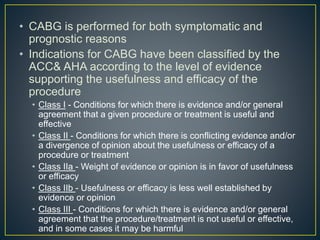
The document discusses guidelines from the ACC/AHA on indications for coronary artery bypass graft (CABG) surgery. It classifies indications into three classes based on evidence: Class I are conditions where CABG is useful and effective, Class II where evidence is conflicting, and Class III where CABG is not useful or effective. It provides the classification for various coronary artery disease presentations such as left main stenosis, multi-vessel disease, and poor left ventricular function. Emergency CABG may be indicated for complications of ST-elevation myocardial infarction.







![• [Guideline] Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR,
Byrne JG, et al. 2011 ACCF/AHA Guideline for Coronary Artery
Bypass Graft Surgery: A Report of the American College of
Cardiology Foundation/American Heart Association Task Force on
Practice Guidelines. Circulation. 2011 Nov 7.[Medline]
• Eagle KA, Guyton RA, Davidoff R, Edwards FH, Ewy GA, Gardner
TJ. ACC/AHA 2004 guideline update for coronary artery bypass graft
surgery: summary article: a report of the American College of
Cardiology/American Heart Association Task Force on Practice
Guidelines (Committee to Update the 1999 Guidelines for Coronary
Artery Bypass Graft Surgery). Circulation. 2004 Aug 31. 110(9):1168-
76. [Medline]
• http://emedicine.medscape.com/article/1893992-overview#a3](https://image.slidesharecdn.com/cabgindications-151112090731-lva1-app6892/85/Cabg-indications-9-320.jpg)