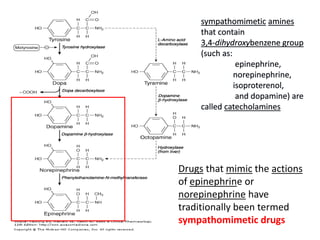
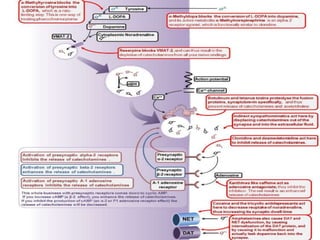
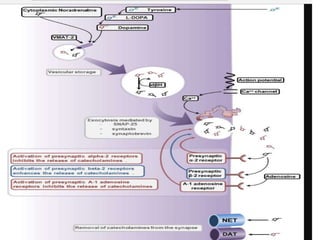
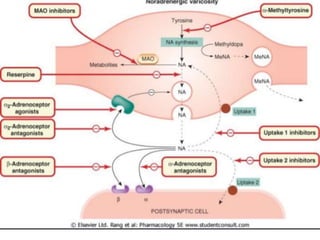
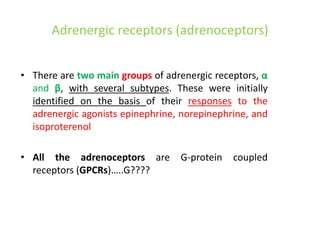
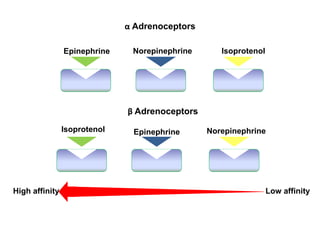
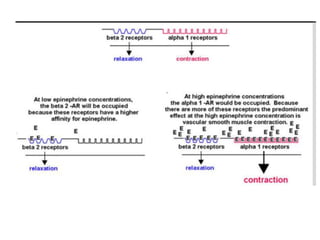
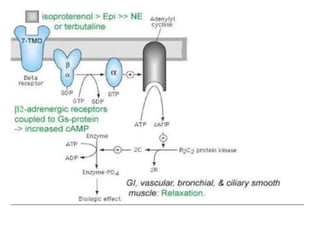
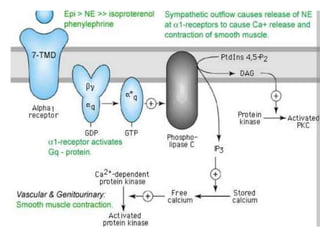
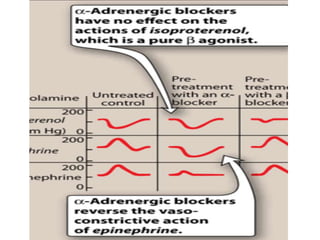
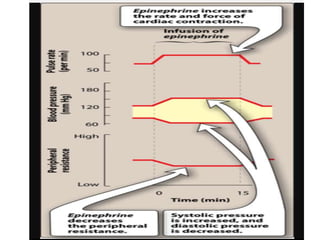
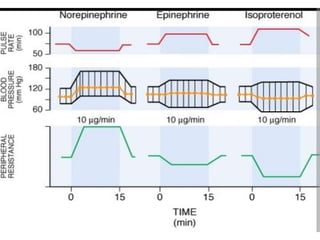
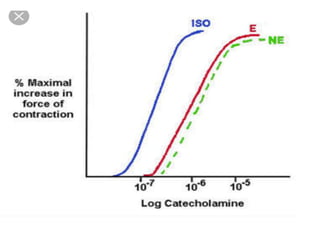
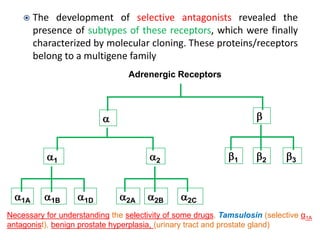
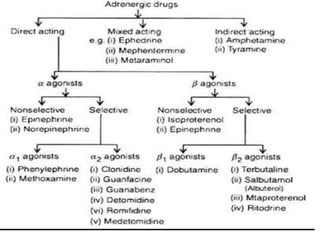
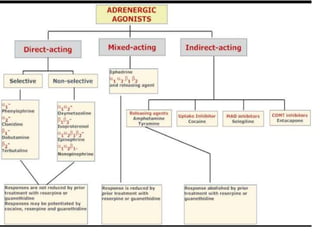
