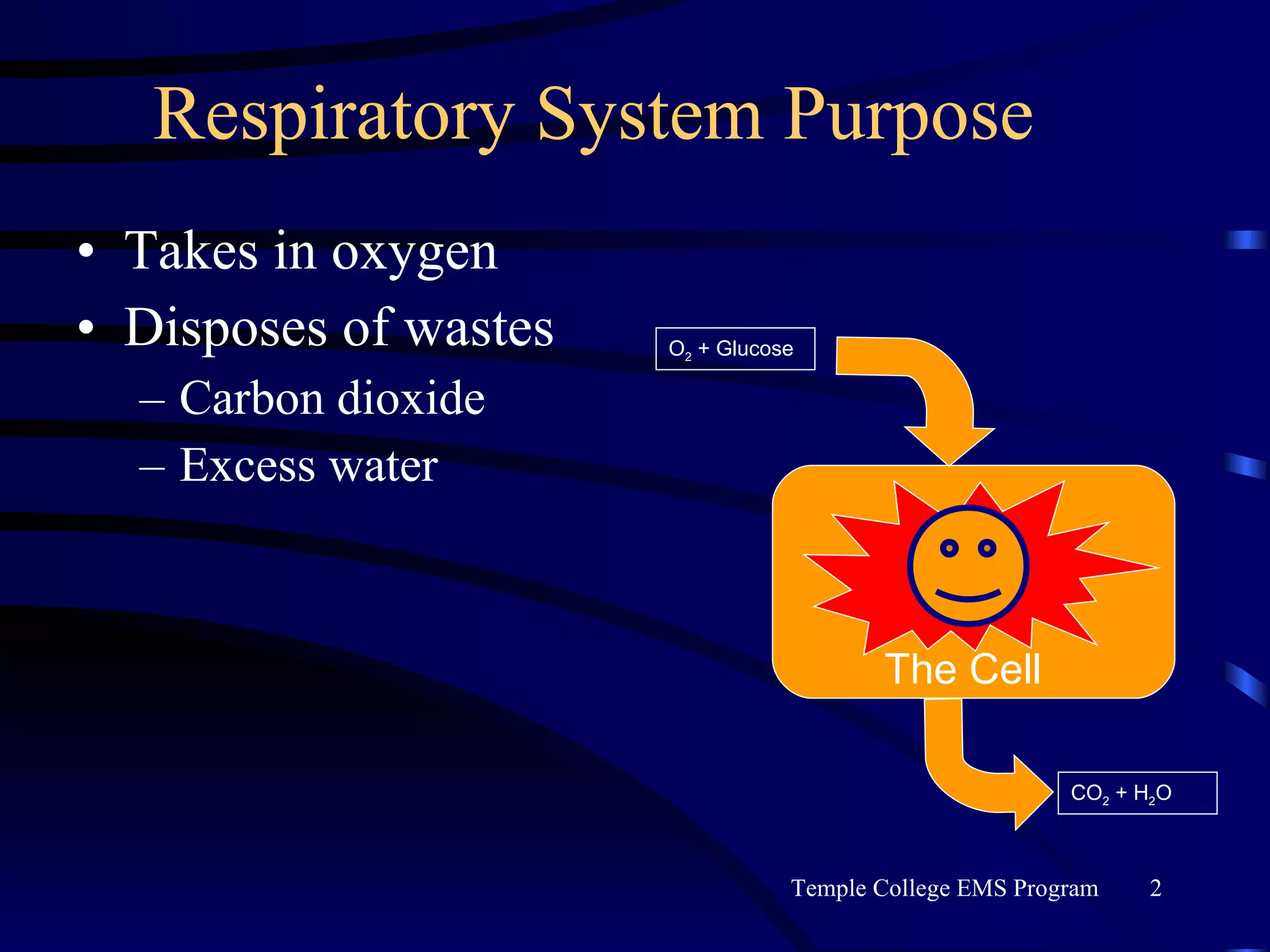
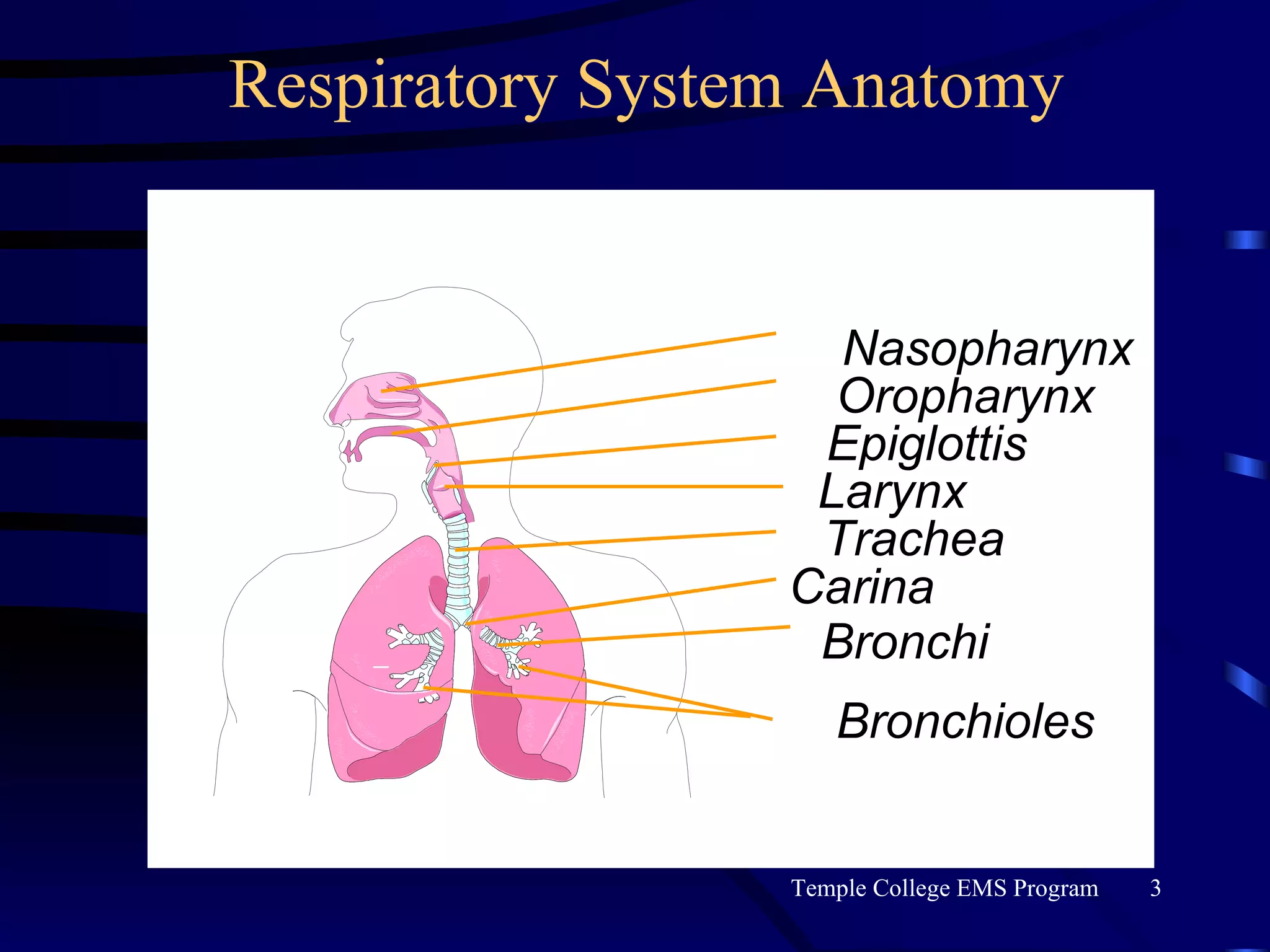
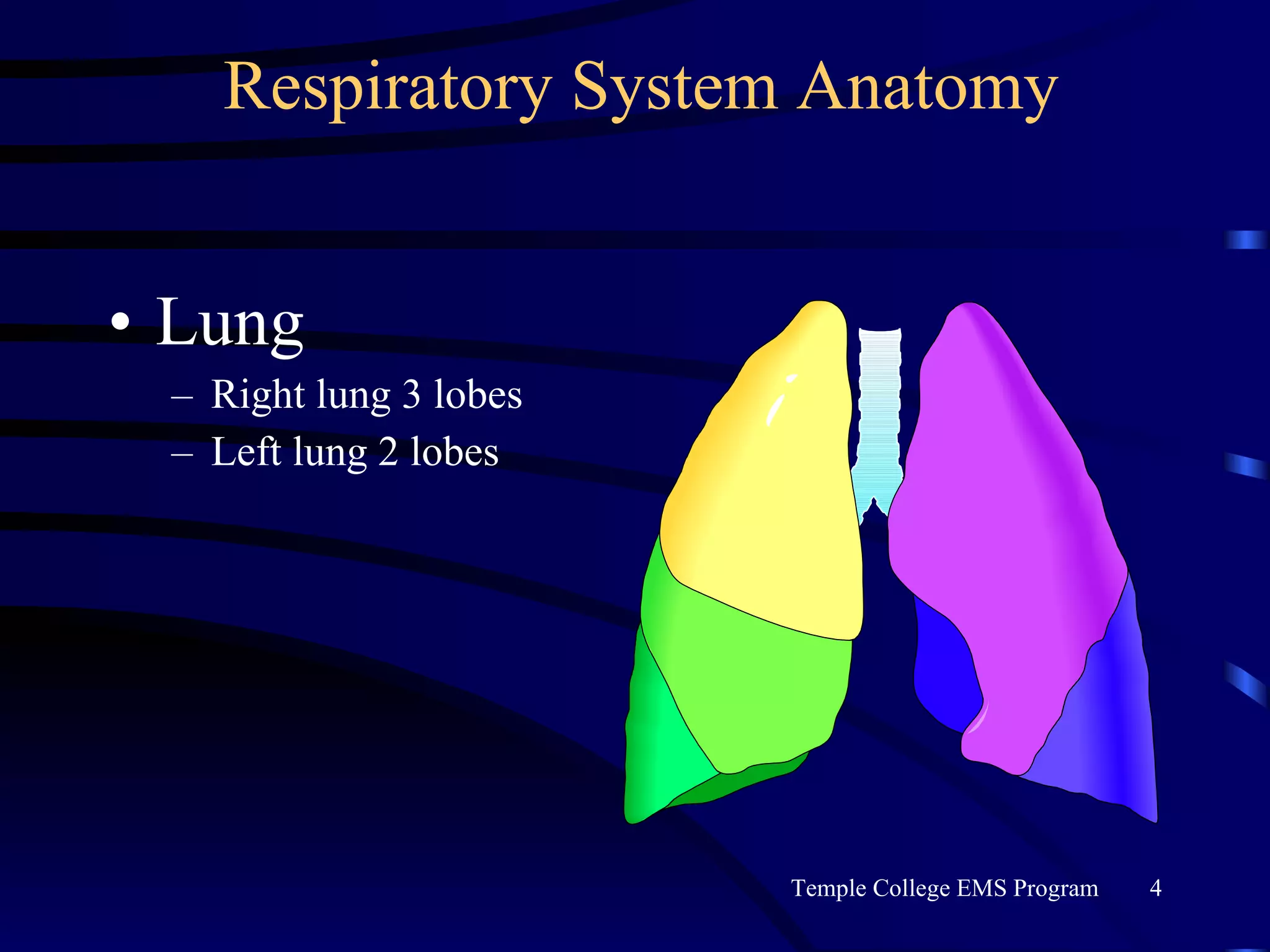
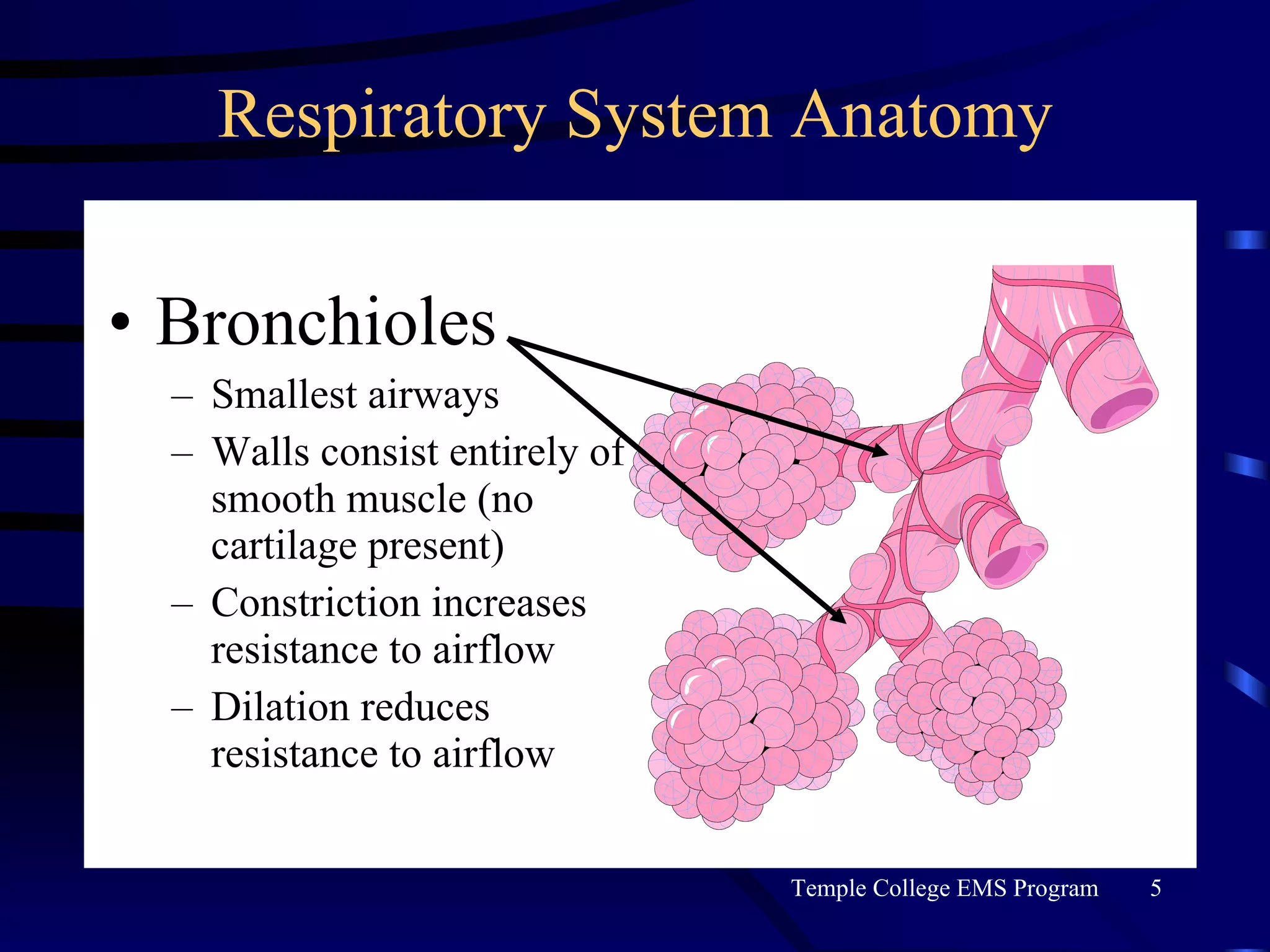
