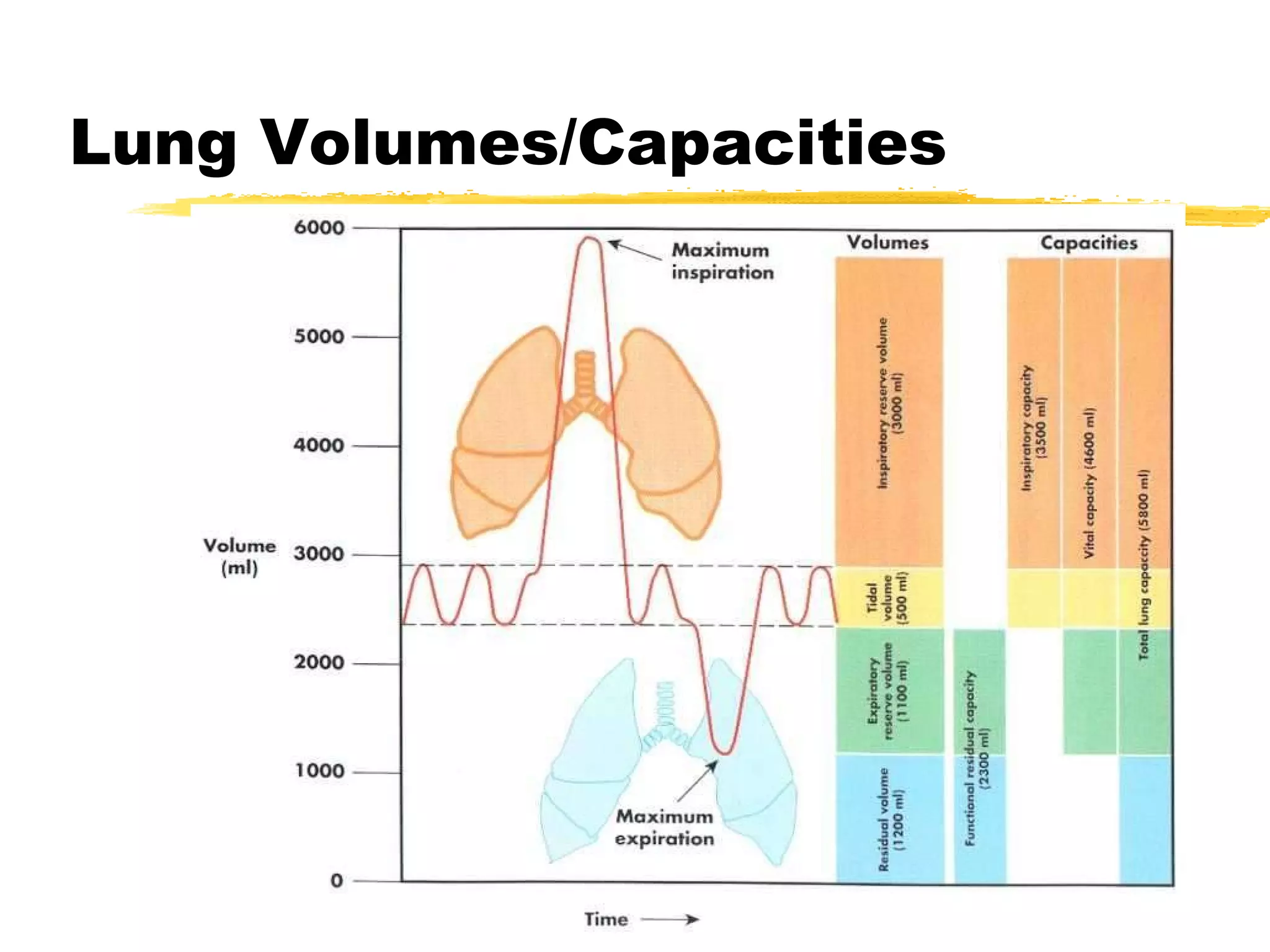
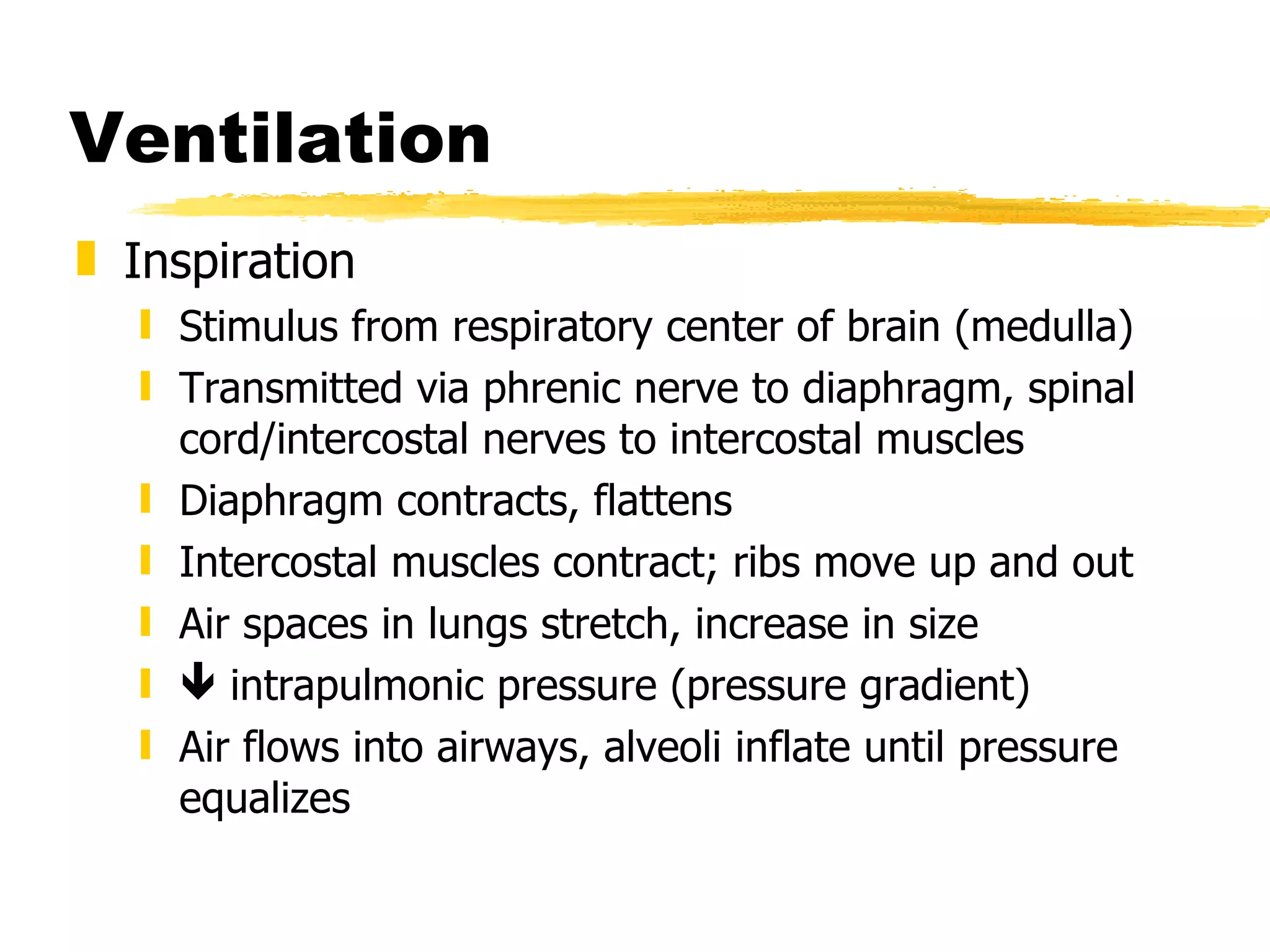
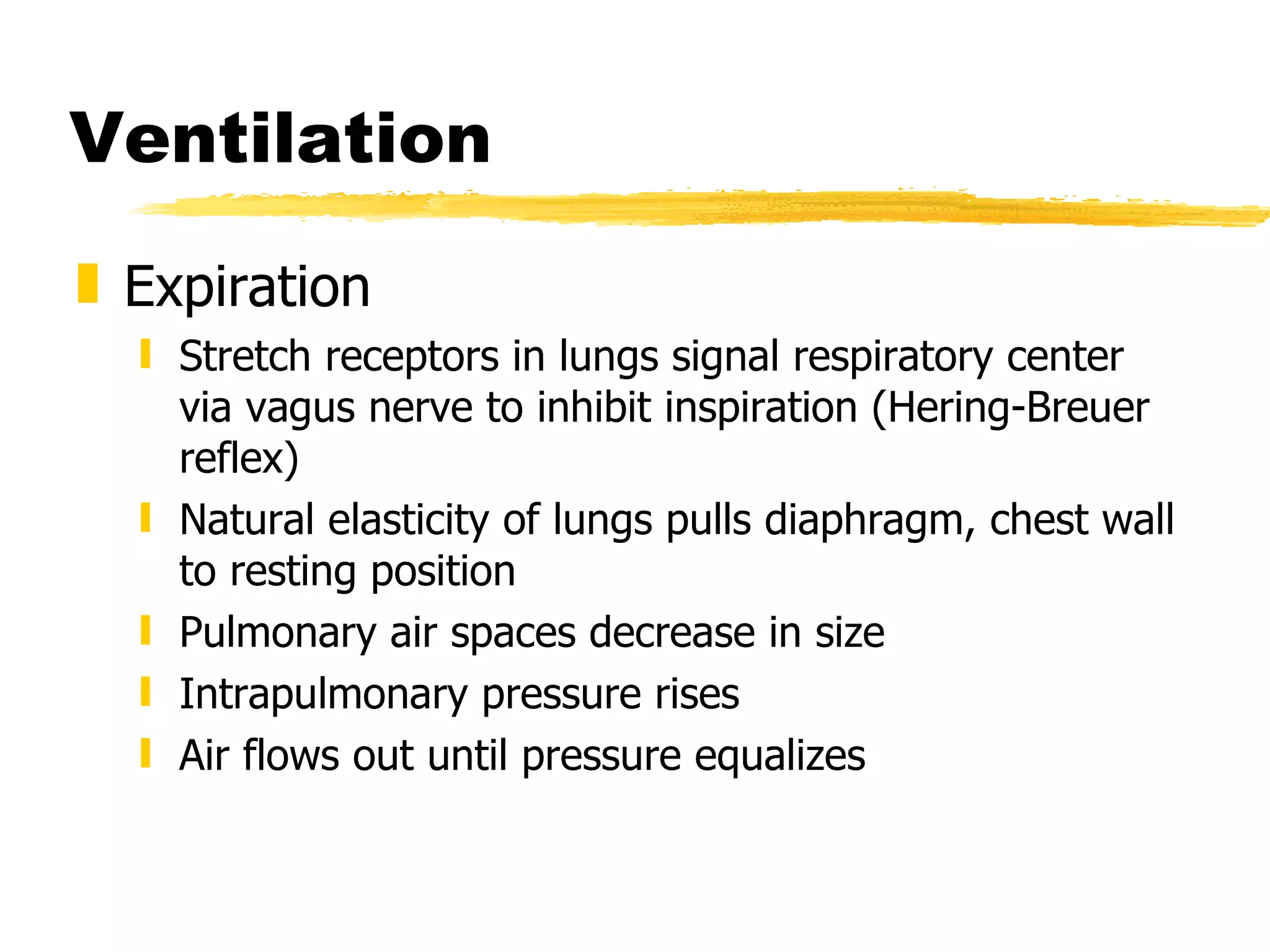
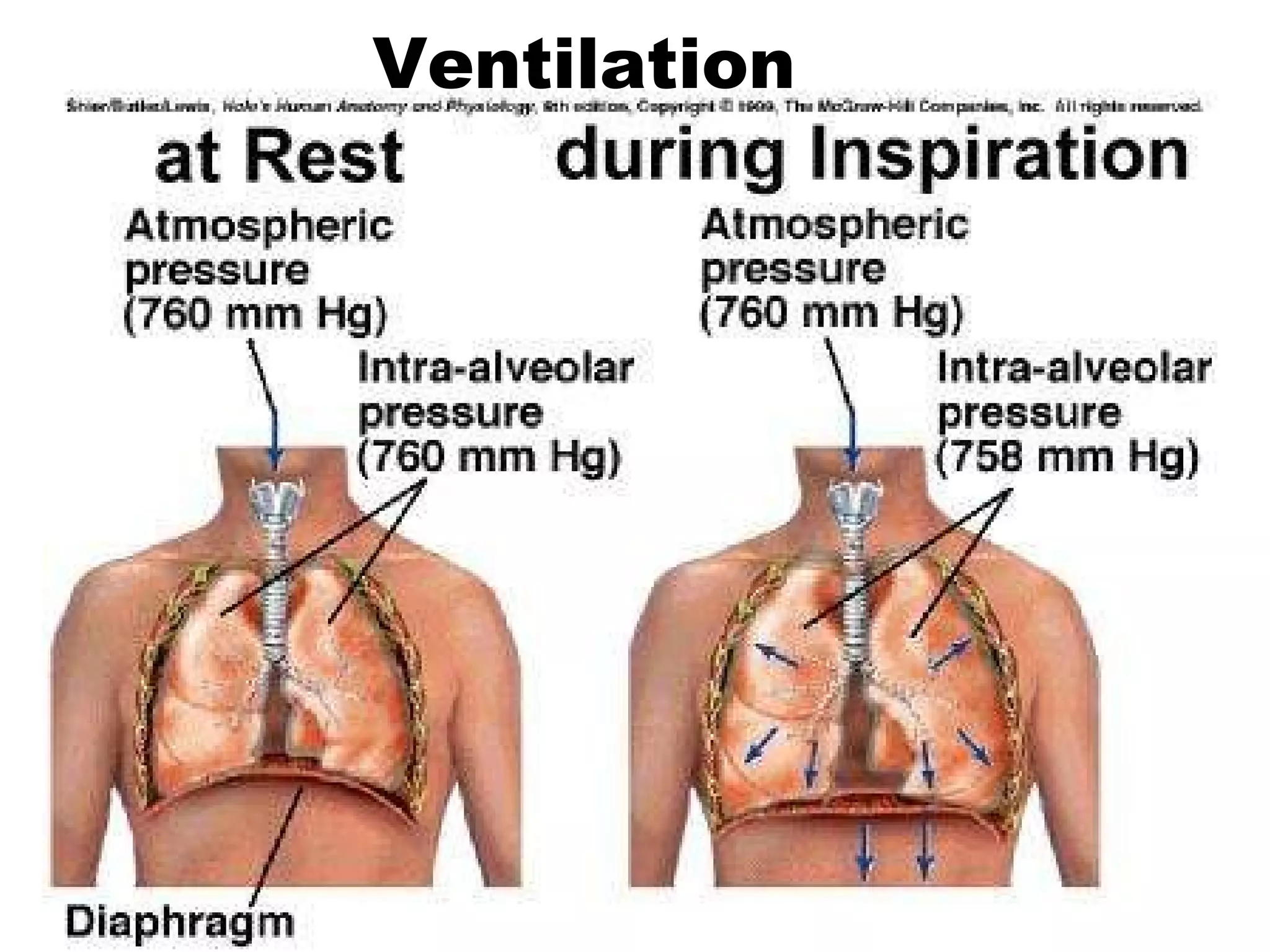
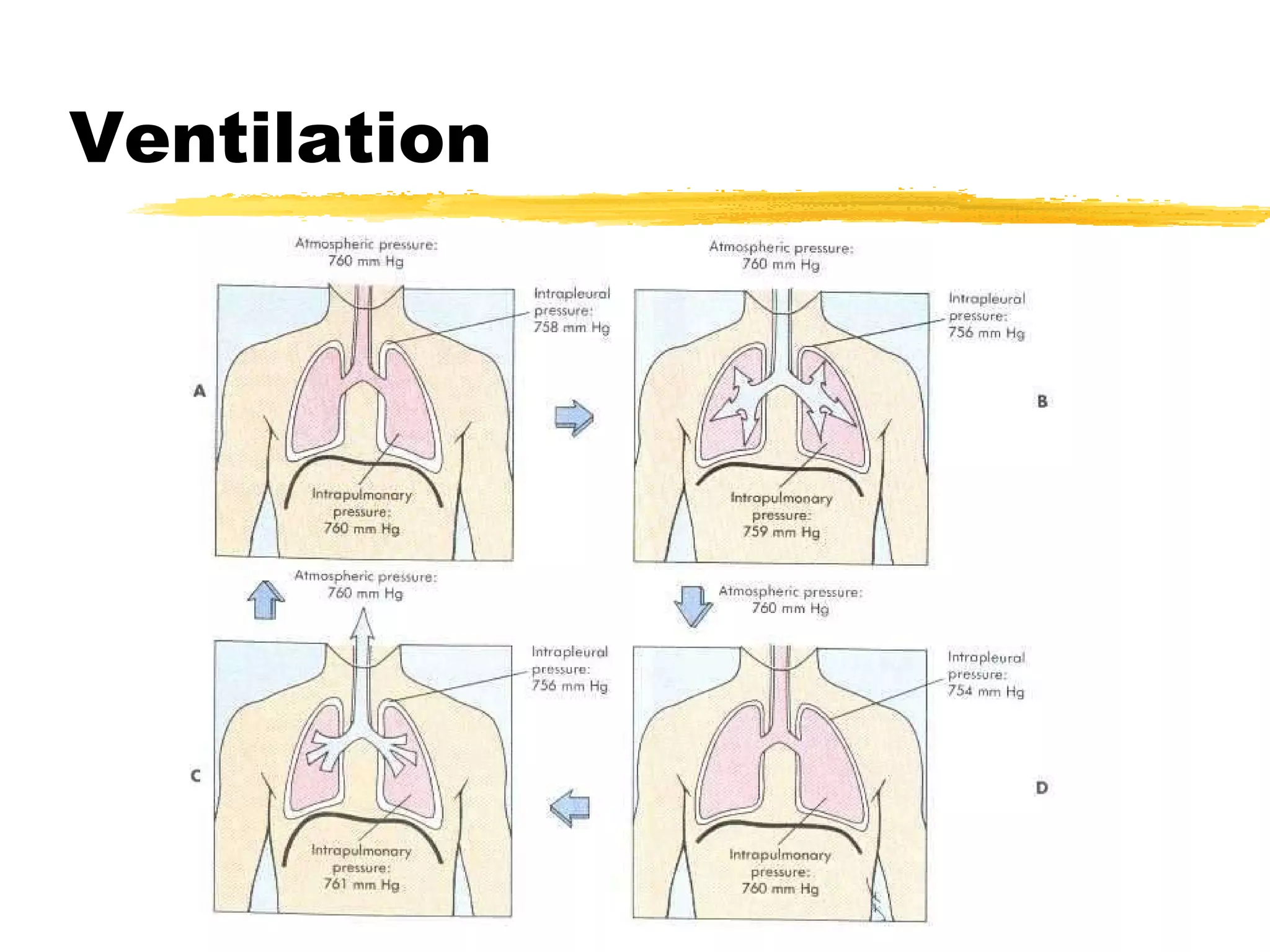
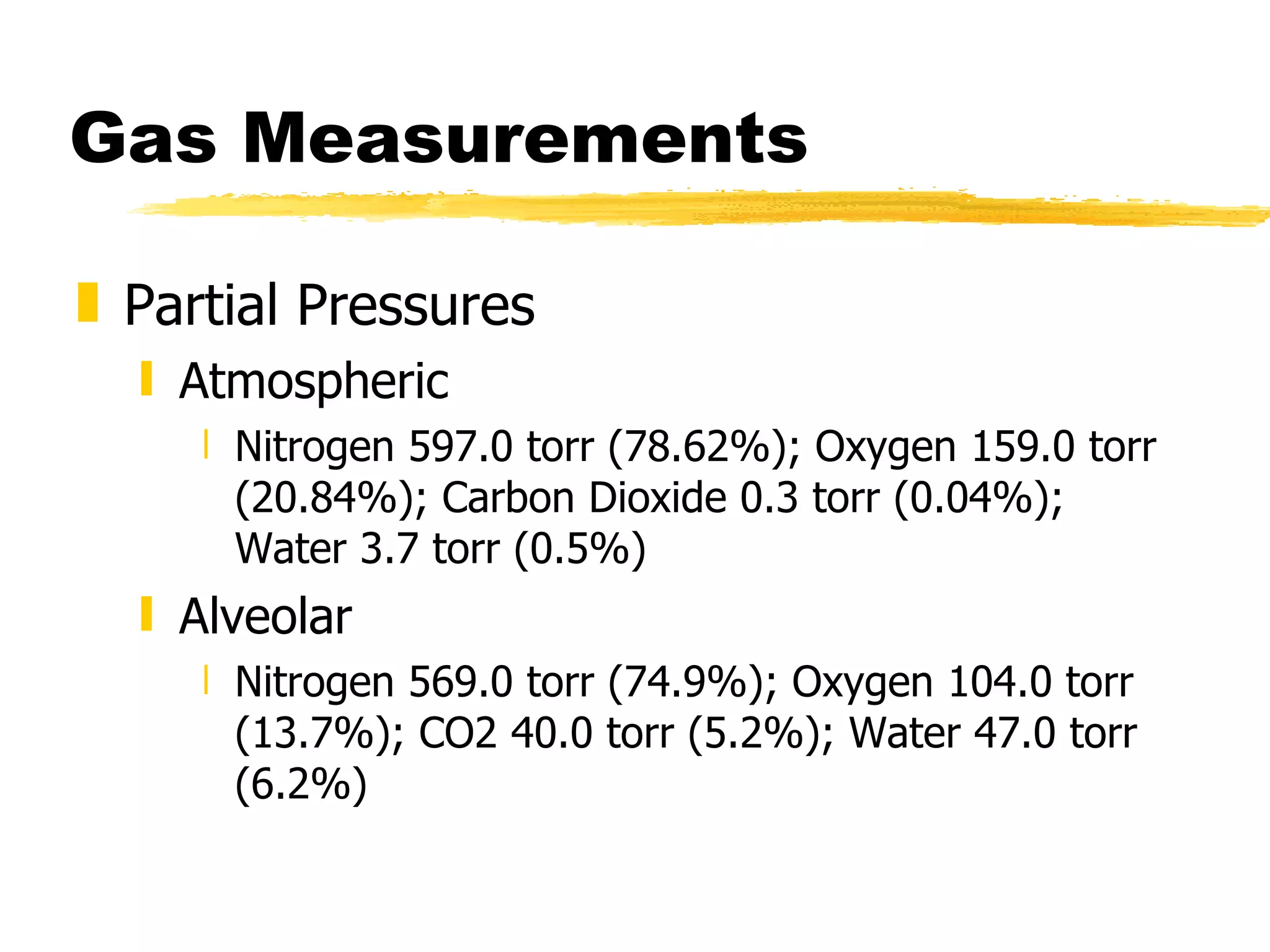