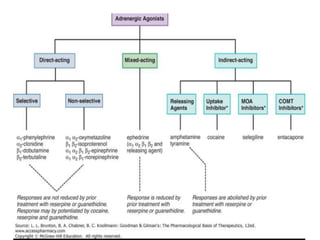
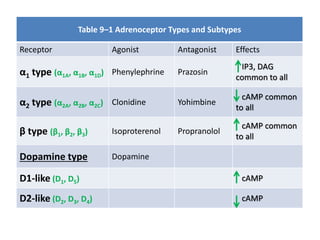
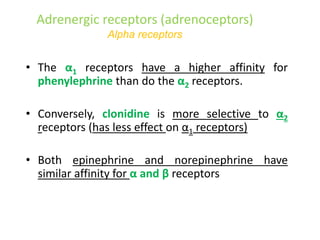
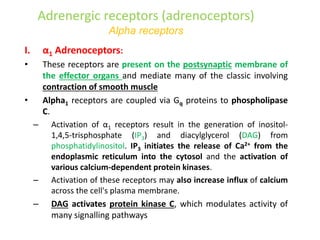
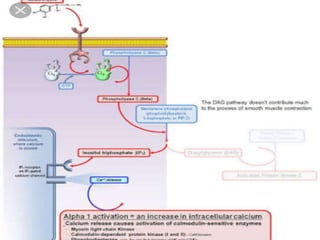
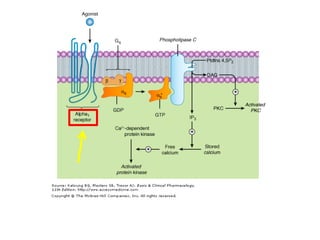
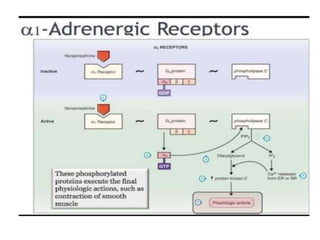
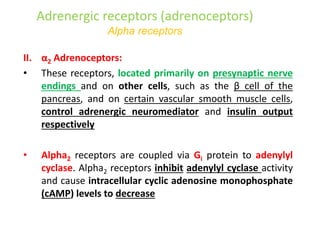
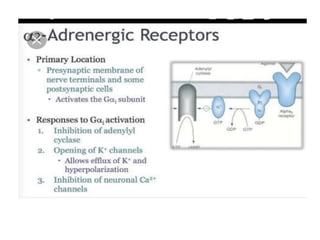
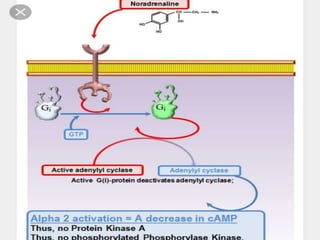
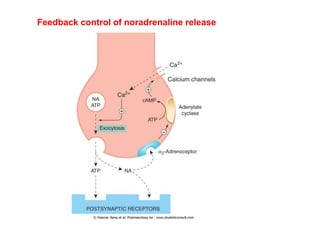
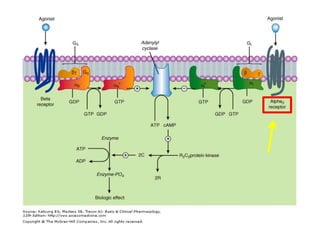
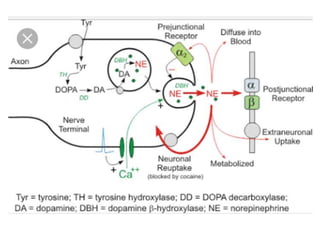
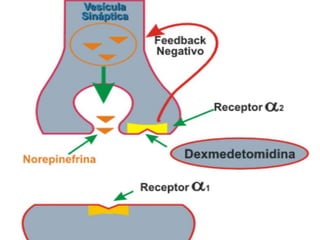
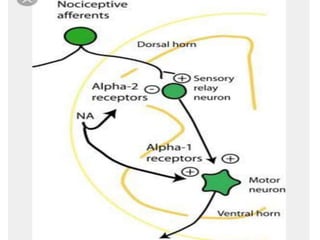
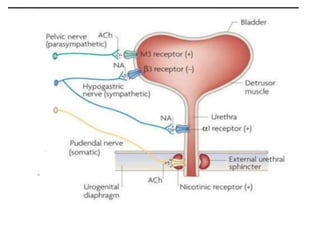
