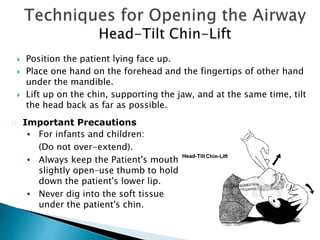
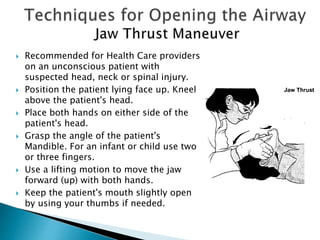
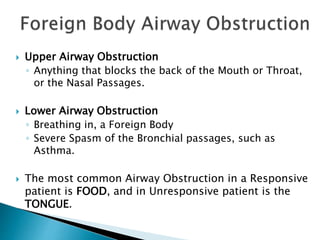
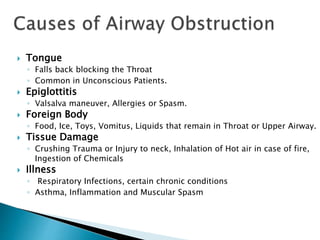
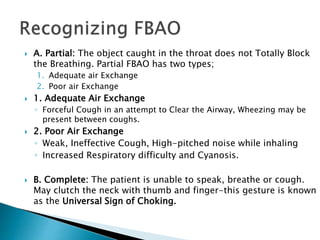
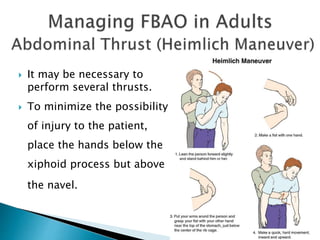
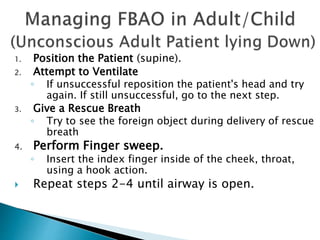
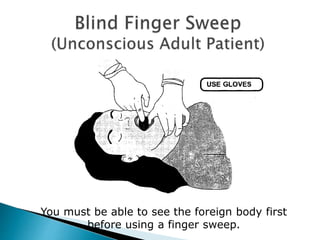
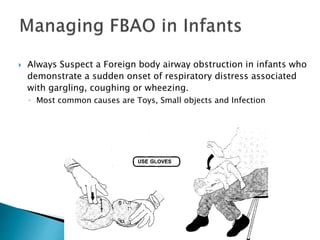
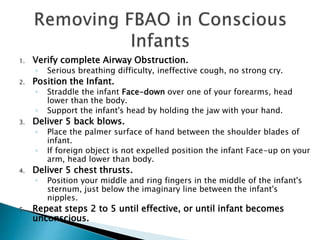
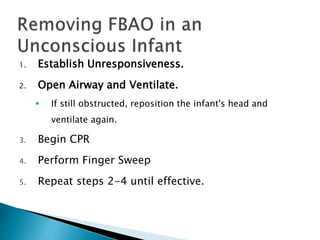
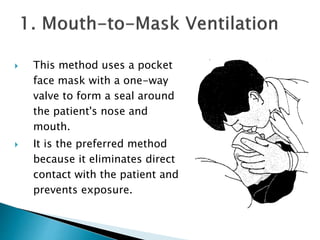
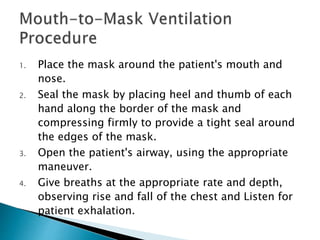
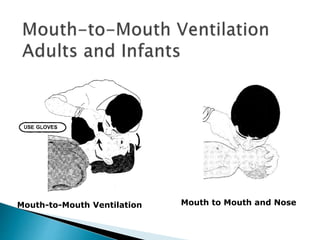
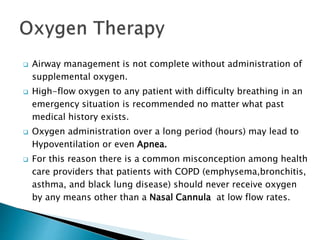
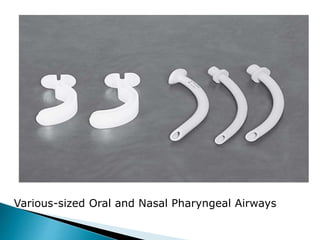
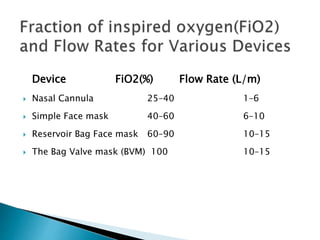
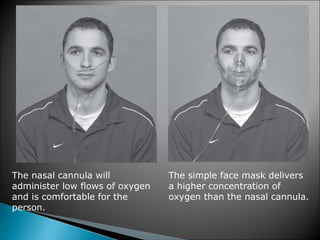
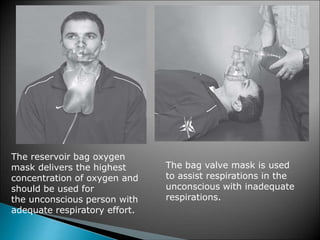
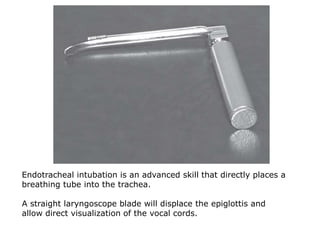
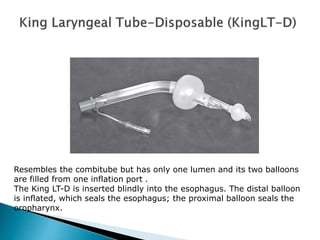
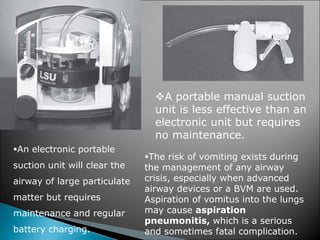
The document provides information on emergency care of the airway in athletic training. It discusses the anatomy of the upper and lower airway, including the oropharynx, nasopharynx, epiglottis, and larynx. Signs of an obstructed airway like cyanosis, snoring respirations, and accessory muscle use are outlined. Techniques for opening the airway like head-tilt chin-lift and jaw thrust are described. Foreign body airway obstructions and their management in adults, children, and infants are covered. Various methods of ventilation including mouth-to-mask, mouth-to-barrier, and mouth-to-mouth are explained. Finally, the document discusses oxygen therapy