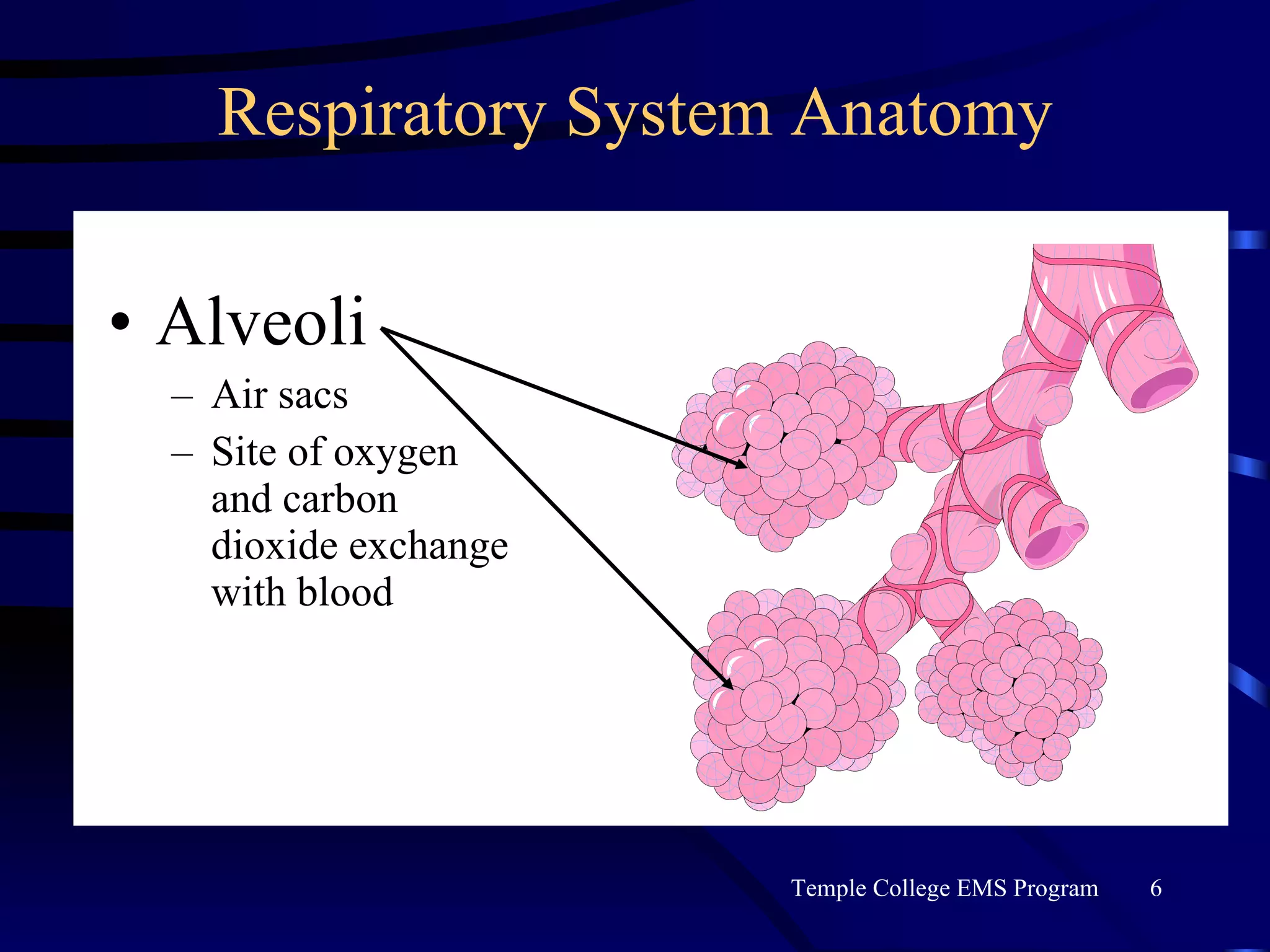
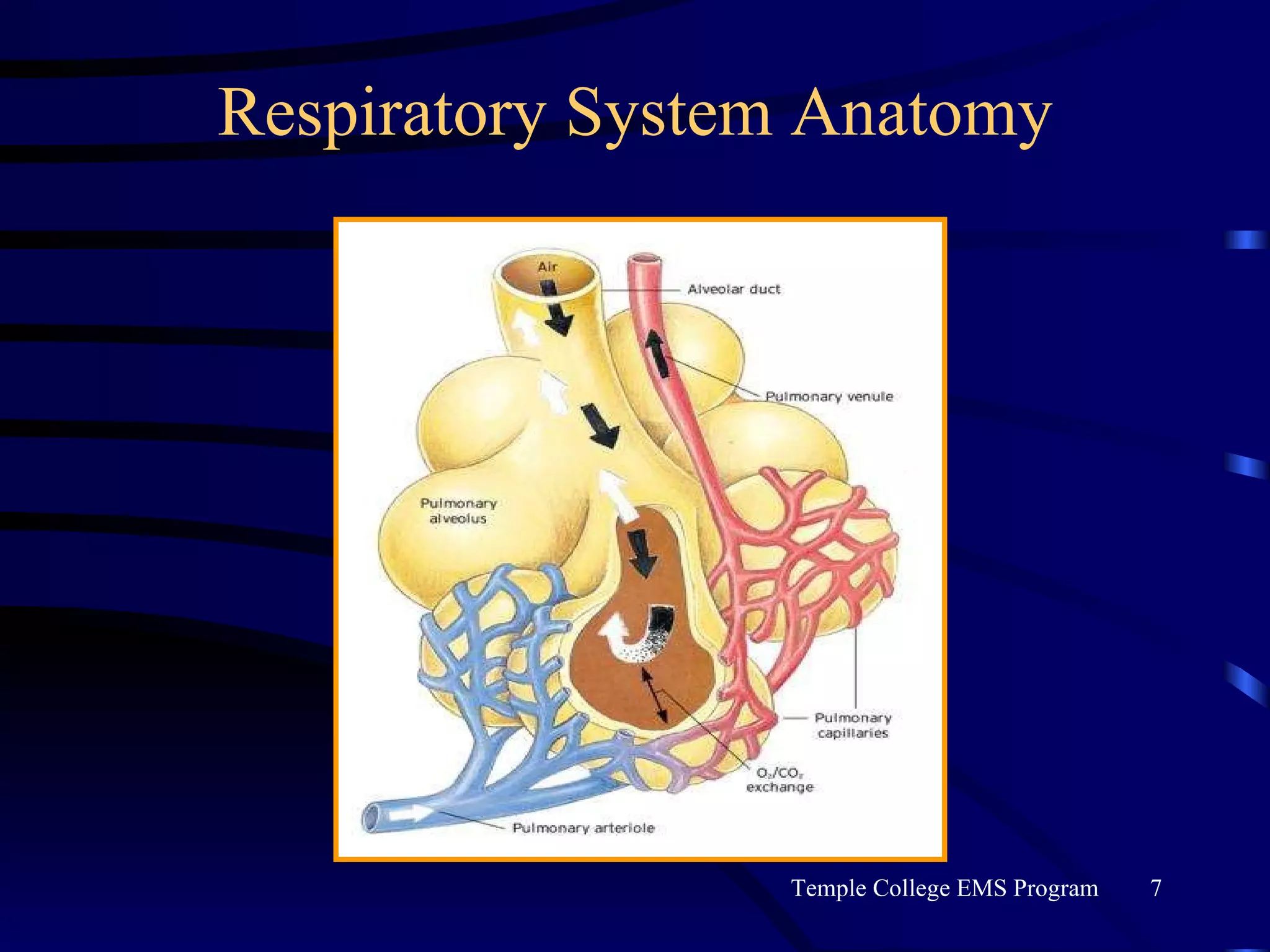
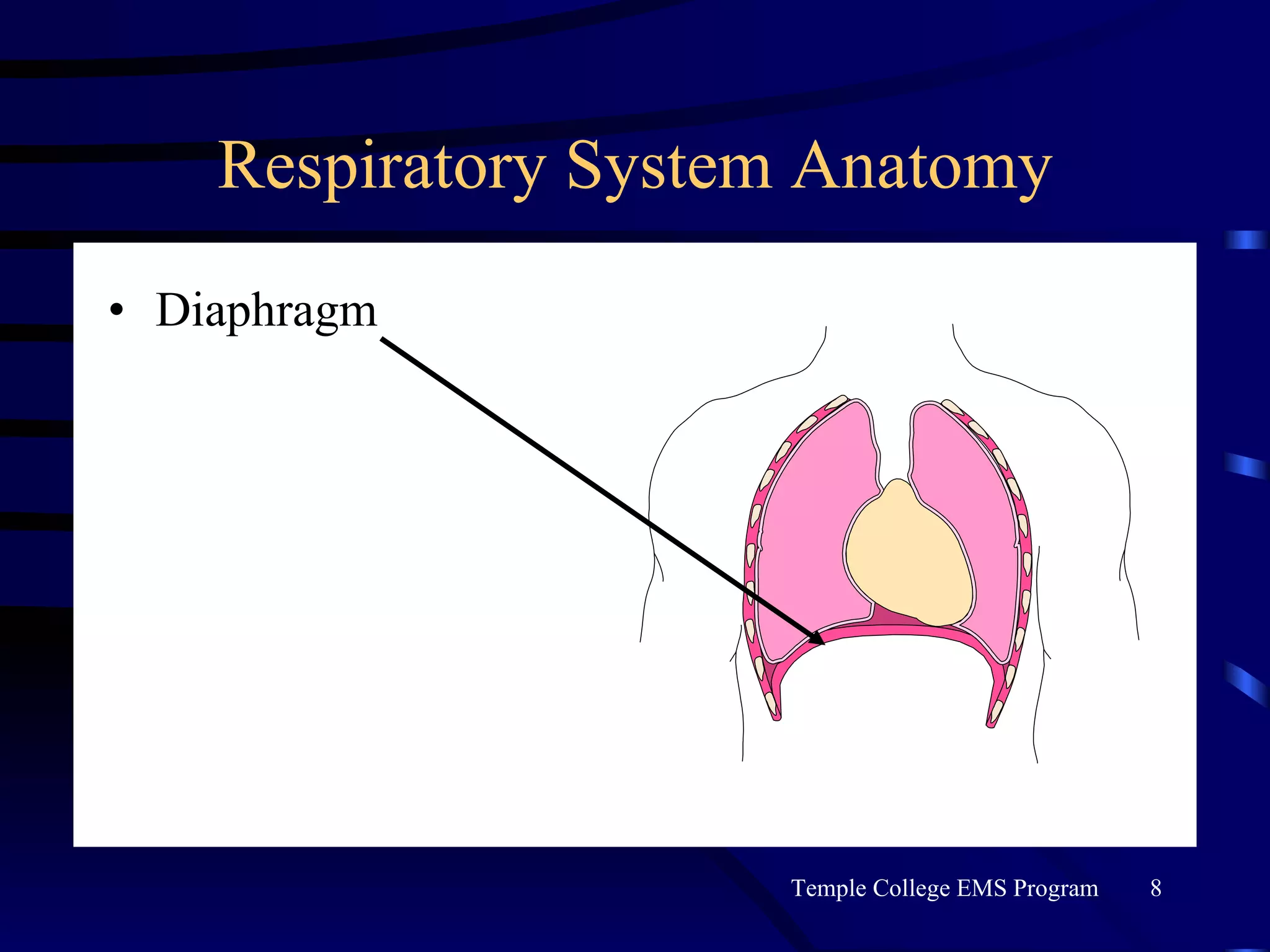
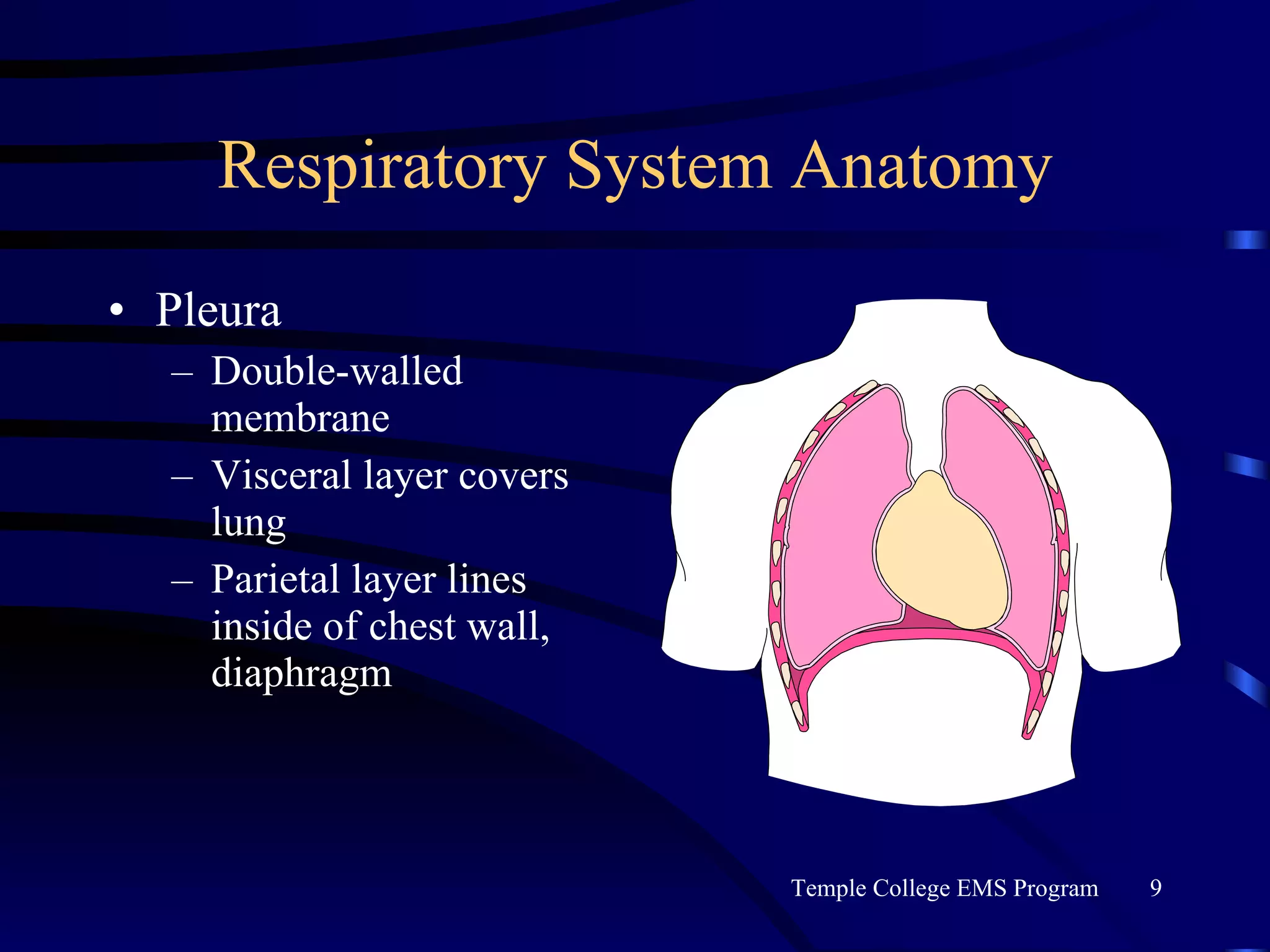