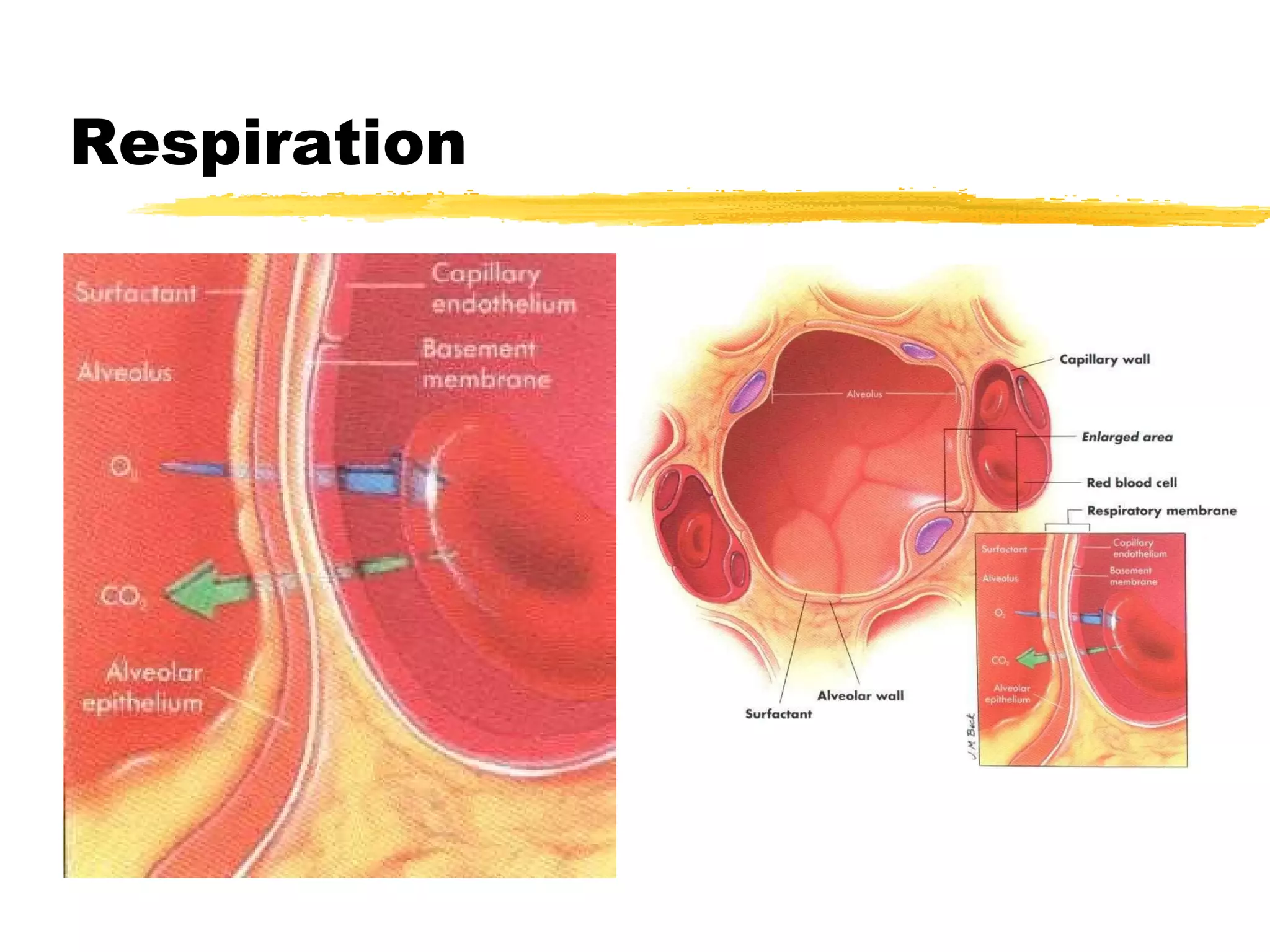
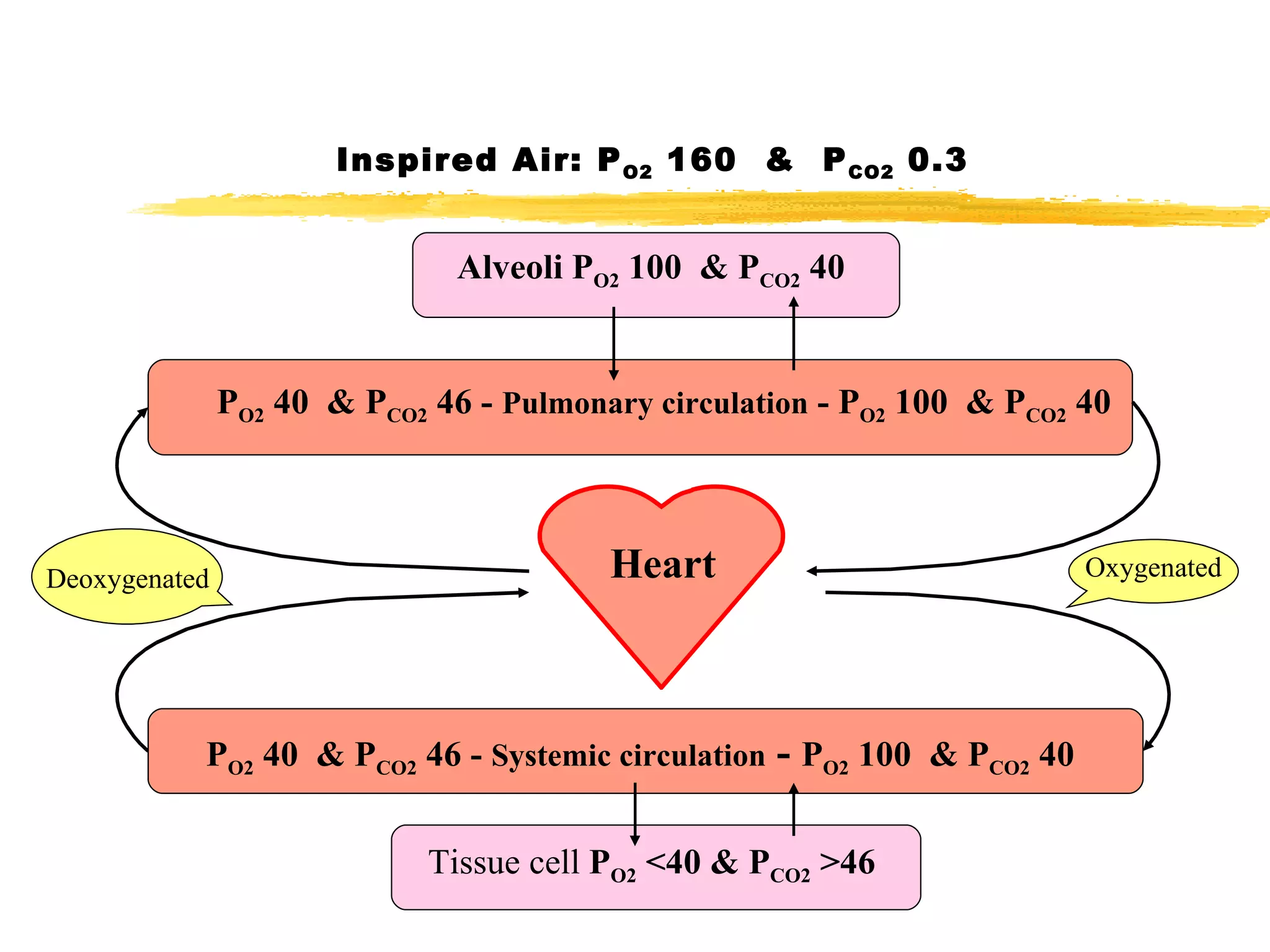
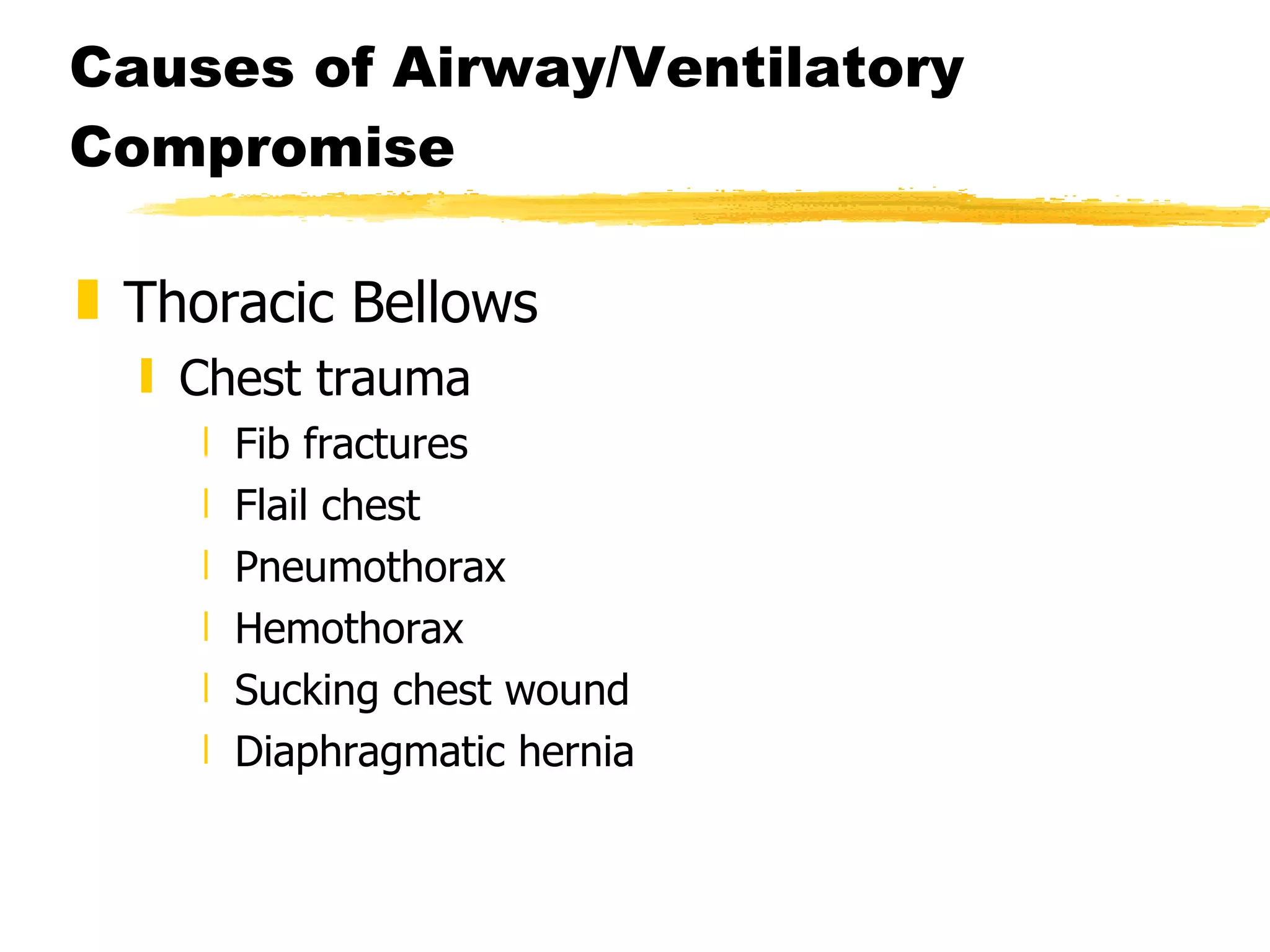
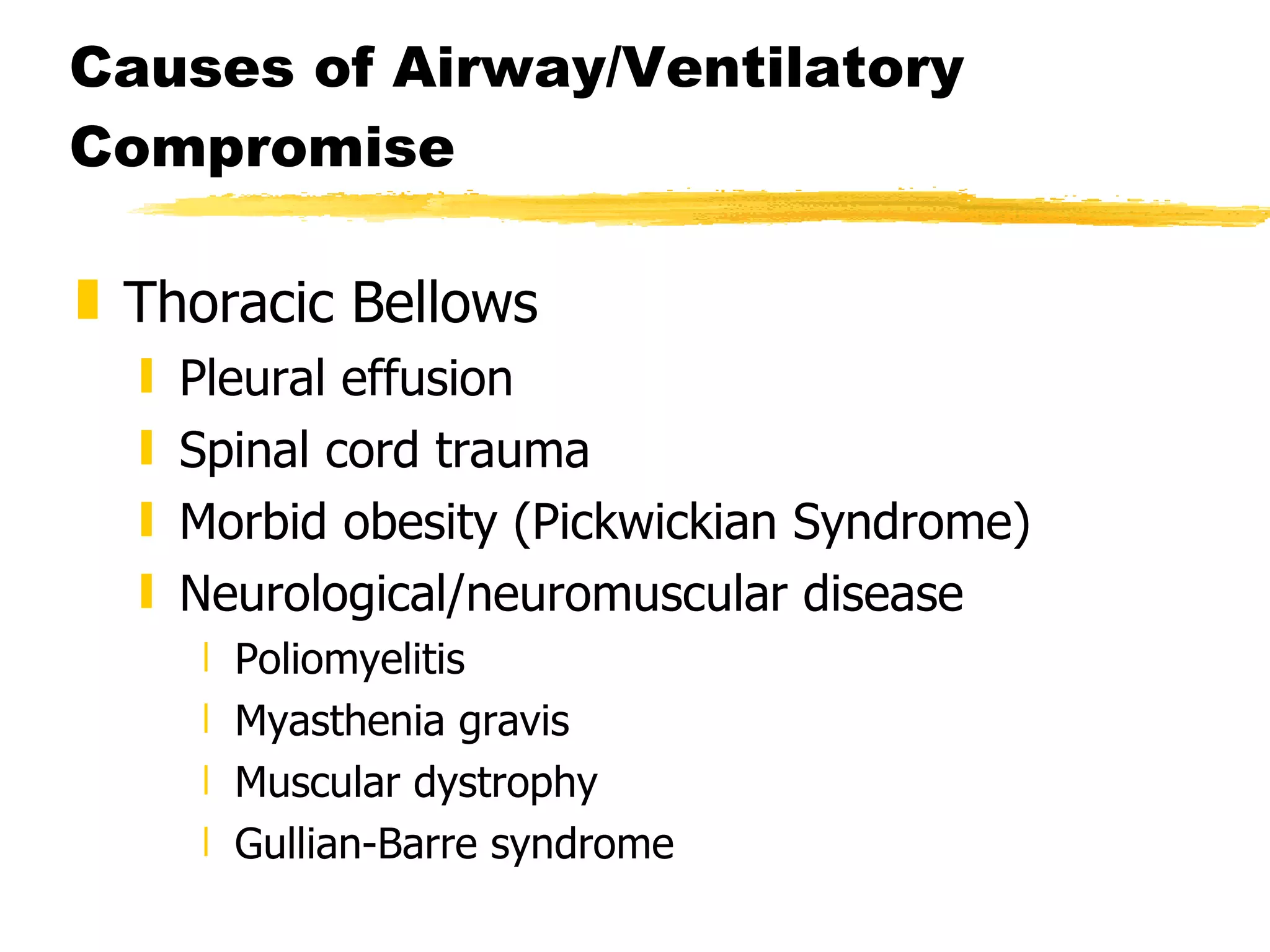
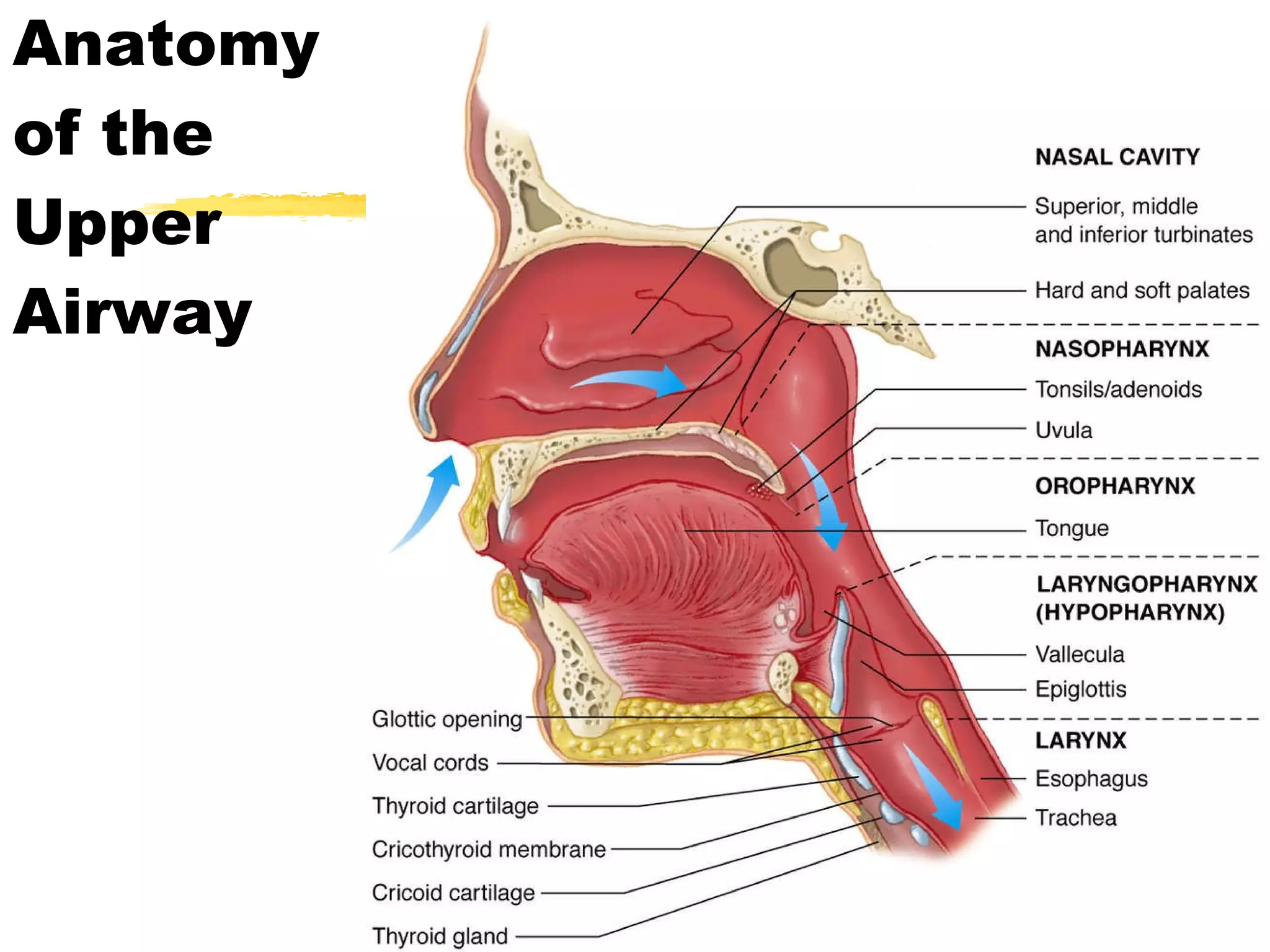
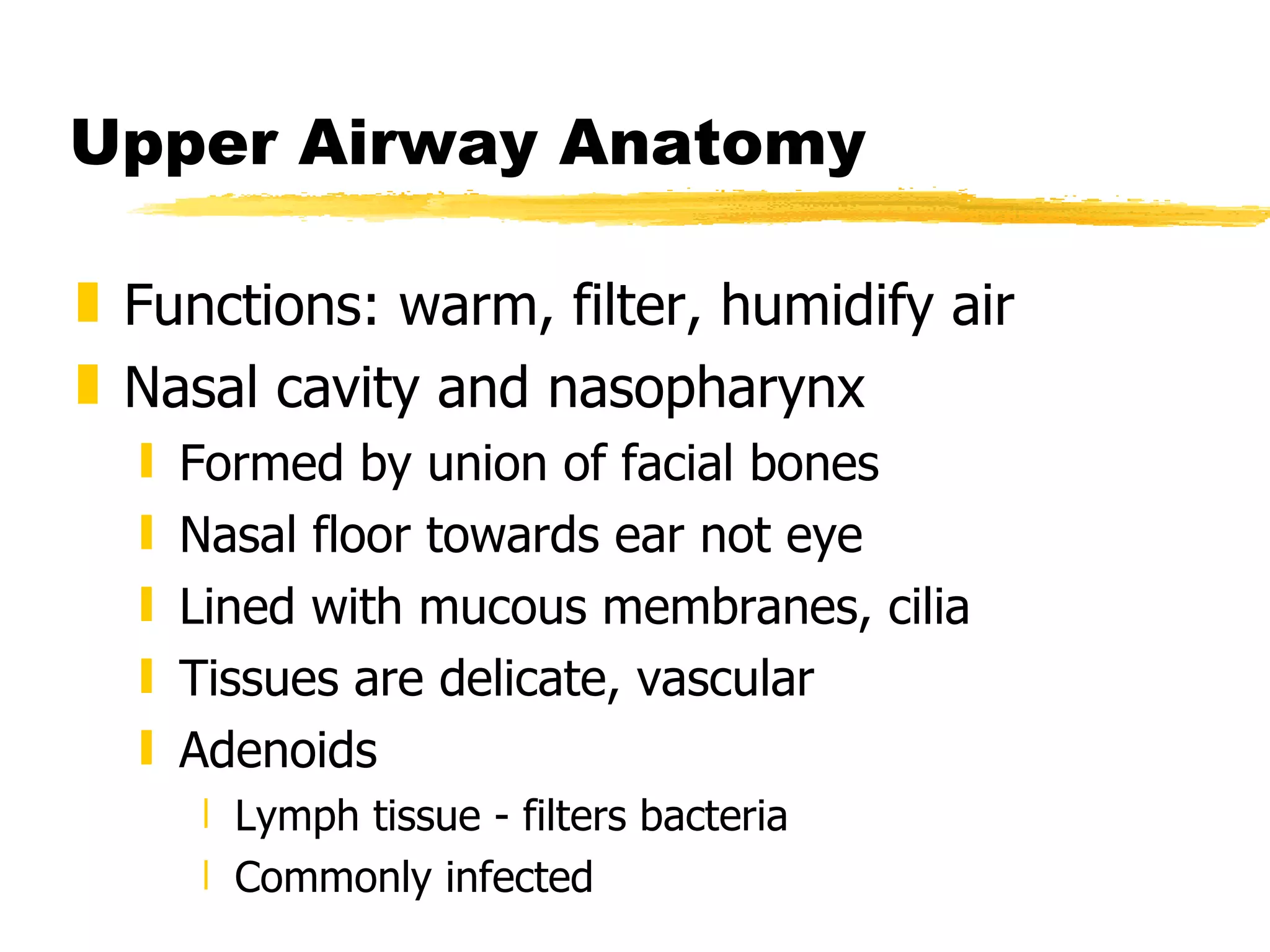
