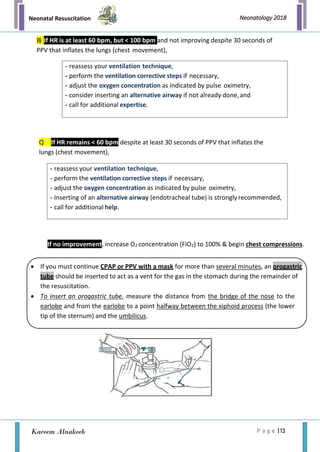
The document outlines the immediate care and resuscitation techniques for newborns in the delivery room, highlighting the physiological transition from fetal to neonatal circulation and the importance of recognizing asphyxia. It details preparation procedures, necessary personnel and equipment, and systematic steps for assessing and performing resuscitation, including positive-pressure ventilation and oxygen management. Key factors affecting the need for resuscitation and potential complications are also emphasized, stressing the critical role of teamwork and immediate intervention.