The document discusses heart transplantation, including:
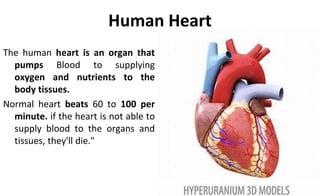
- The normal function of the human heart and what happens when it is not able to supply blood properly.
- That heart transplantation involves replacing a damaged heart with a healthy donor heart through surgery.
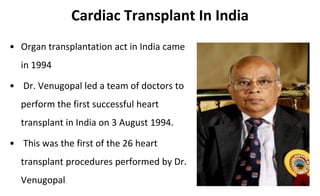
- Some details about the first successful heart transplant performed in India in 1994 and hospitals approved to perform the procedure.
- Criteria for determining donor heart suitability and matching it to a recipient, including blood type and body size compatibility.
- Indications and contraindications for receiving a heart transplant.
- Surgical techniques for transplantation, including the biatrial technique which is the standard orthotopic heart transplant procedure.




![Criteria For Determining Brain Death
Clinical Evaluation
• Mechanism of brain injury is sufficient to account for irreversible loss
of brain function
• Absence of reversible causes of CNS depression
• CNS depressant drugs
• Hypothermia (<32°C [85°F])
• Hypotension (MAP <55 mmHg)
• Absence of neuromuscular blocking drugs that may confound the
results of the neurologic exam
• No spontaneous movements, motor responses, or posturing](https://image.slidesharecdn.com/hearttyransplantation-190912083604/85/Heart-tyransplantation-9-320.jpg)
























