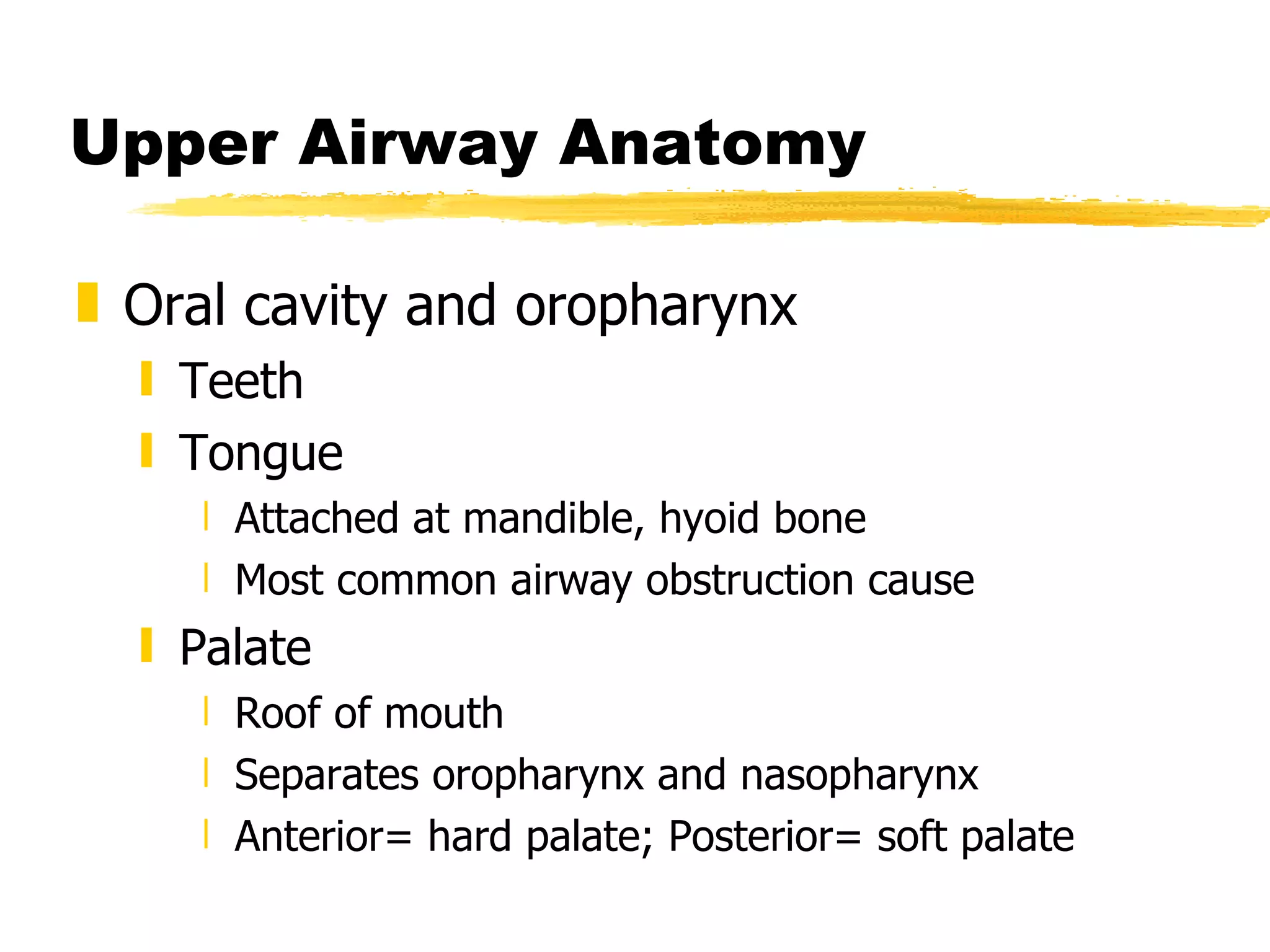
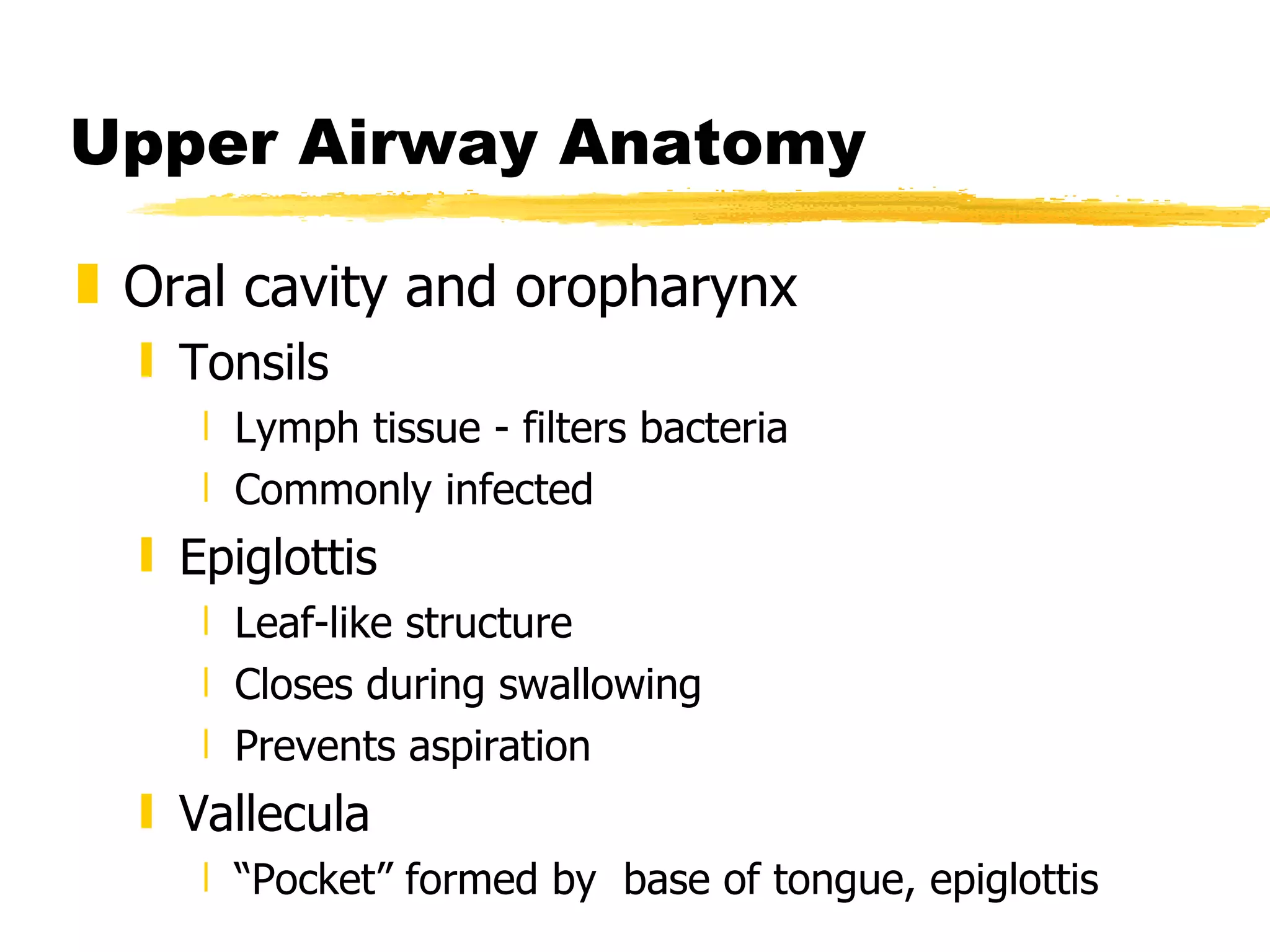
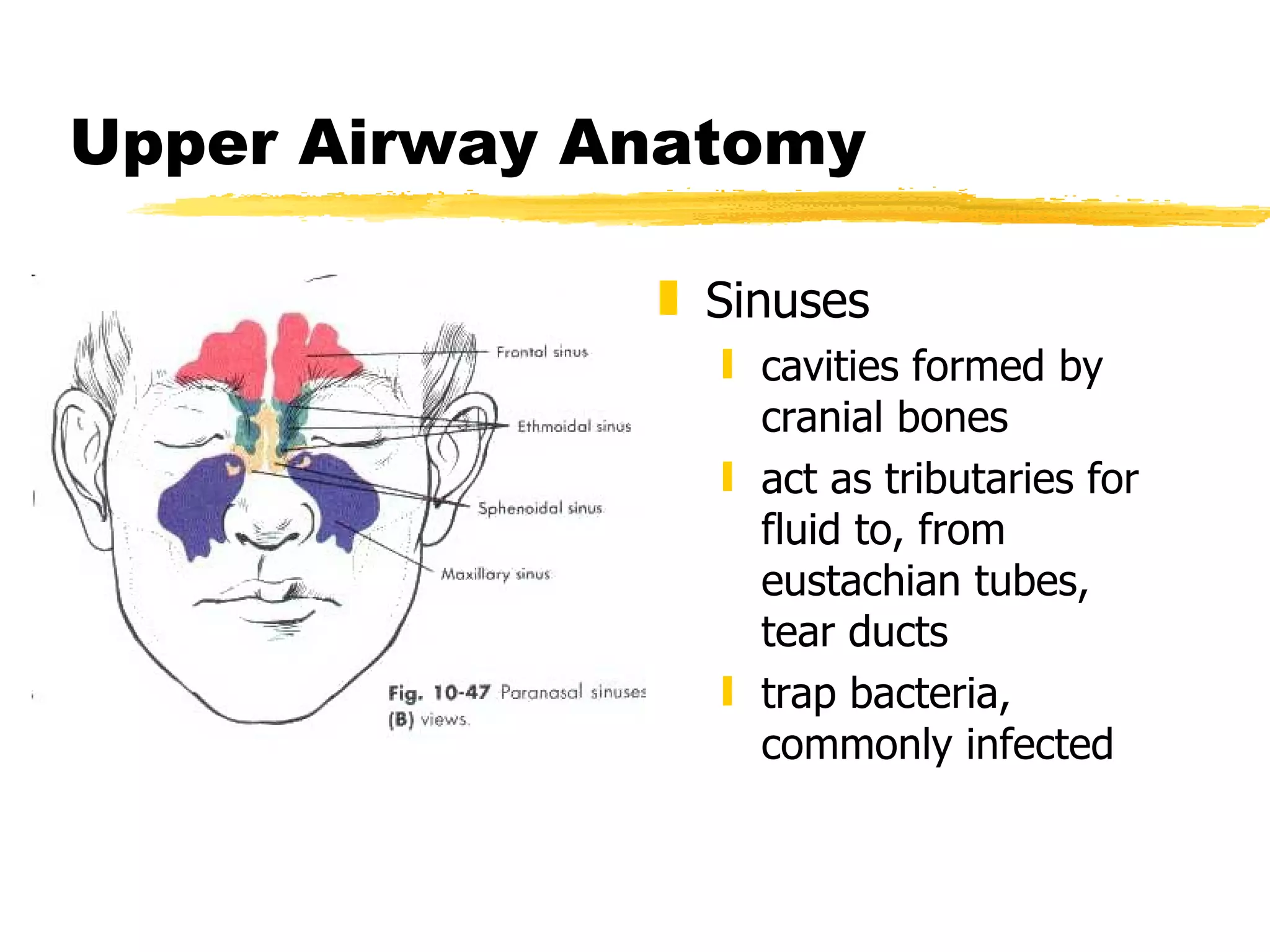
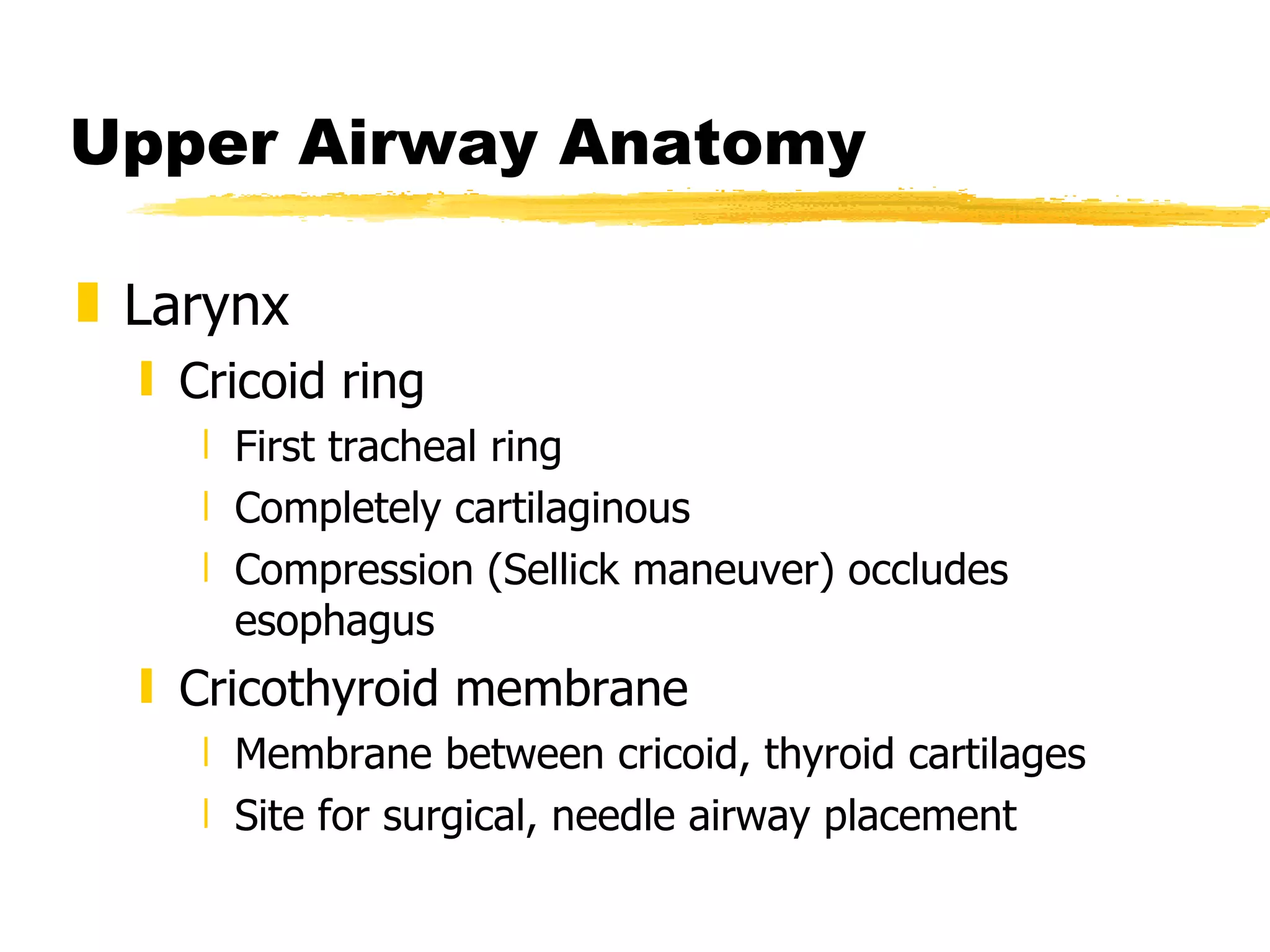
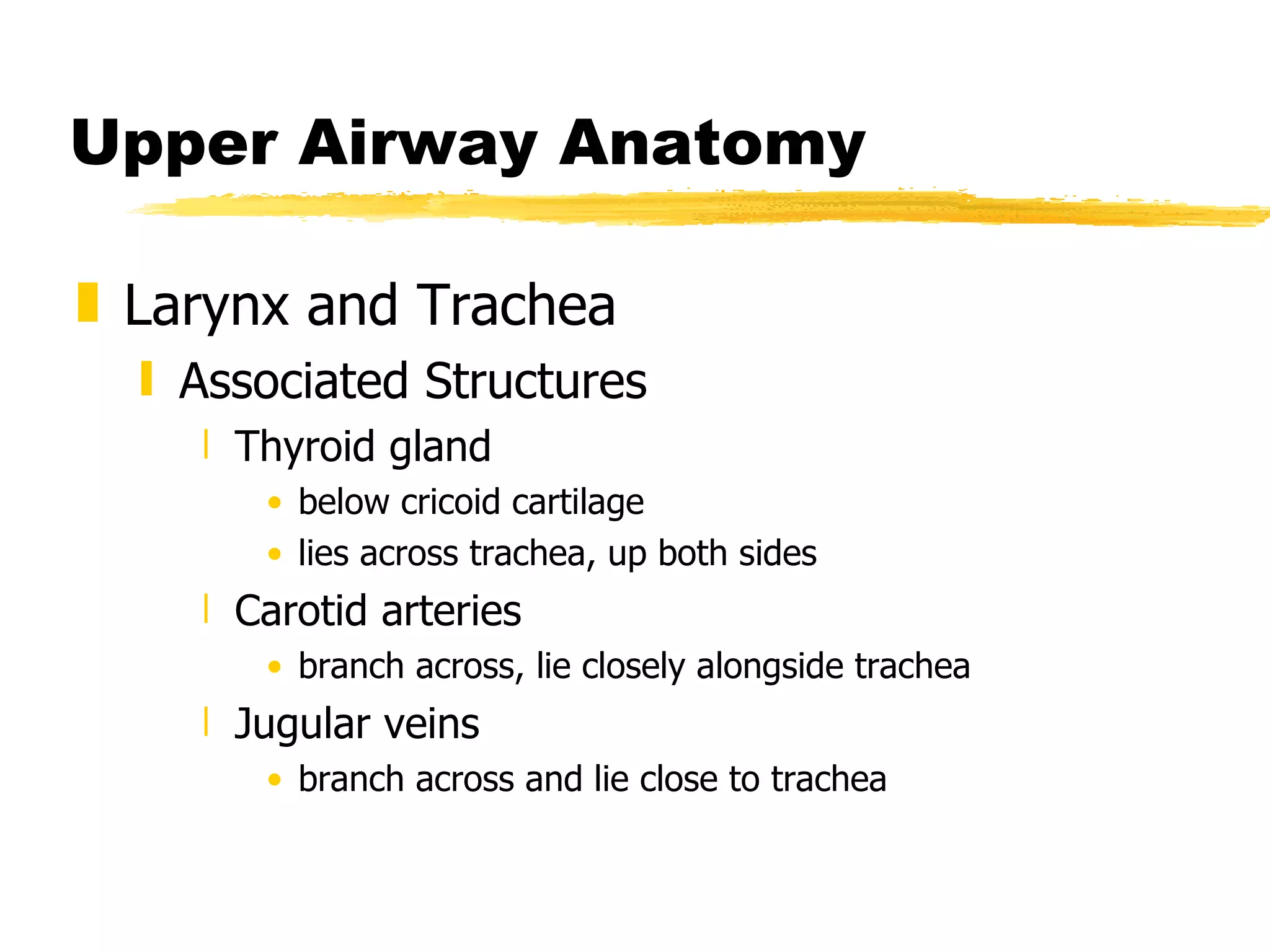
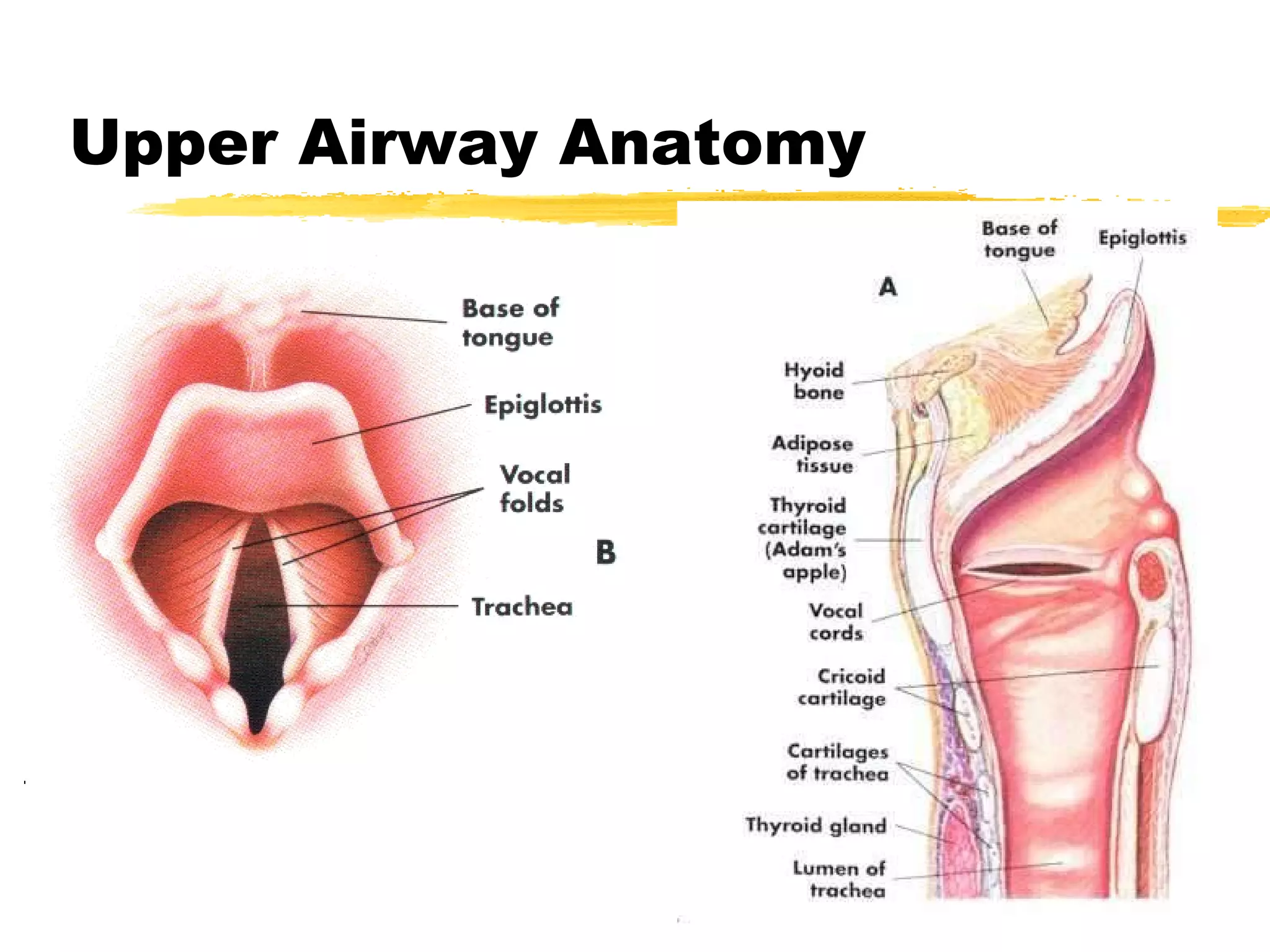
