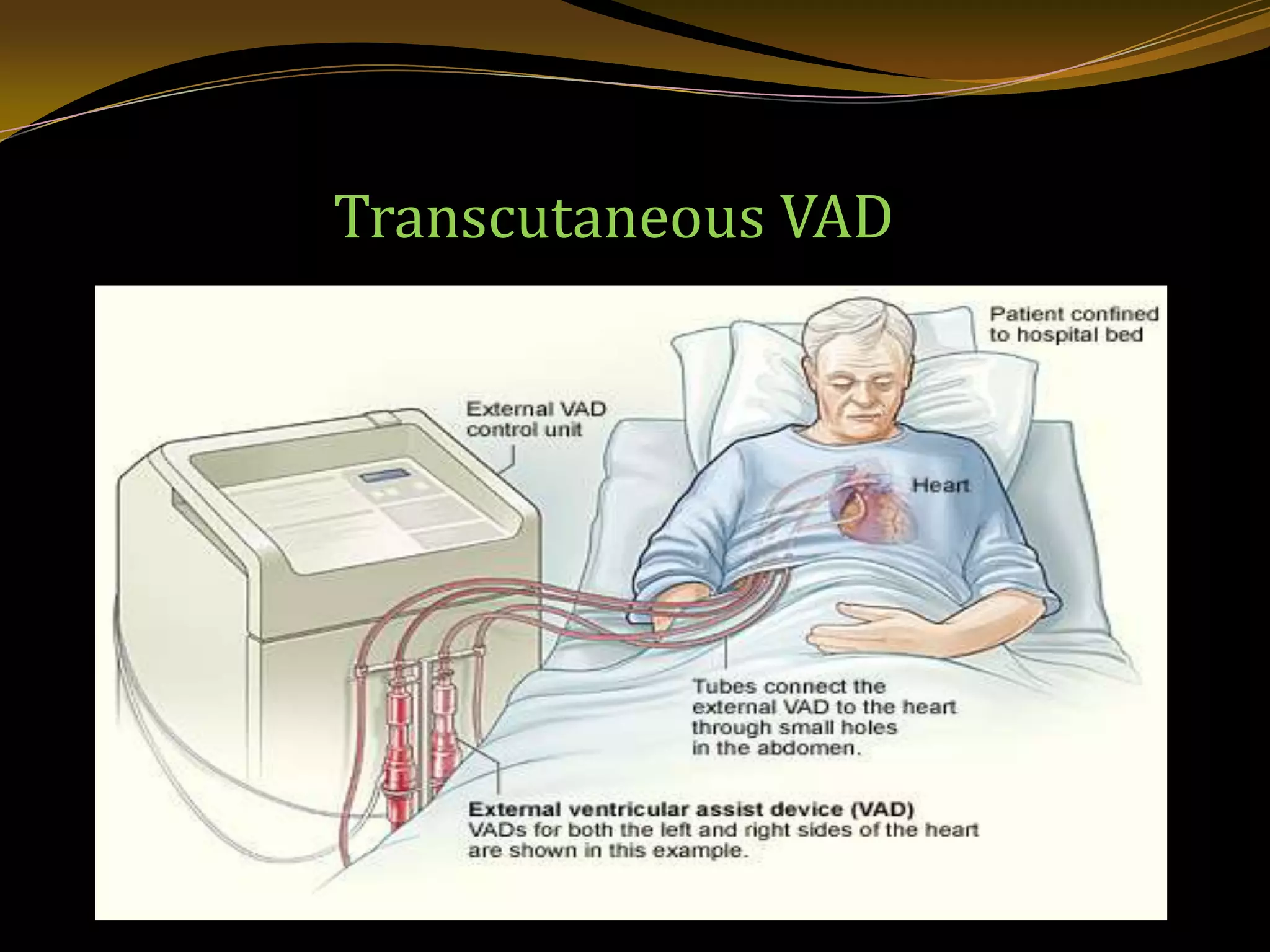
A ventricular assist device (VAD) is a mechanical pump that helps the failing heart pump blood. Some VADs are short-term, while others provide long-term support. The most common type is the left ventricular assist device (LVAD) which helps the left ventricle. VADs carry risks like infection, blood clots, and device malfunctions but can help patients live longer while waiting for a heart transplant or serve as permanent heart failure treatment. After surgery, patients recover in the hospital while taking medications and regaining strength. Living with a VAD requires ongoing monitoring but allows many to return to normal activities with doctor approval.