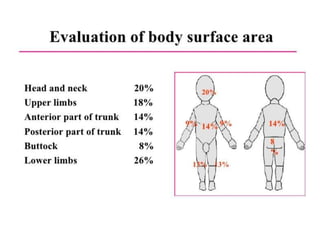
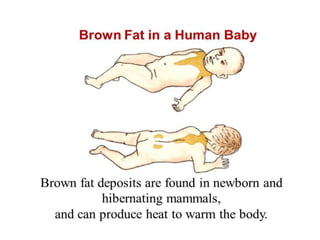
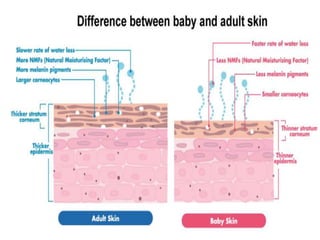
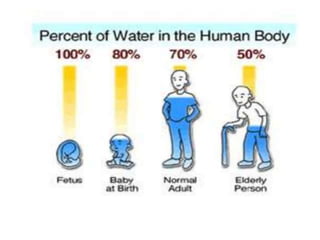
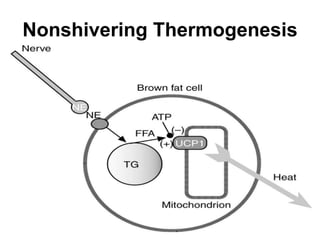
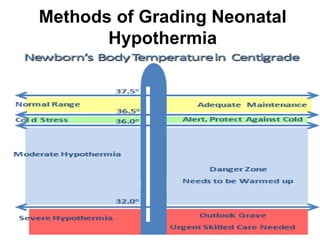
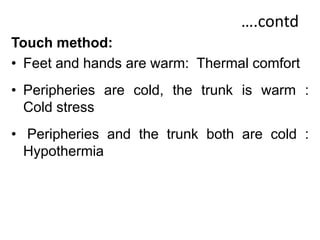
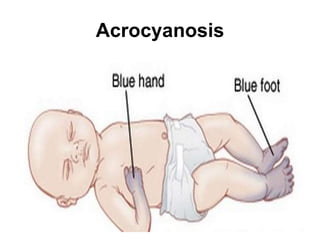
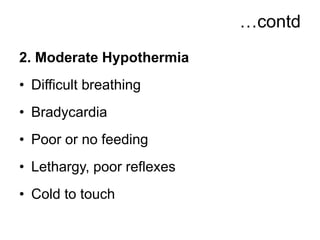
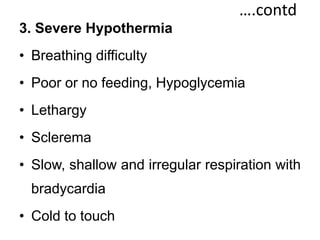
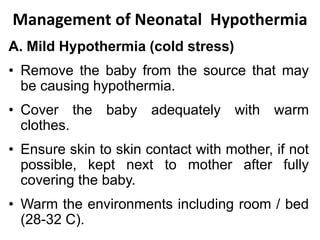
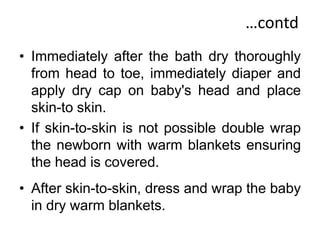
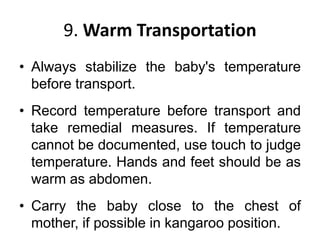
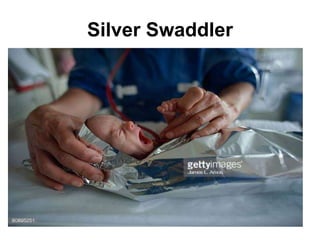
This document discusses neonatal hypothermia, including defining it as an axillary temperature below 36.5°C, identifying factors that cause heat loss in newborns like large surface area and inability to shiver thermogenesis. It describes methods to grade hypothermia severity from mild to severe and associated clinical features. Management involves rewarming techniques based on severity while preventing further heat loss. Complications are also outlined. The focus is on establishing a "warm chain" through various preventive measures from delivery to transportation to reduce neonatal hypothermia risk.