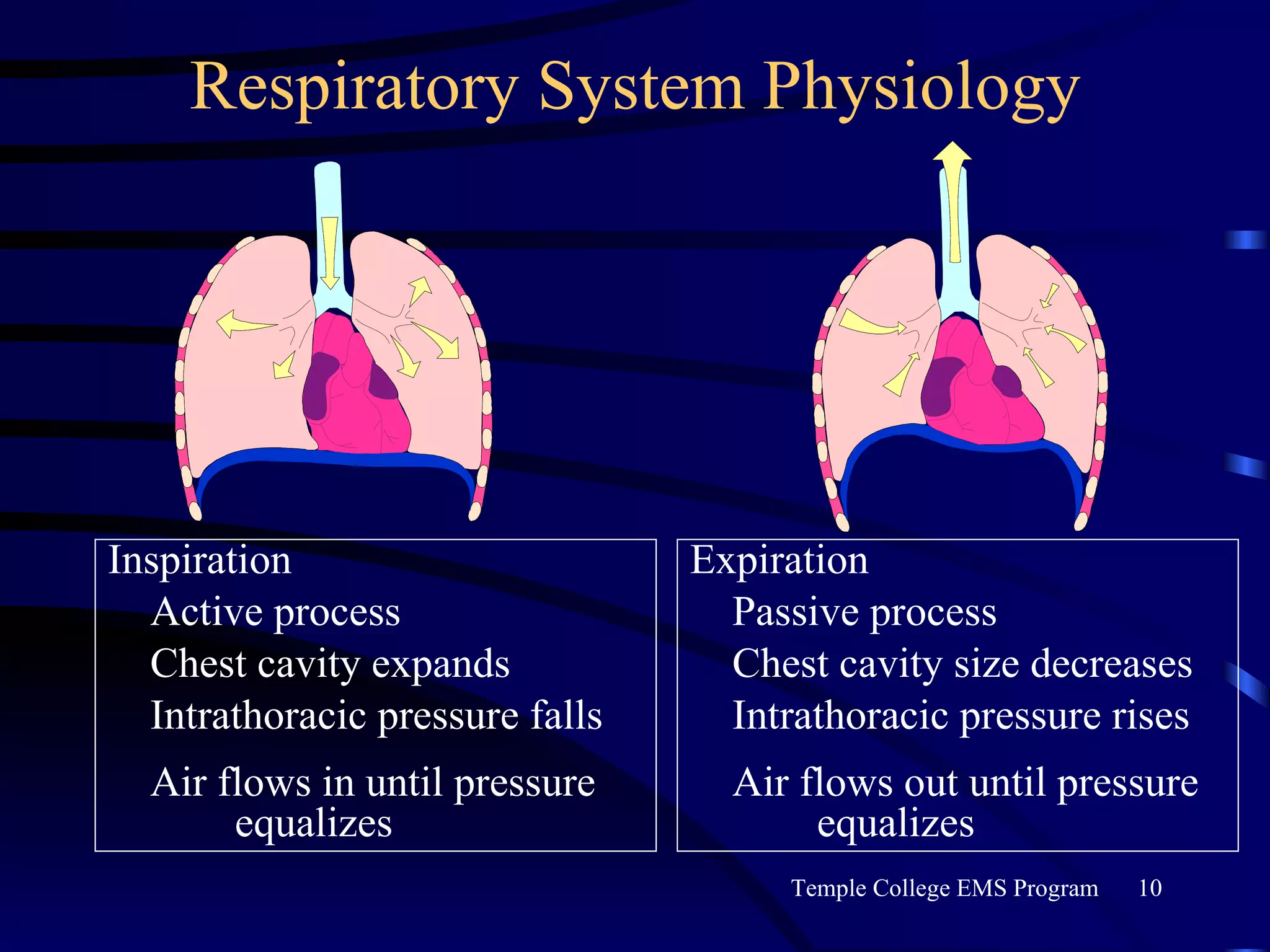
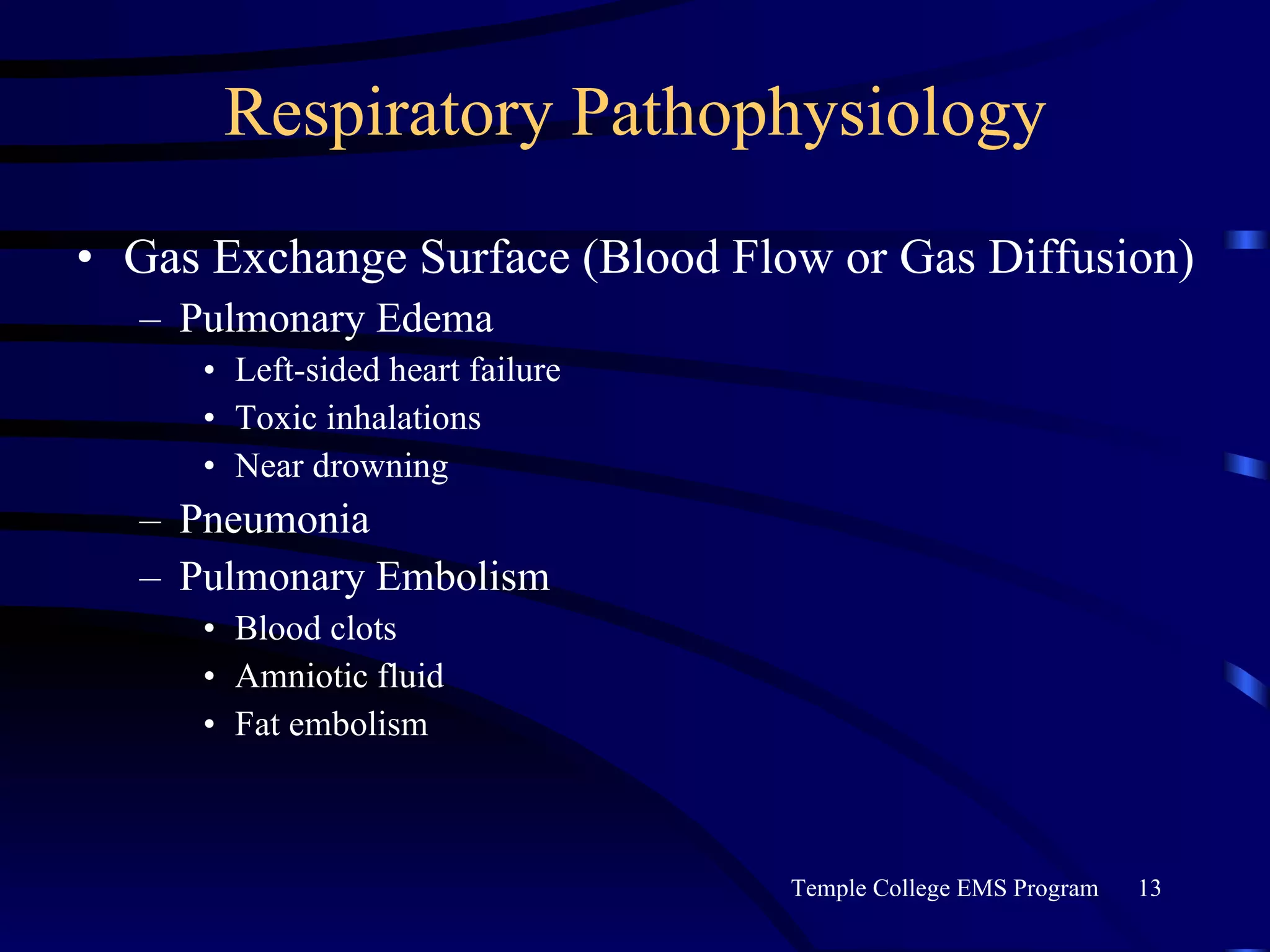
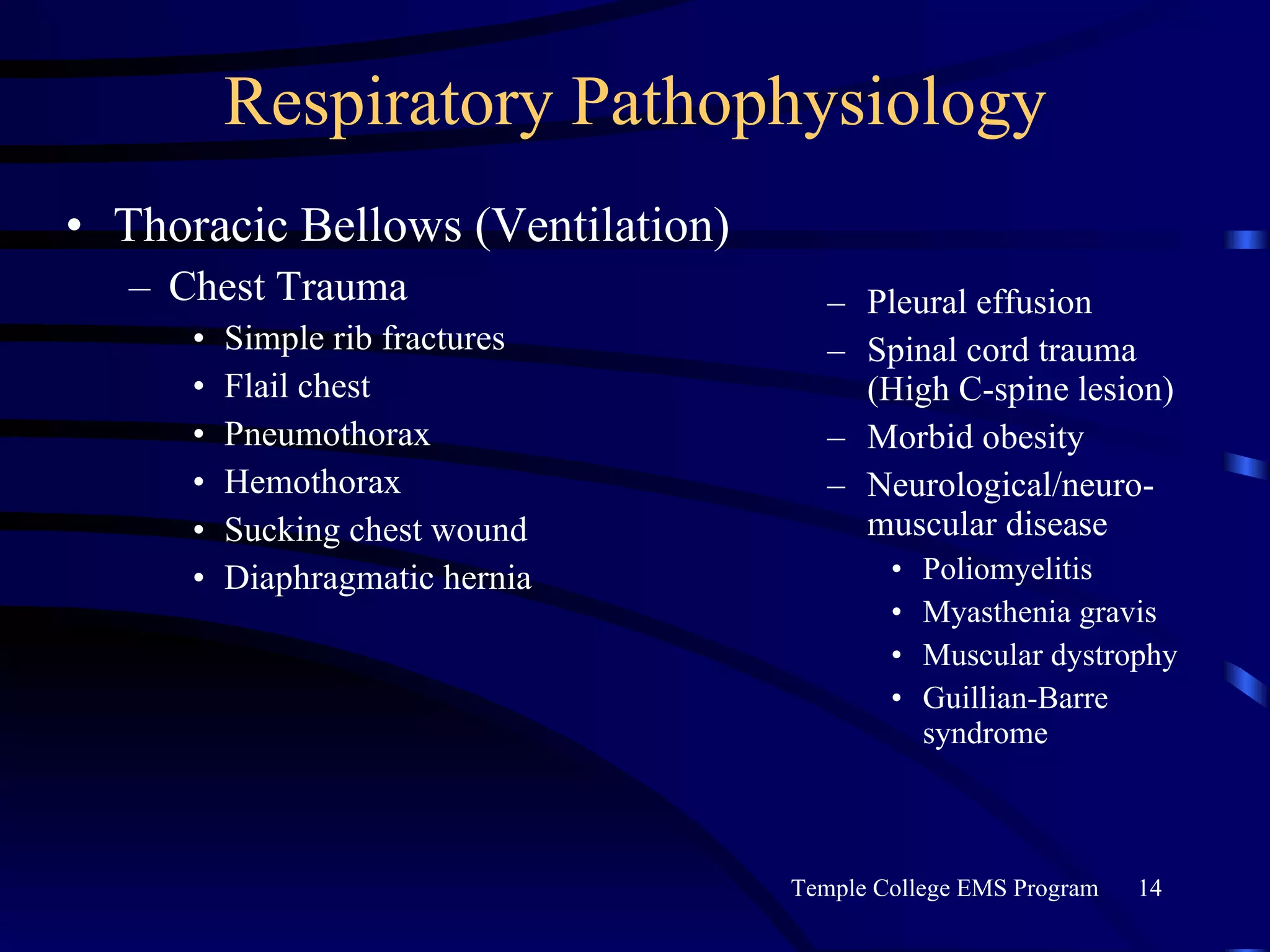