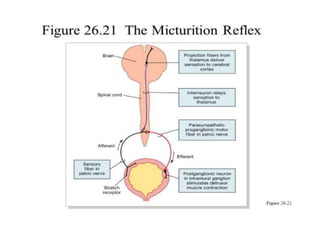
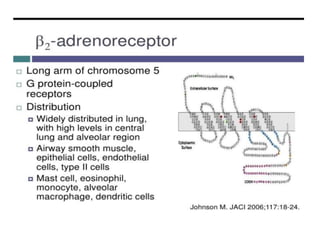
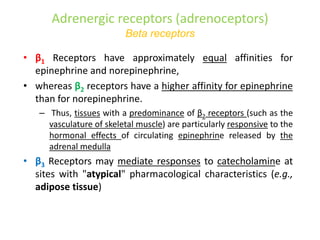
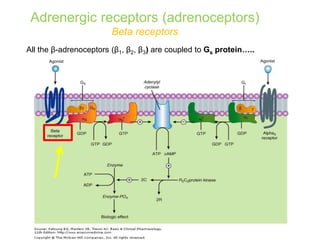
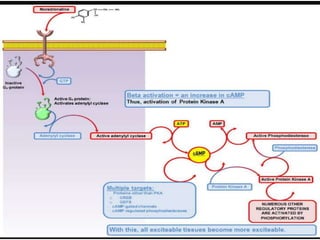
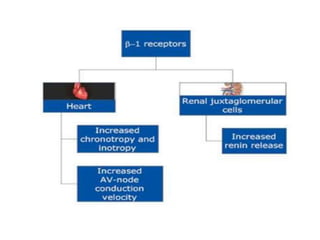
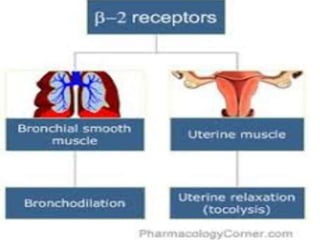
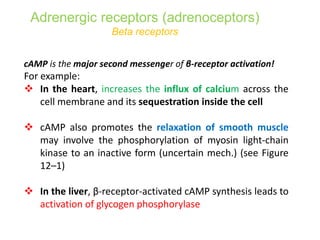
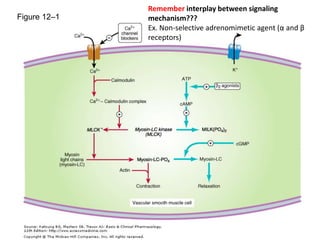
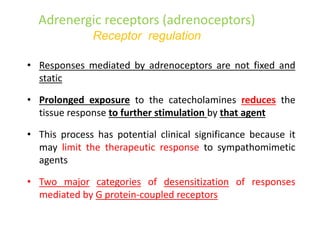
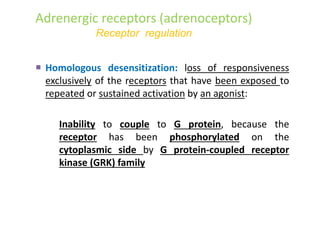
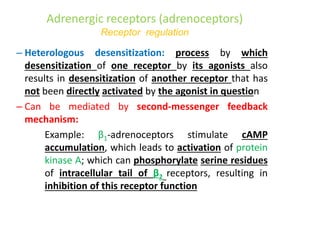
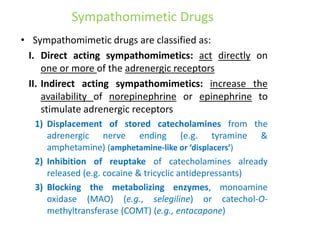
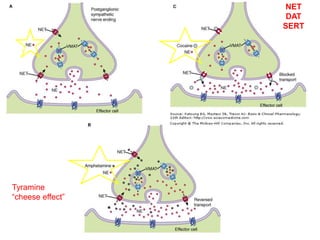
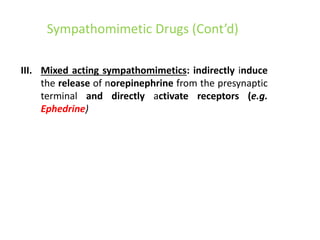
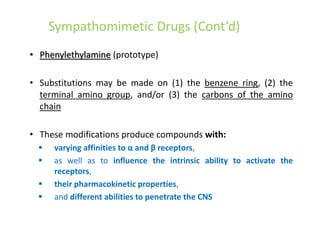
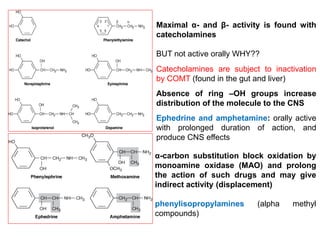
