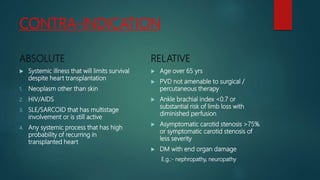
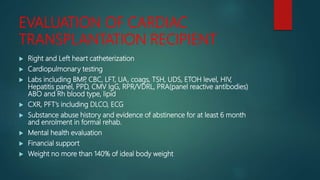
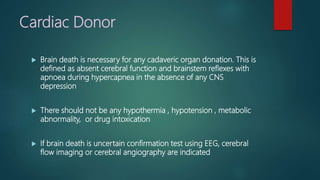
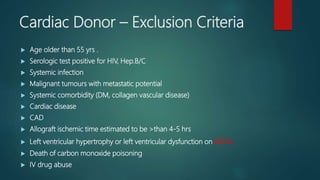
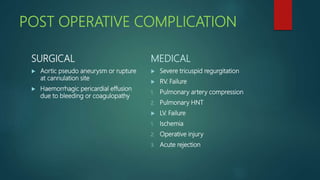
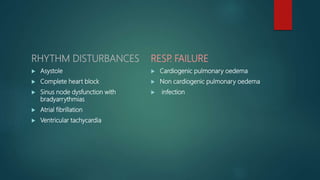
Cardiac transplantation involves surgically implanting a donor heart into a recipient with heart failure. It is indicated for end-stage heart disease that is refractory to maximal medical therapy. Absolute contraindications include active infections, cancers, and pulmonary hypertension. Evaluation of recipients includes cardiac testing and screening for medical/psychosocial risks. Donor hearts must be from brain dead individuals without systemic disease or infection. Post-operative care requires lifelong immunosuppression to prevent rejection while managing complications like infection, rejection, and arrhythmias. Long-term follow-up focuses on screening for issues like allograft vasculopathy.