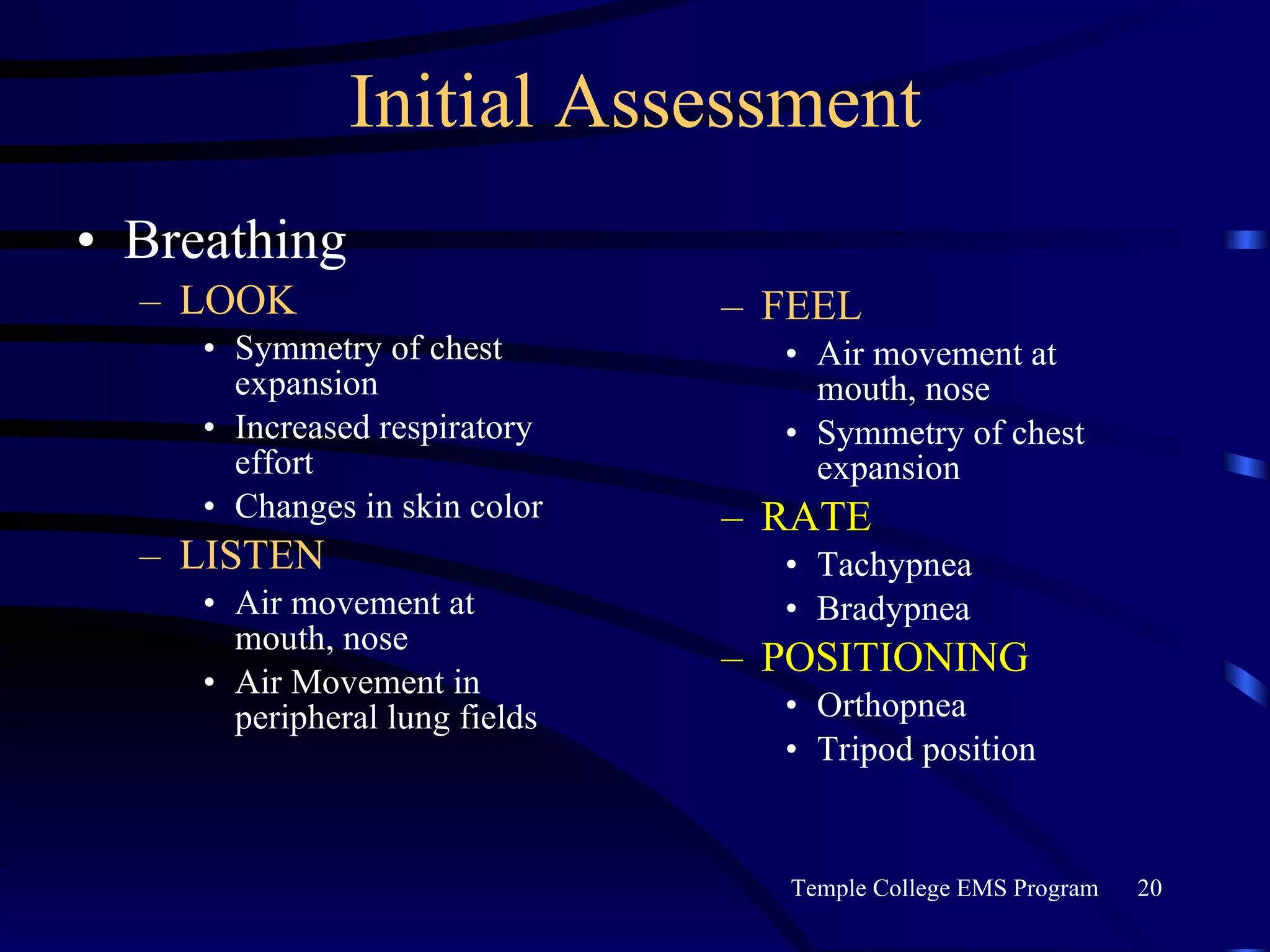
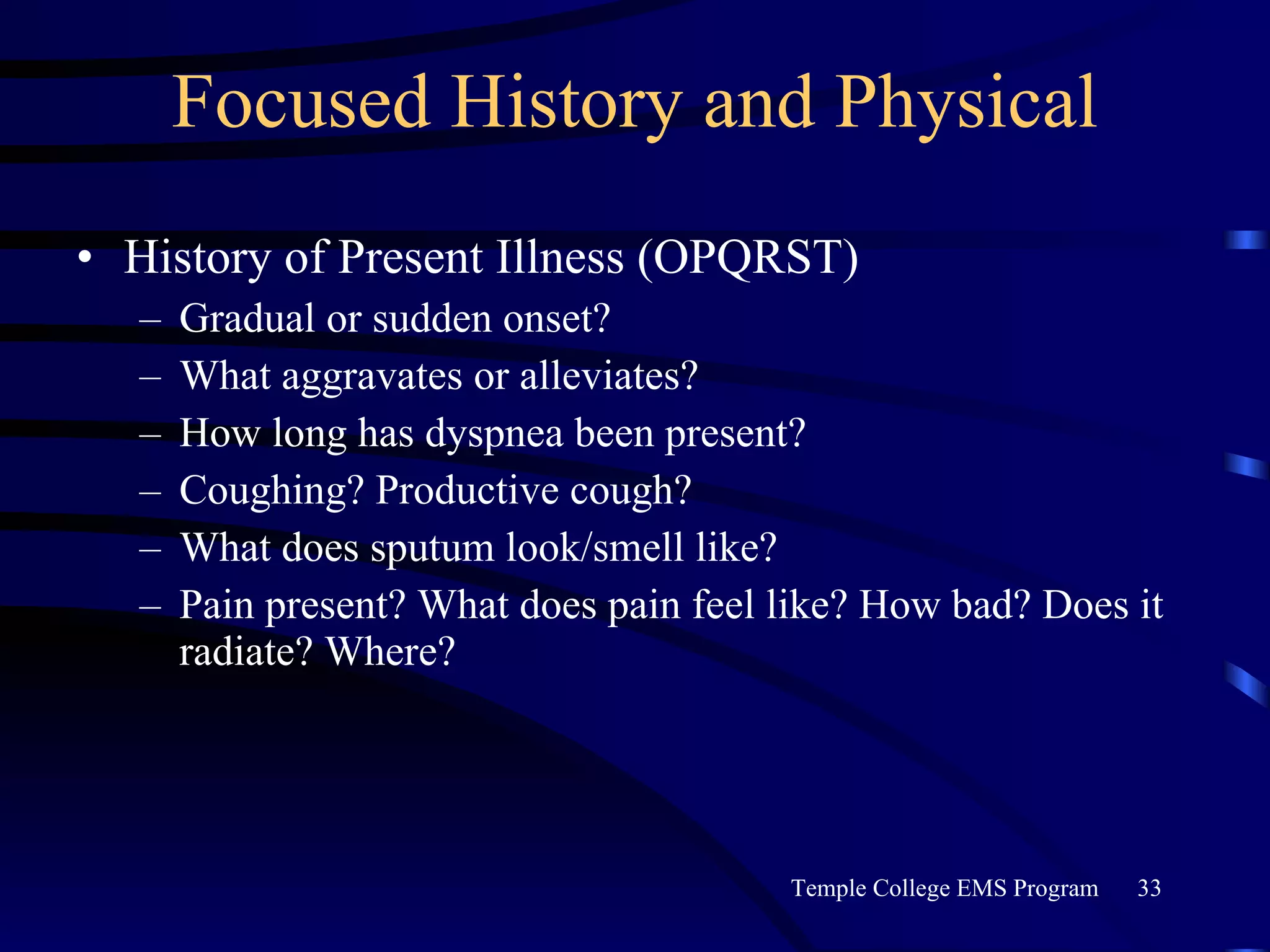
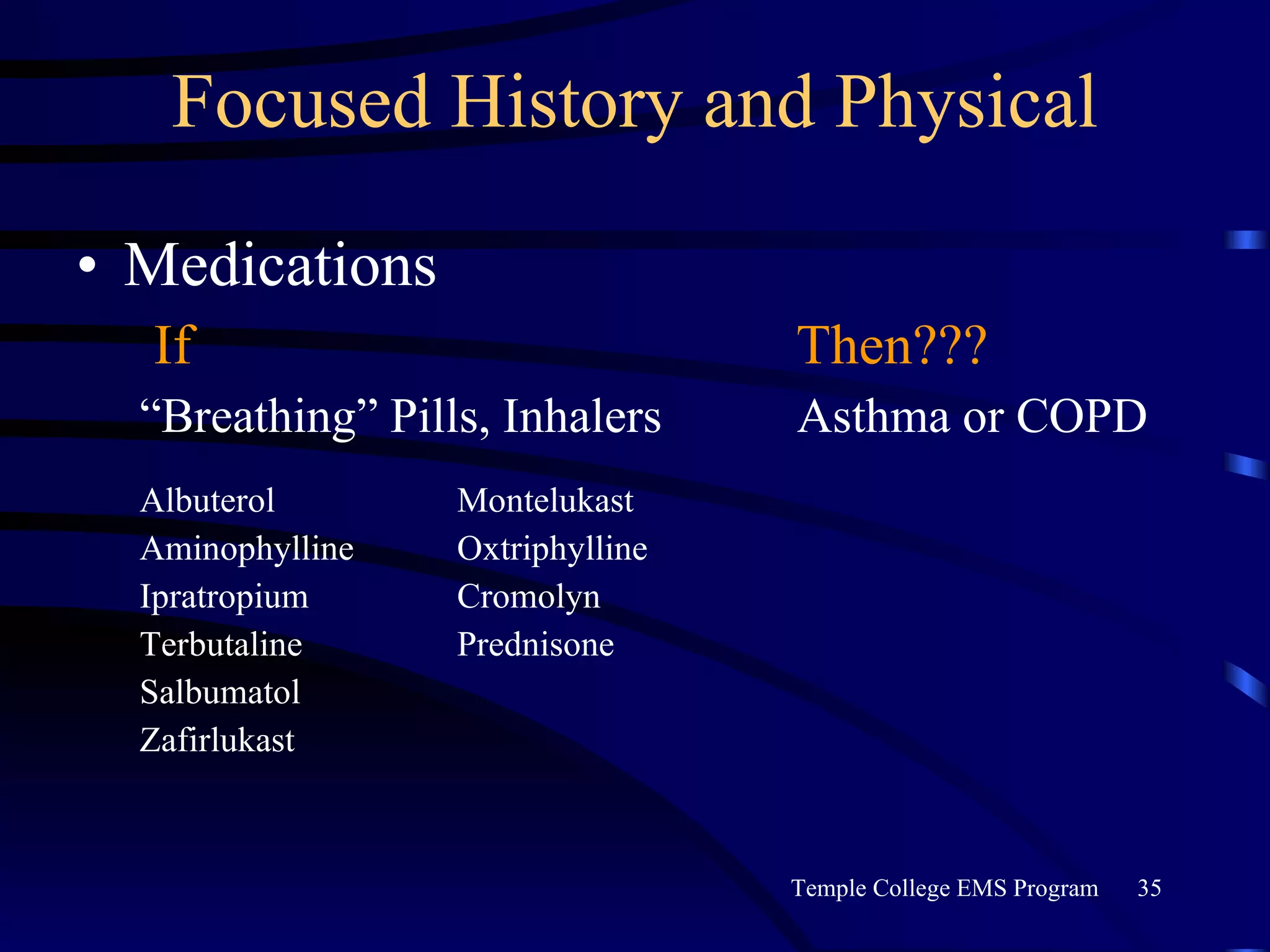
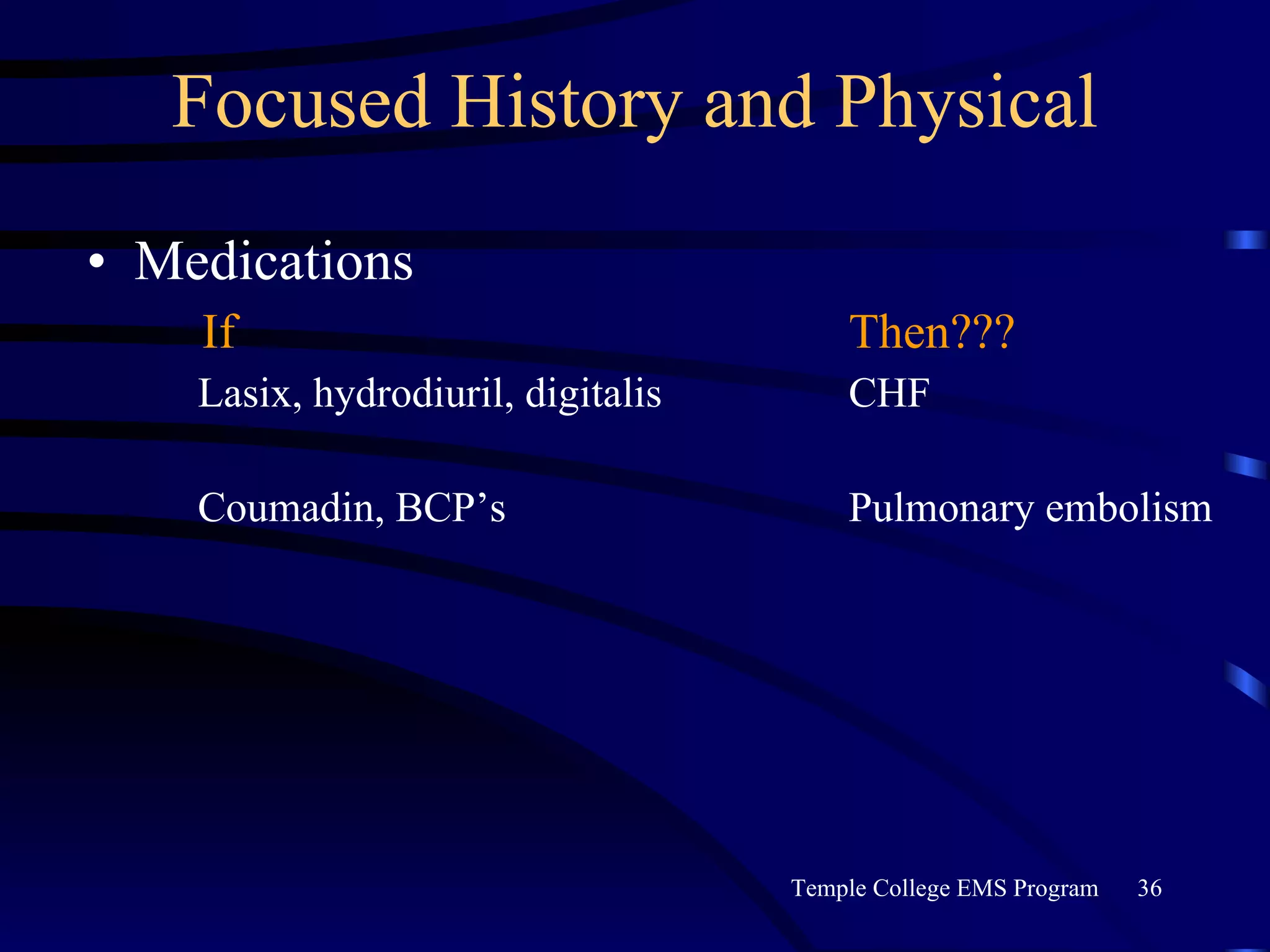