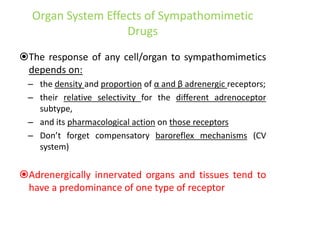
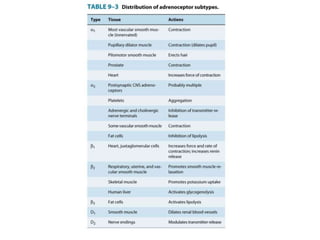
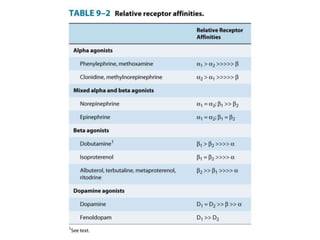
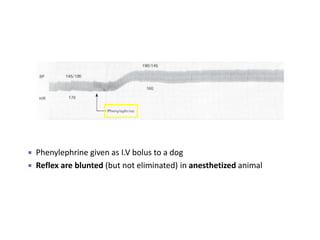
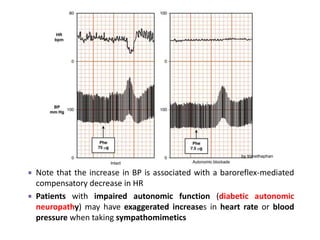
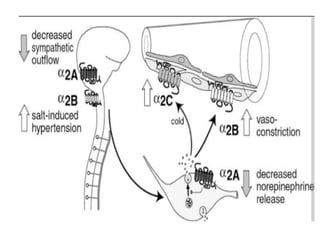
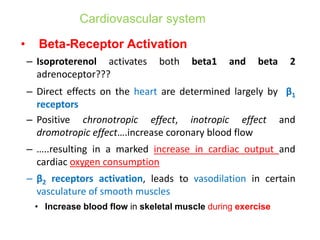
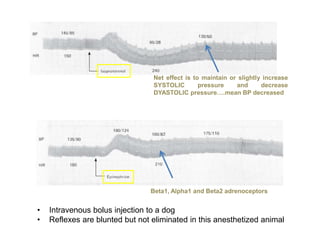
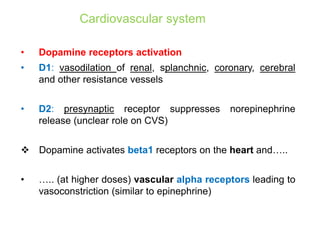
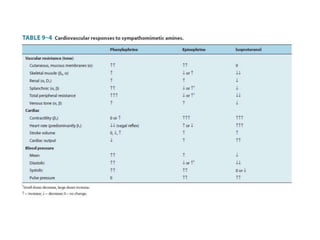
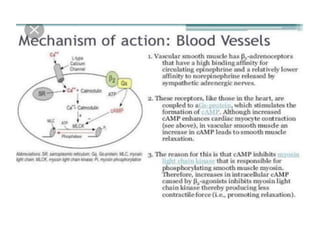
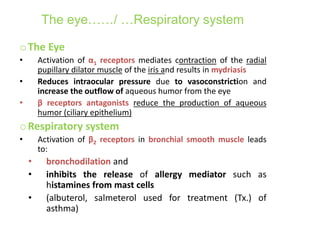
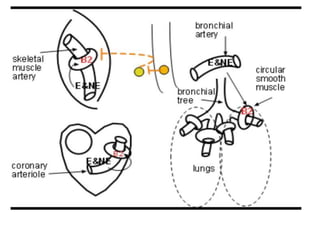
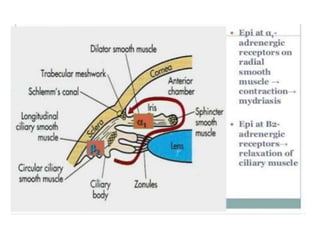
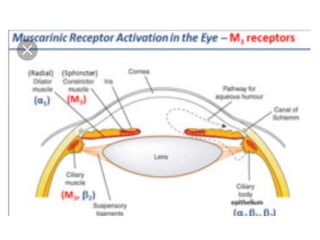
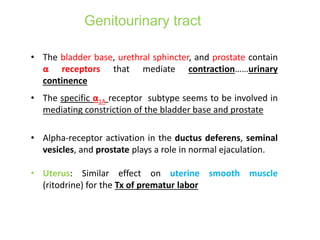
