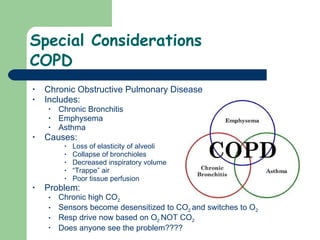
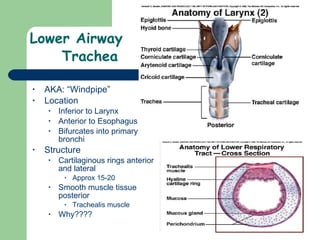
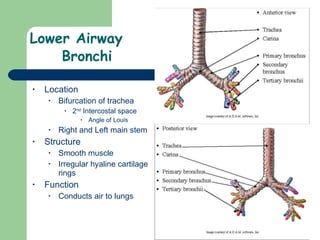
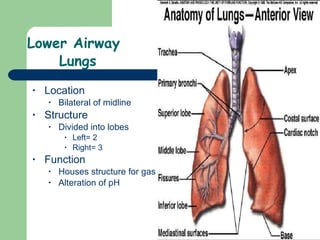
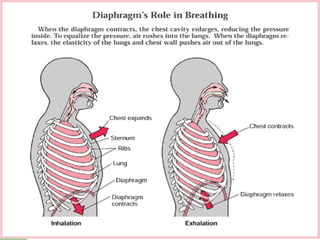
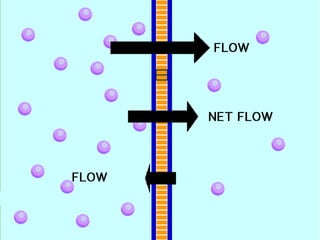
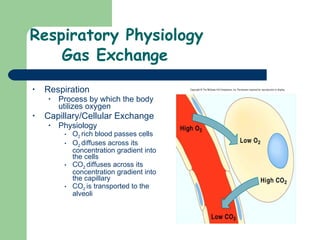
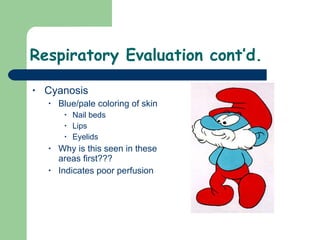
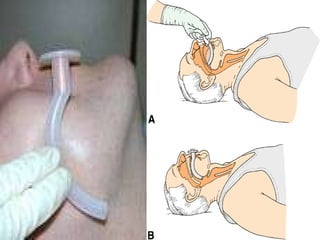
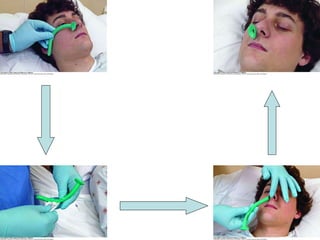
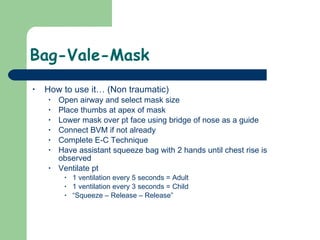
This document provides an overview of the respiratory system, including its structures and functions. It describes the upper airway including the nose, mouth, pharynx and larynx. It then describes the lower airway structures like the trachea, bronchi, bronchioles and lungs. It discusses gas exchange that occurs in the lungs via diffusion between alveoli and capillaries. It also covers respiratory physiology including ventilation, respiration and gas exchange. Finally, it discusses respiratory assessment and various respiratory conditions like distress, failure and arrest as well as airway management techniques.


























































![Cylinder Calculations Can you make it??? Time(min)= (Tank Pressure[psi]-200psi)xConstant Flow Rate (L/min) Constants D cylinder= 0.16 E cylinder= 0.28 M cylinder= 1.56 H cylinder= 3.4 Example You are transporting a patient who is receiving 15L/min of oxygen by NRB. The transport time is 20 min. On your E cylinder, the psi is 1200. Do you have enough oxygen for your patient, of should you prepare to change you settings? Time =(1200psi-200psi)X0.28 15L/min =18 2/3 min = NOT ENOUGH](https://image.slidesharecdn.com/8airway-090910172456-phpapp02/85/8-Airway-73-320.jpg)