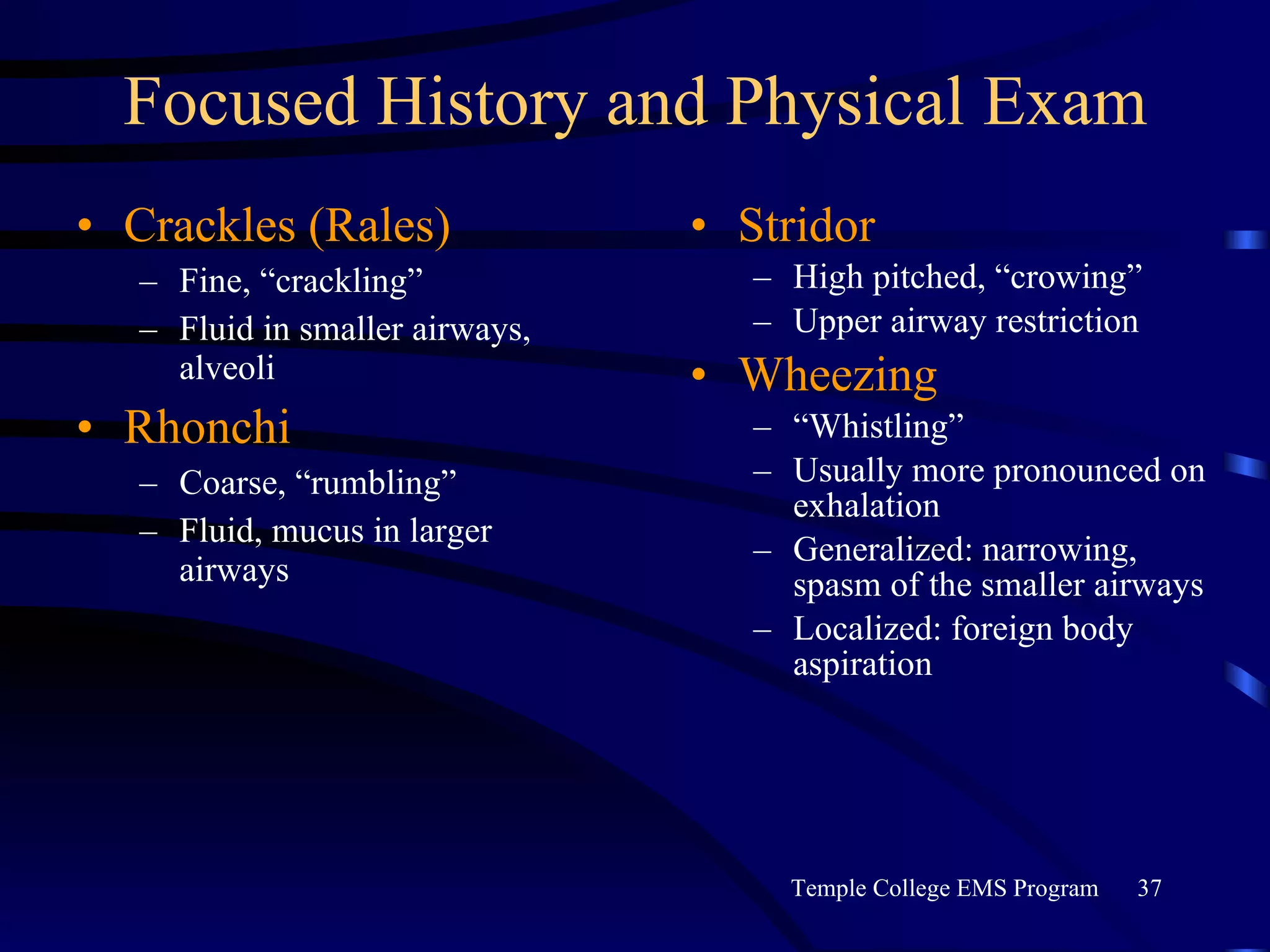
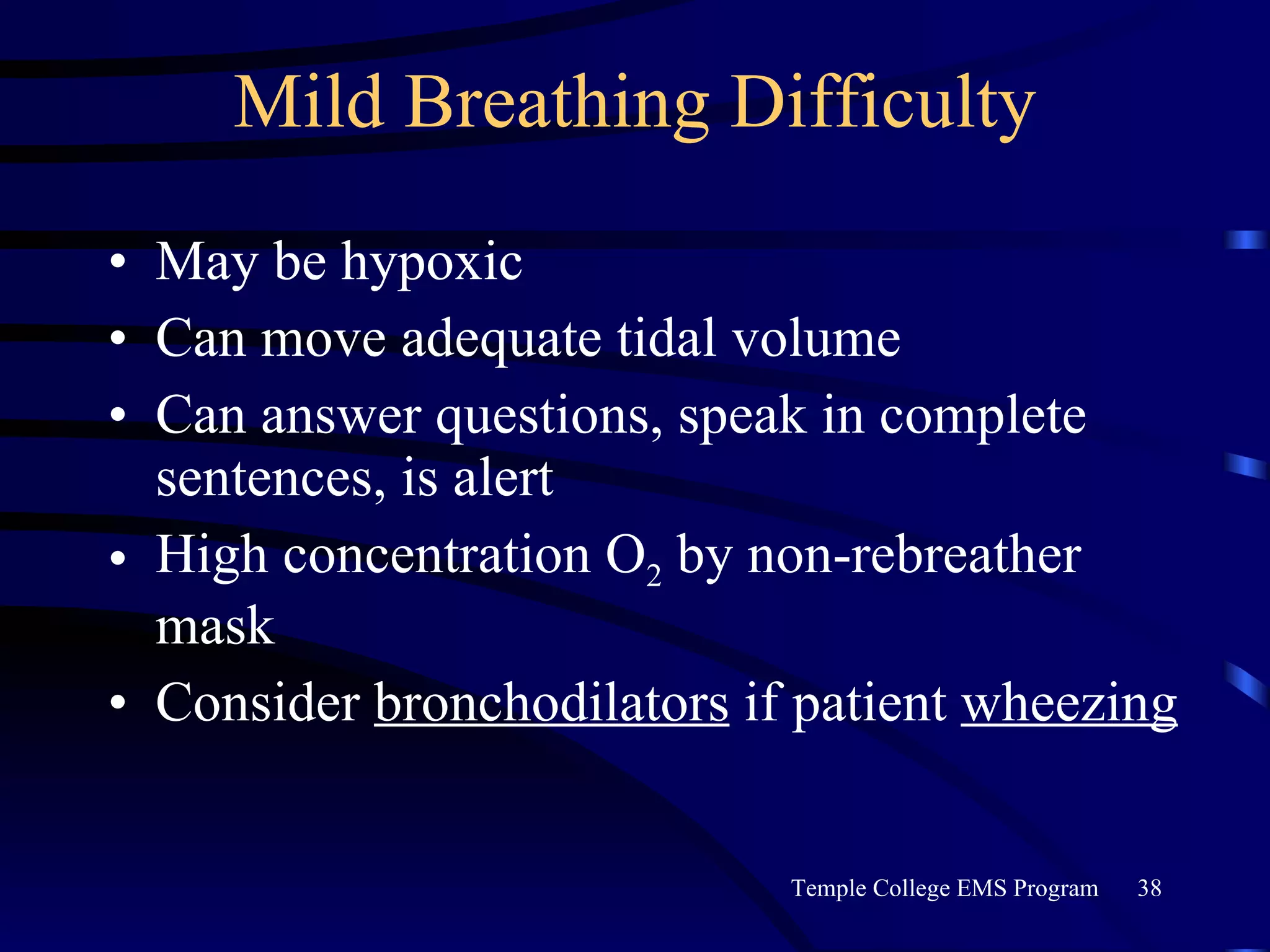
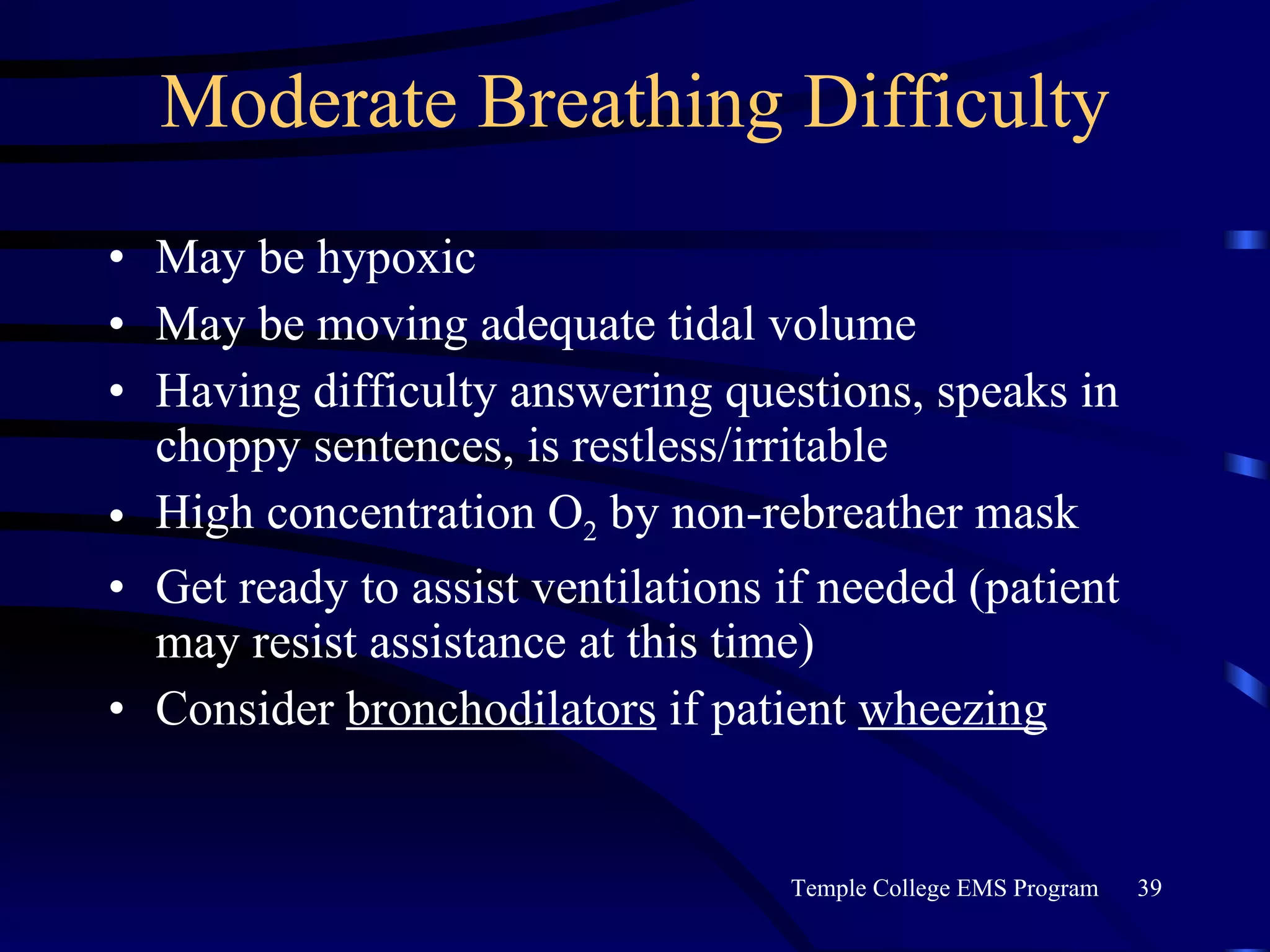
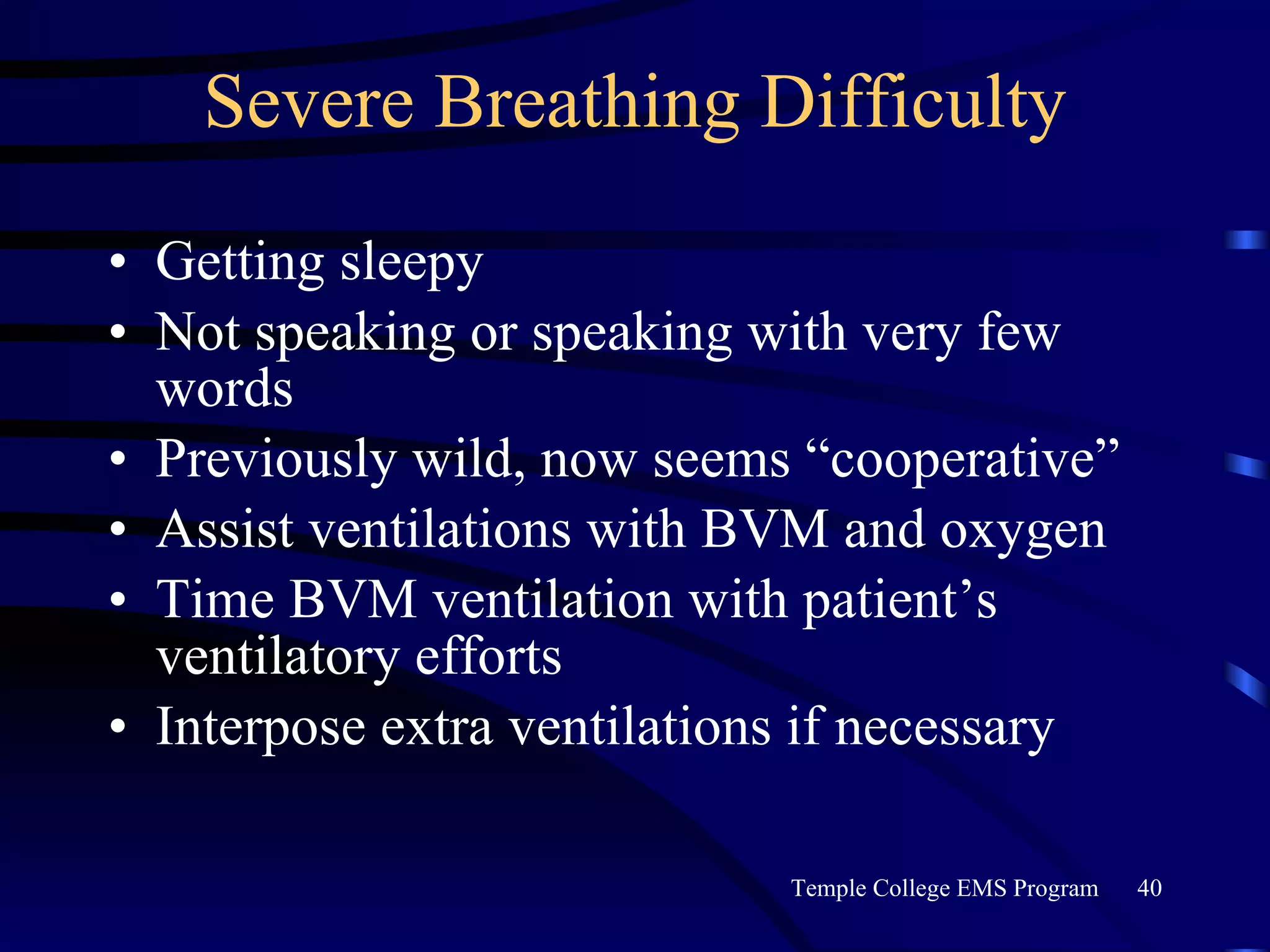
The document summarizes key aspects of the respiratory system for EMTs, including anatomy, physiology, assessment, and initial management of respiratory emergencies. It describes the respiratory system's purpose of gas exchange, relevant anatomy such as the lungs and airways, normal physiology of breathing, common pathologies affecting ventilation and gas exchange, and the ABCDE approach to assessment and initial management of patients with respiratory distress or failure.