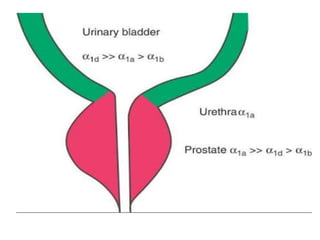
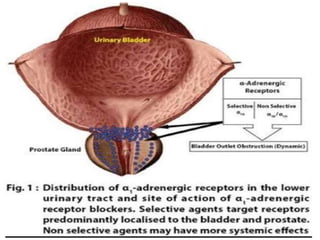
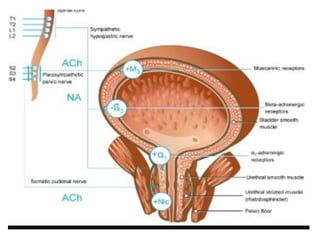
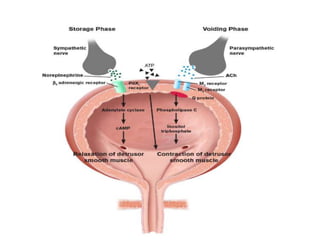
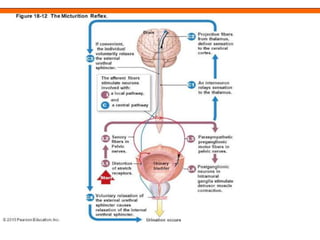
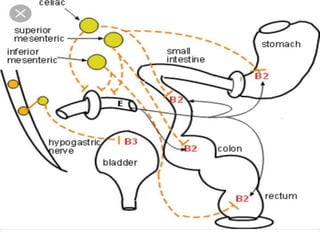
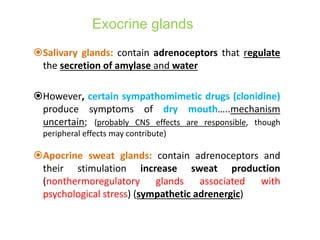
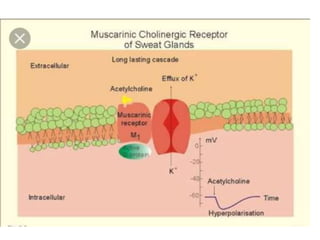
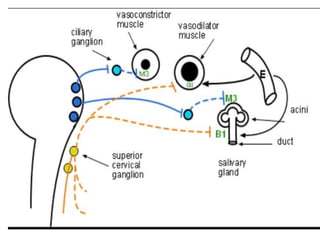
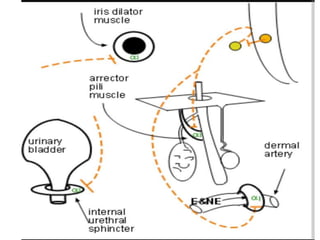
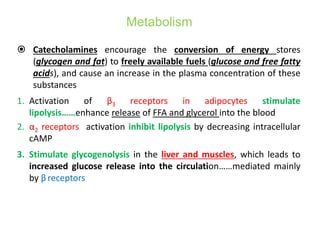
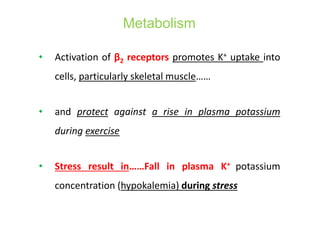
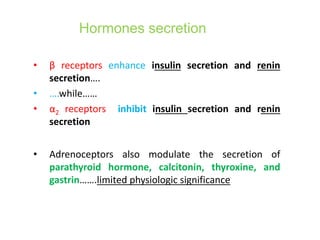
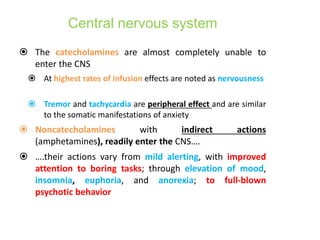
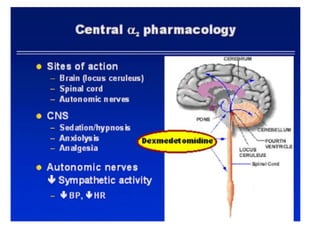
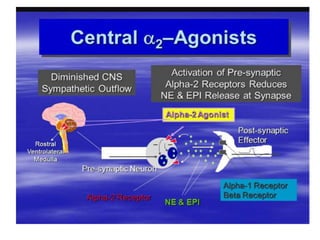