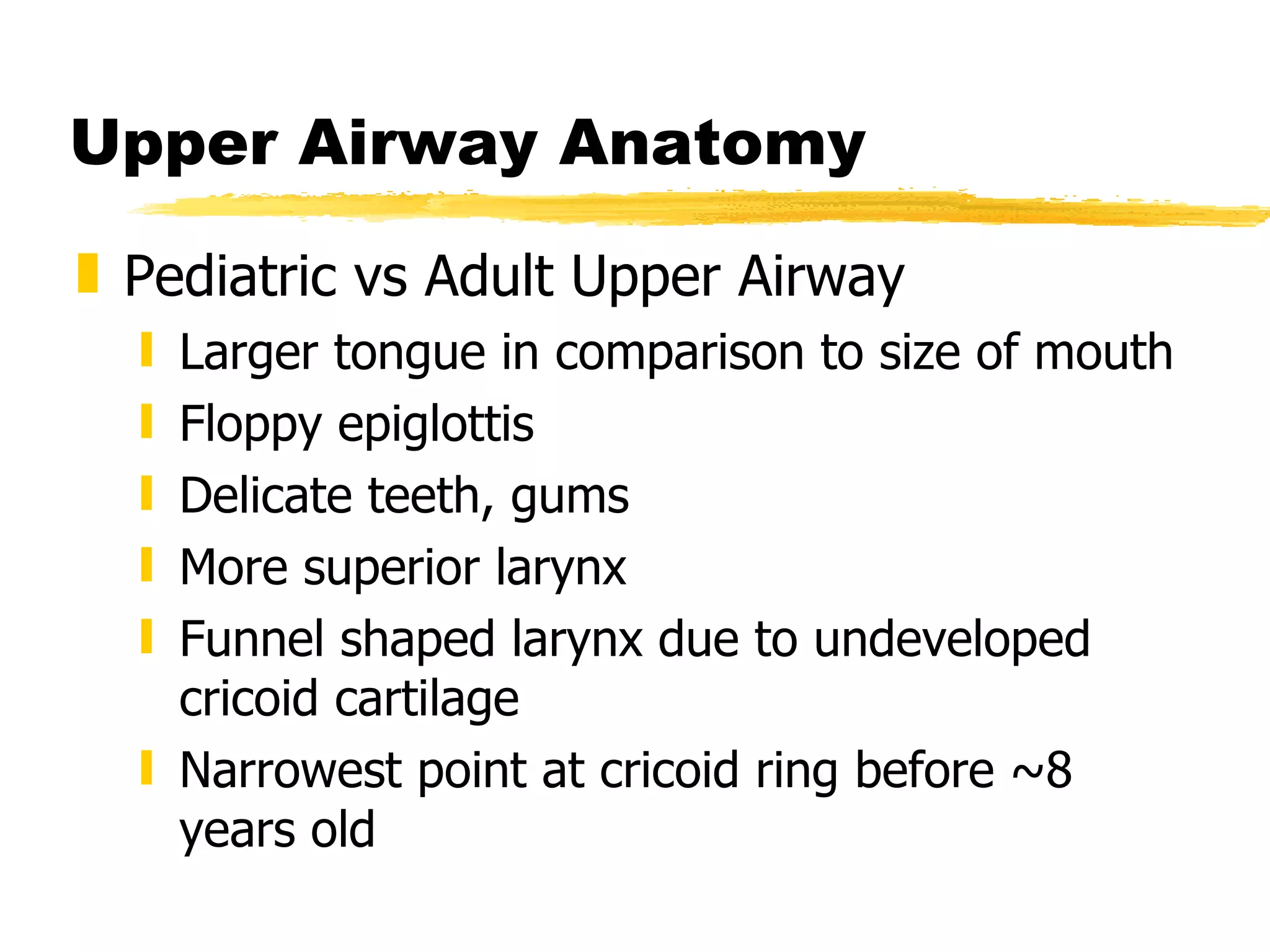
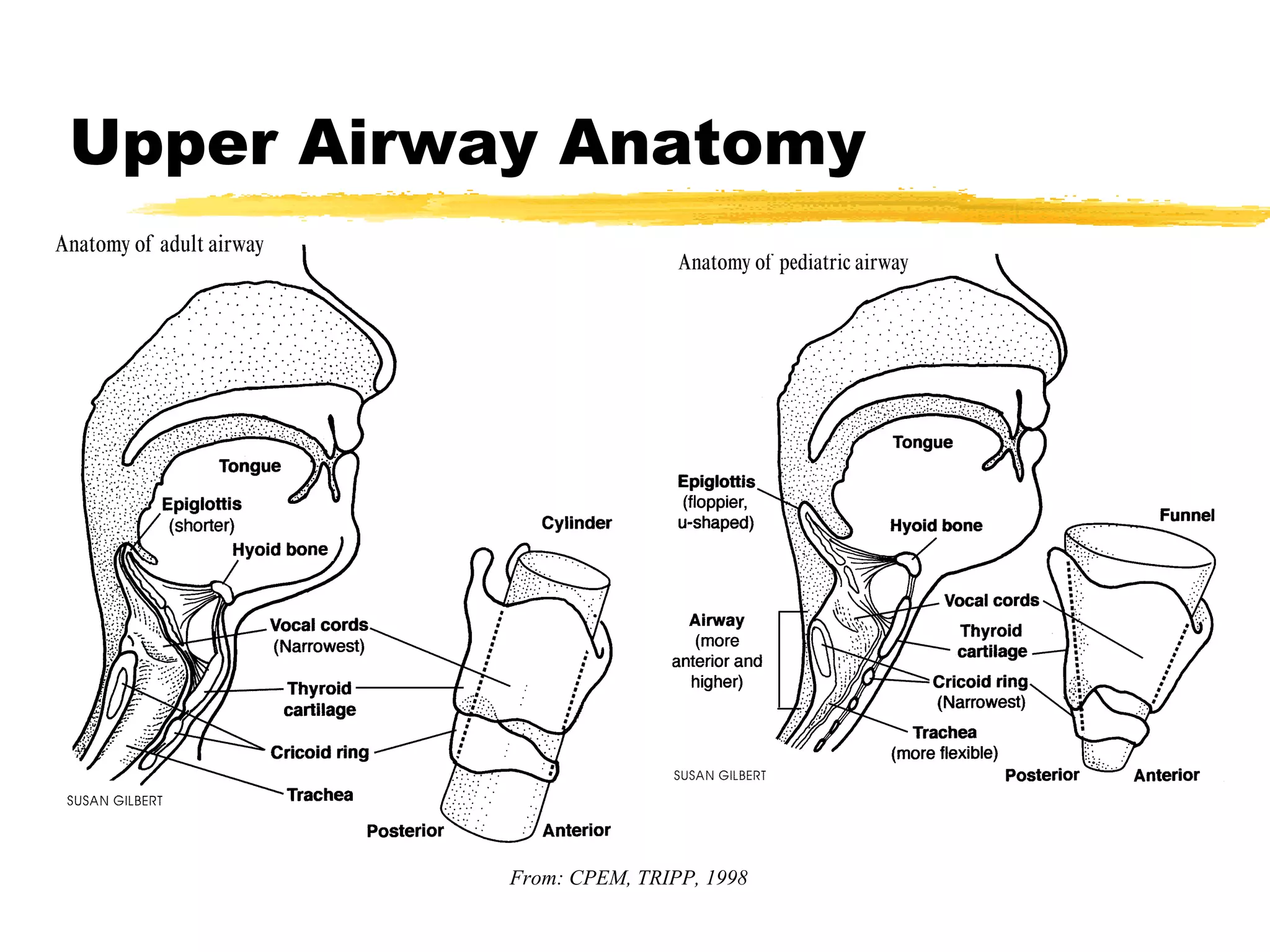
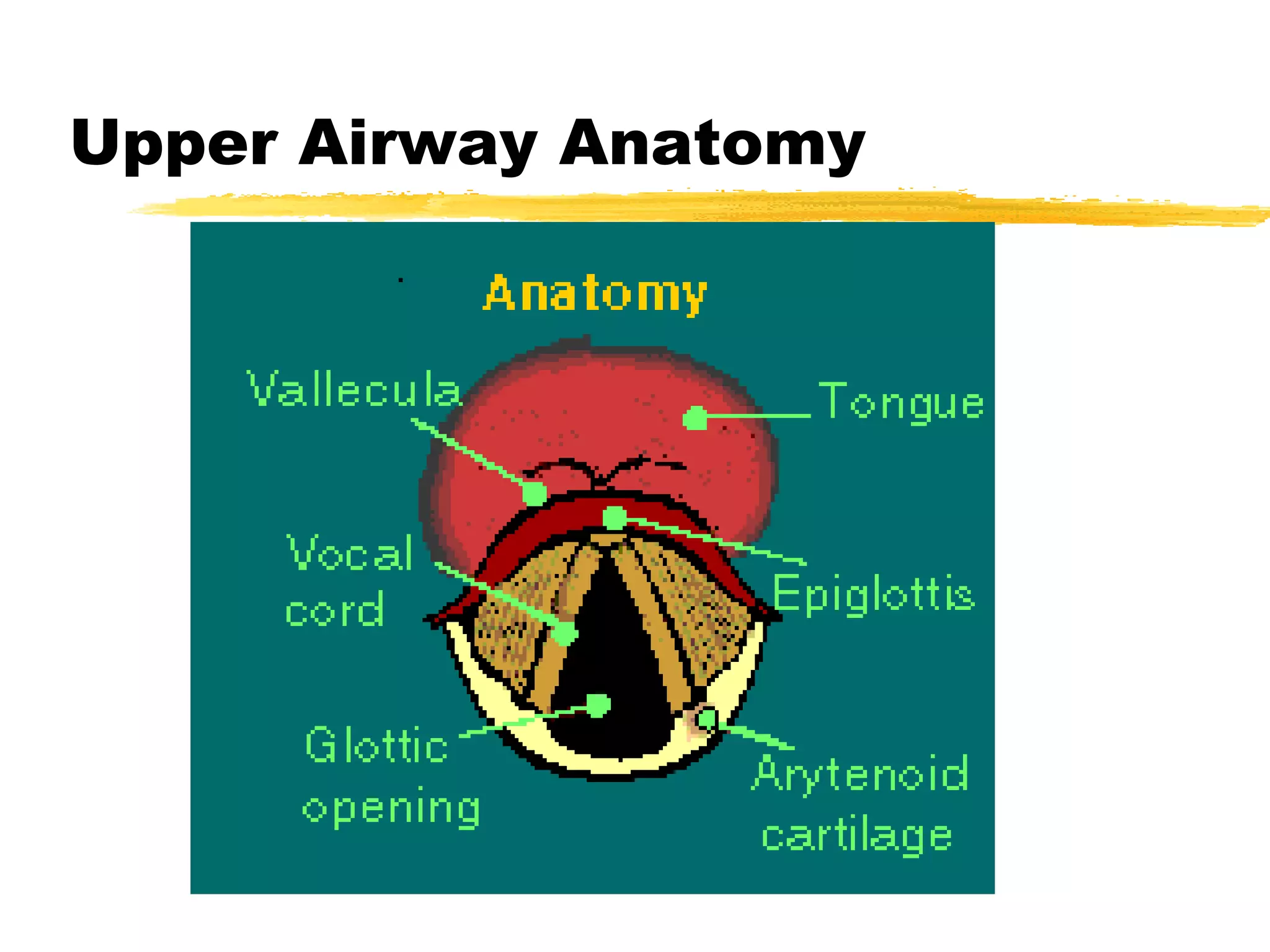
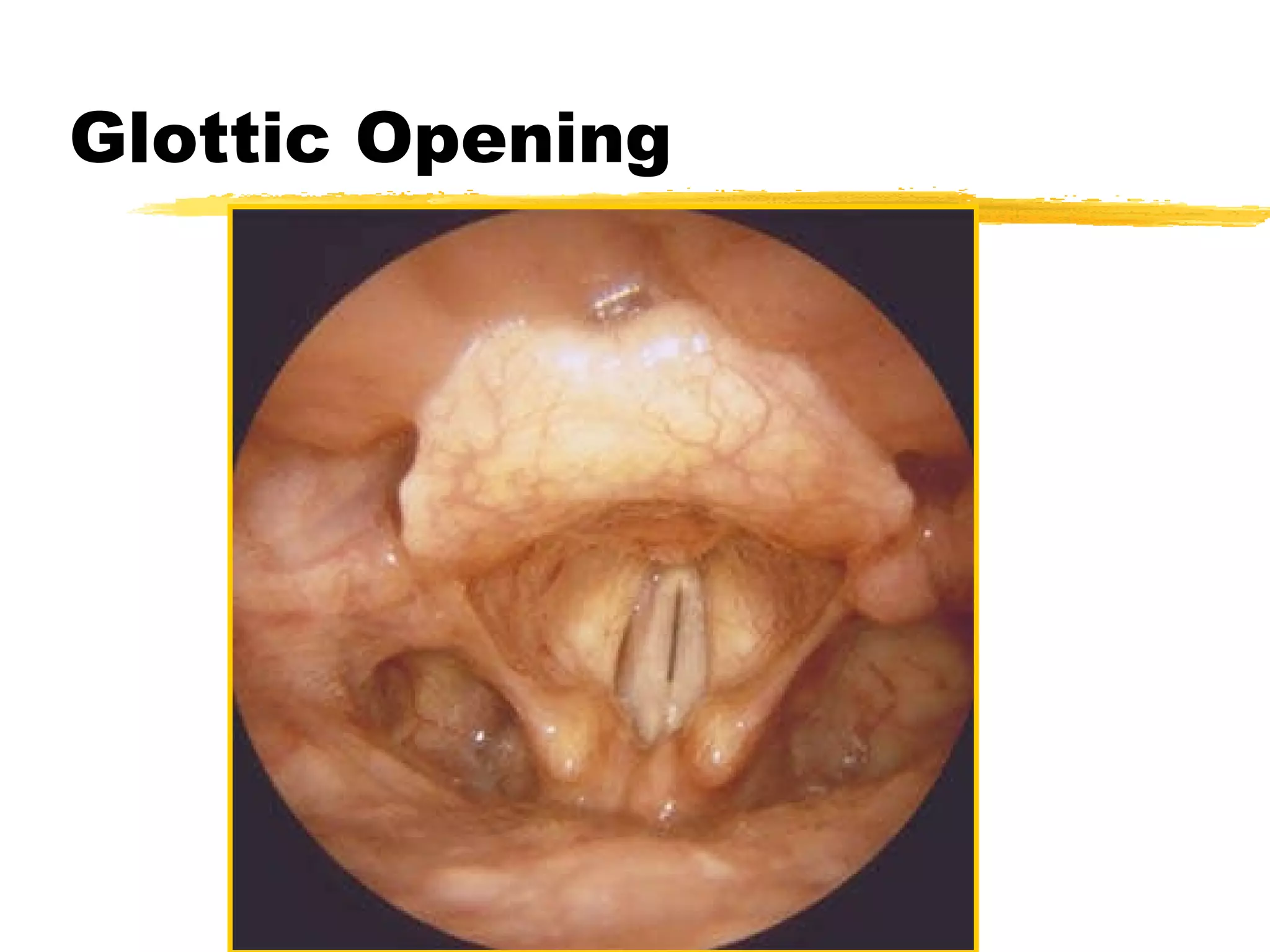
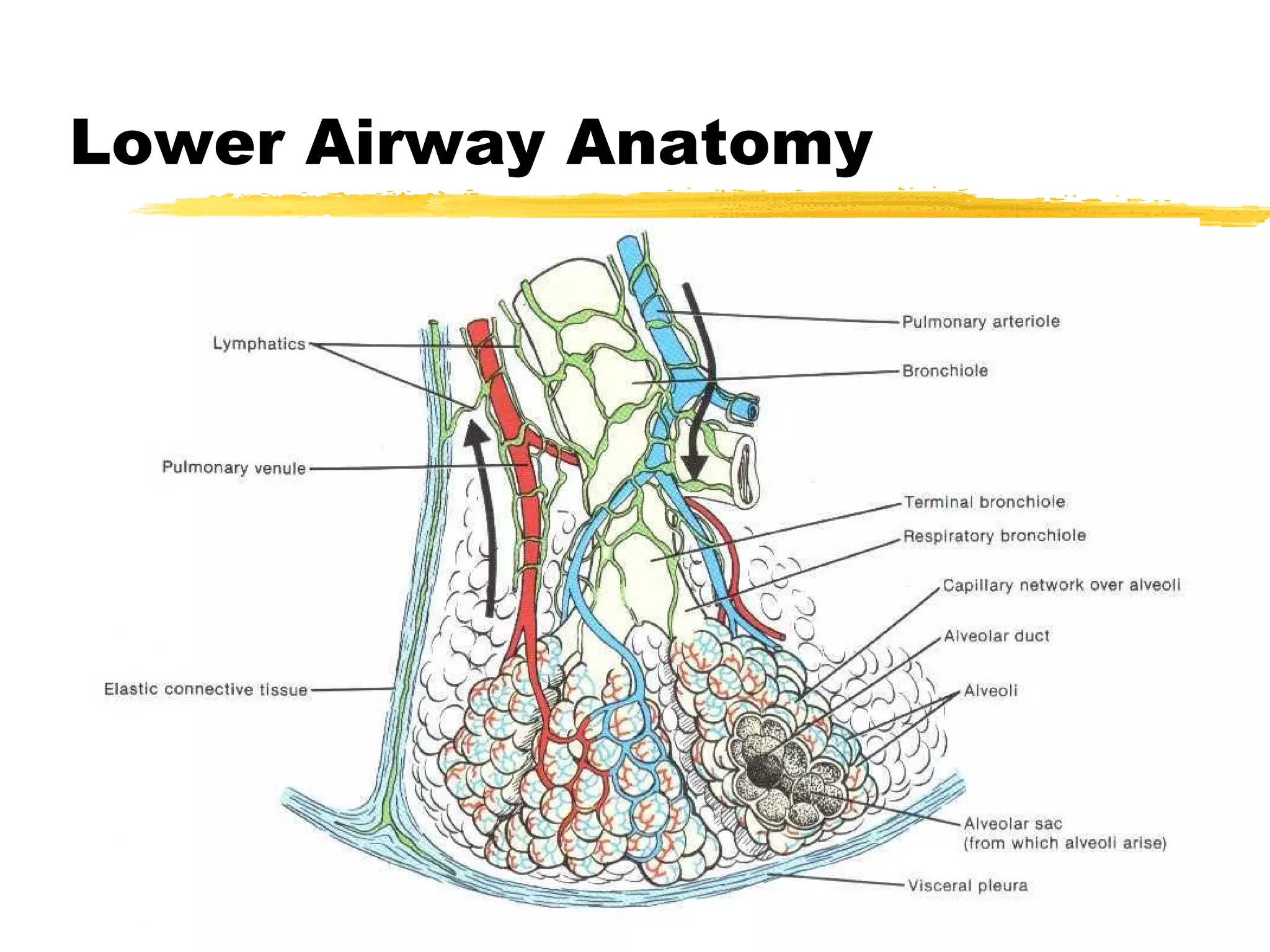
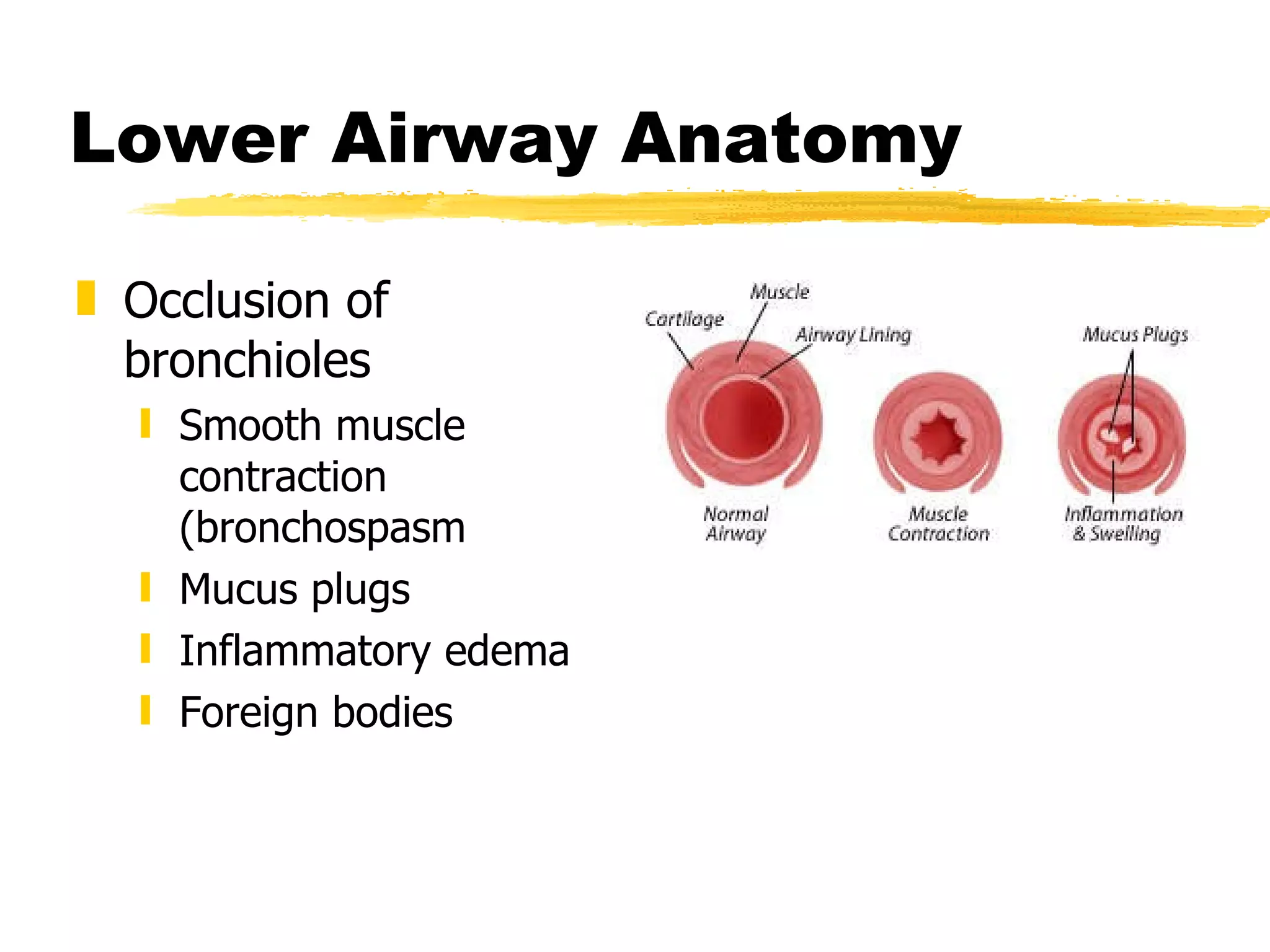
