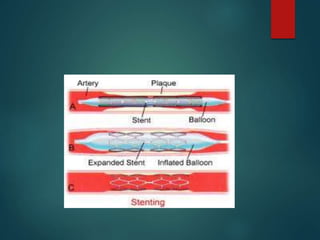
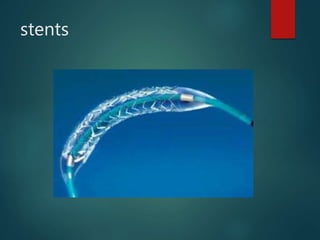
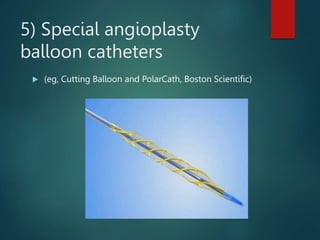
Percutaneous transluminal coronary angioplasty (PTCA) is a minimally invasive procedure used to open blocked coronary arteries and restore blood flow to the heart. During PTCA, a catheter with a deflated balloon at the tip is inserted into the blocked artery and inflated to compress the plaque and widen the artery. Stents may be placed to help keep the artery open. The procedure aims to improve blood supply and relieve symptoms caused by coronary artery disease.