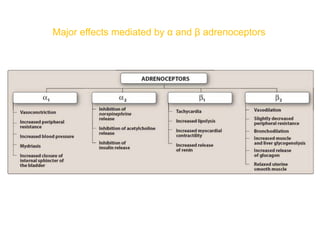
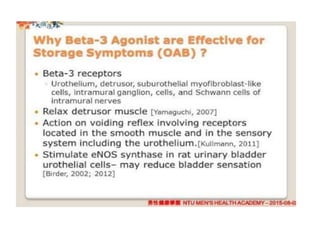
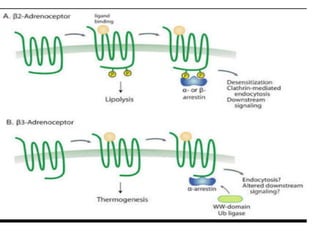
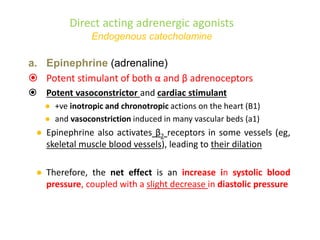
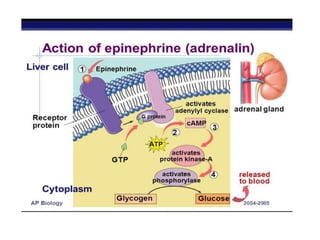
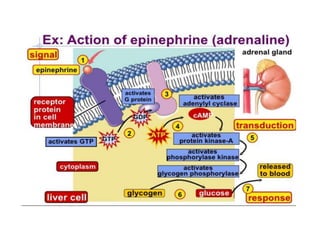
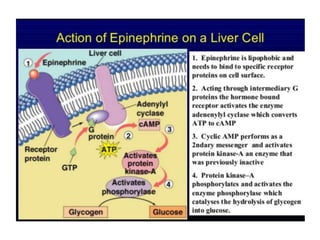
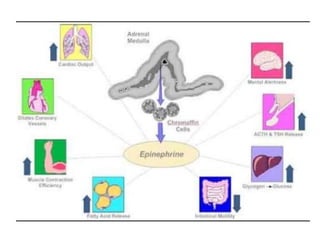
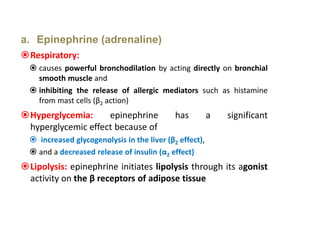
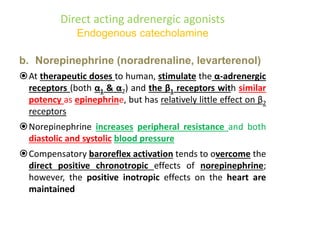
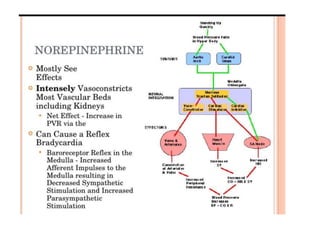
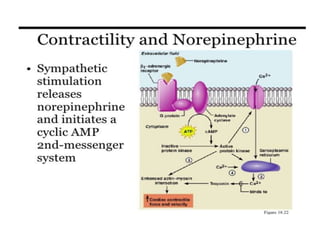
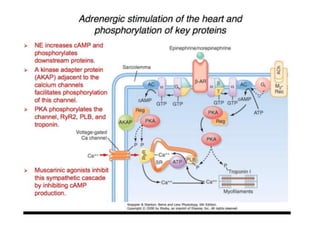
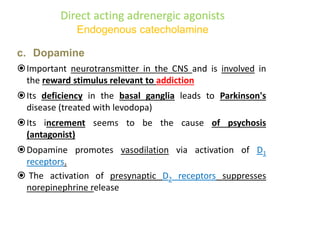
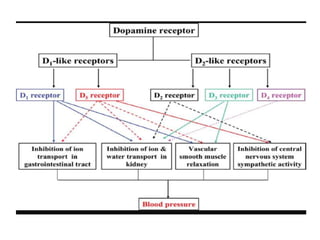
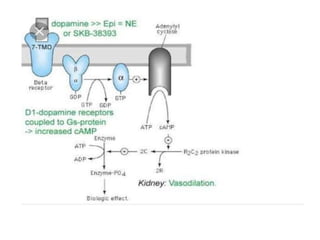