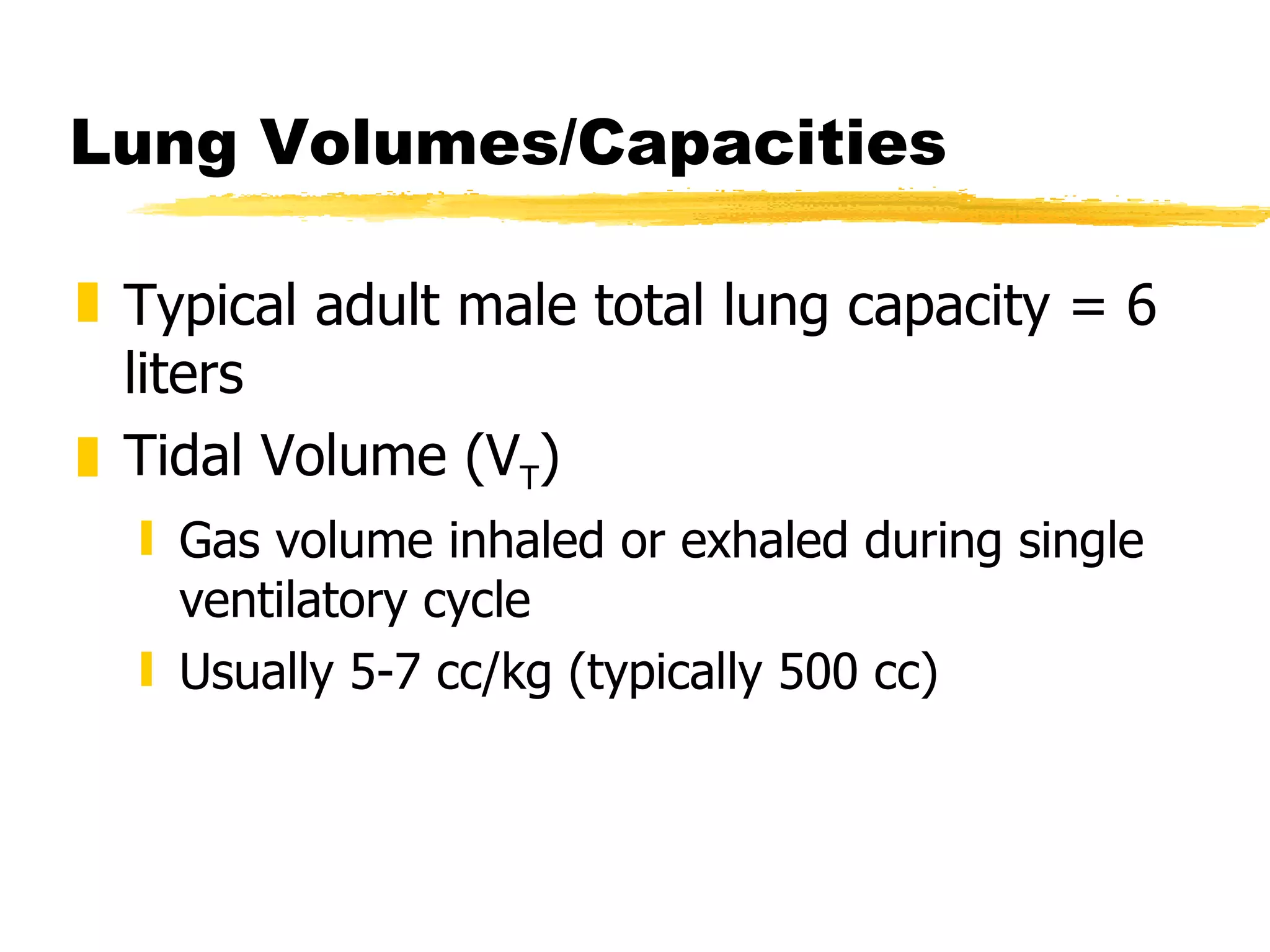
This document discusses airway management and ventilation for EMS professionals. It covers topics such as airway anatomy, causes of respiratory distress, methods of assessing the airway and ventilation, and basic life support airway management techniques including oxygen delivery devices. The objectives are to ensure optimal ventilation by delivering oxygen to the blood and removing carbon dioxide from the body.
![Lung Volumes/Capacities Alveolar Air (alveolar volume) [V A ] Air reaching alveoli for gas exchange Usually 350 cc](https://image.slidesharecdn.com/airwaymanagementpart1-100415030811-phpapp01/75/Airway-management-part-1-31-2048.jpg)
 Amount of gas moved in, out of respiratory tract per minute Tidal volume X RR Alveolar Minute Volume Amount of gas moved in, out of alveoli per minute (tidal volume - dead space volume) X RR](https://image.slidesharecdn.com/airwaymanagementpart1-100415030811-phpapp01/75/Airway-management-part-1-32-2048.jpg)