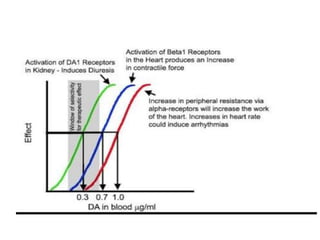
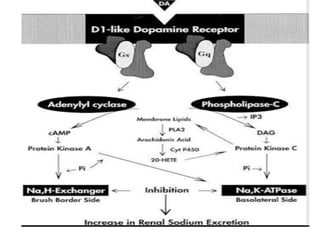
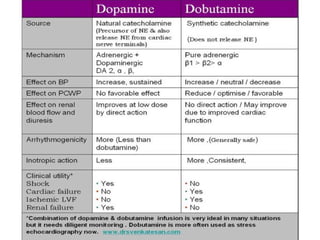
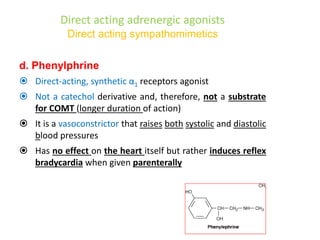
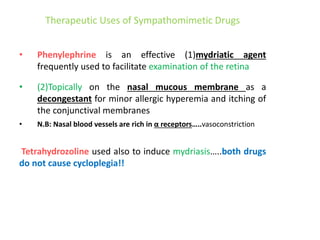
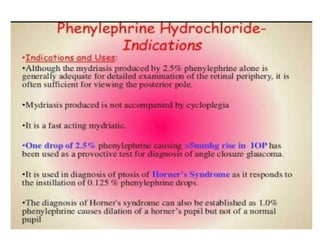
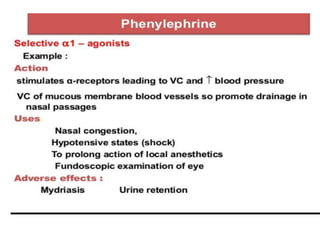
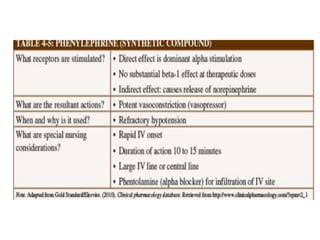
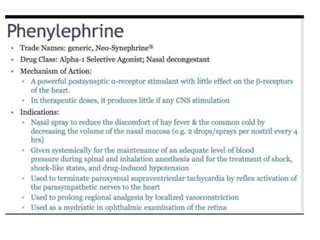
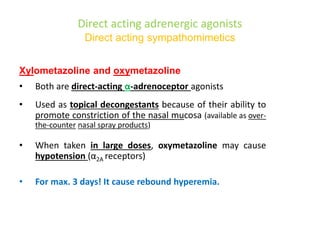
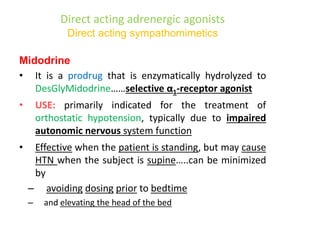
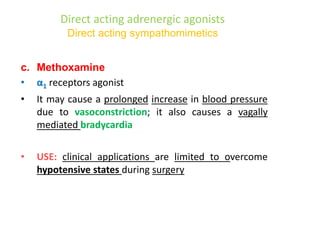
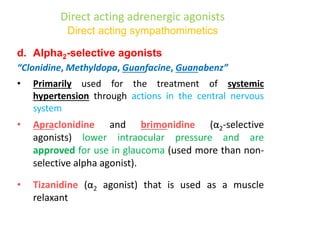
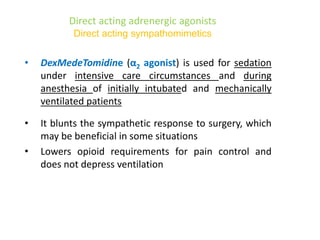
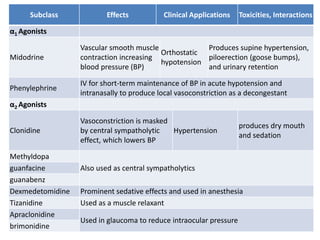
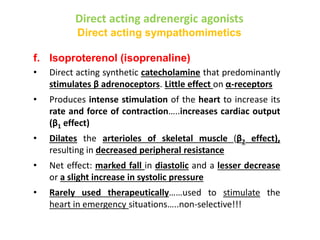
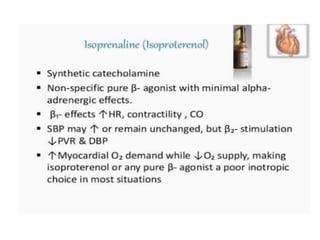
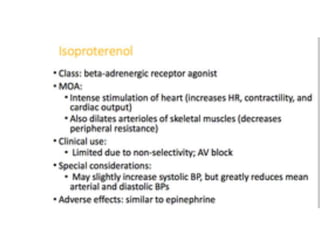
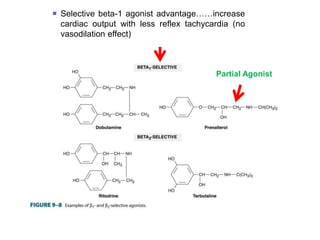
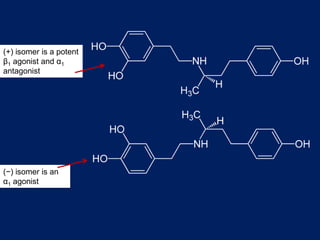
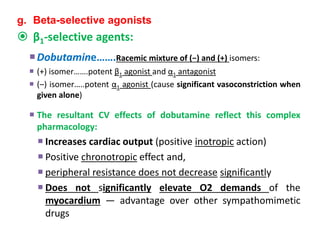
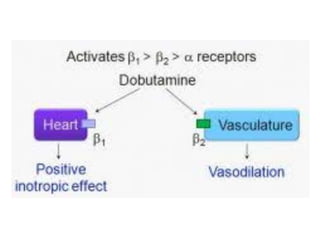
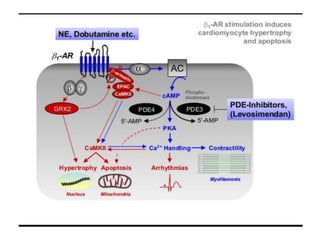
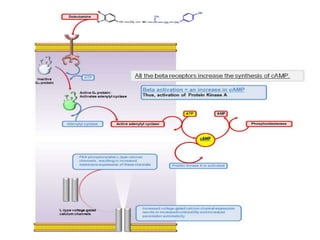
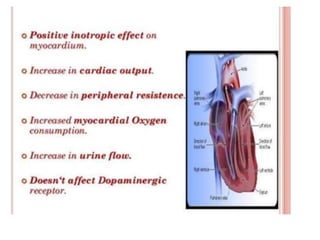
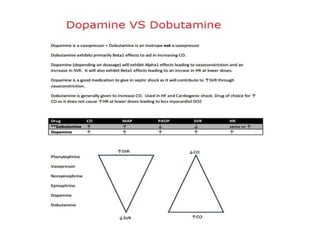
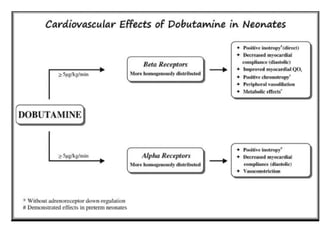
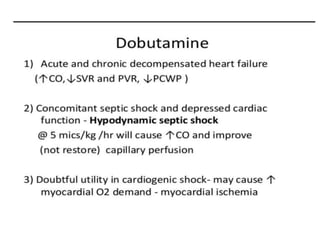
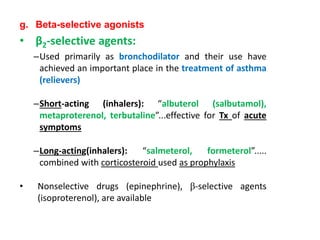
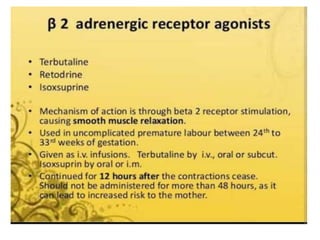
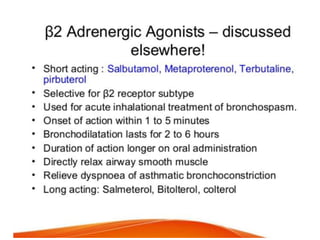
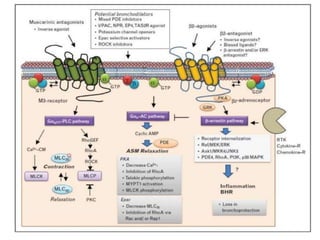
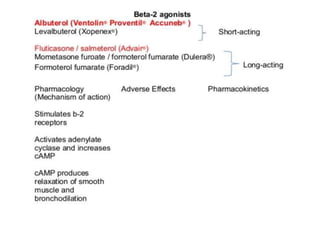
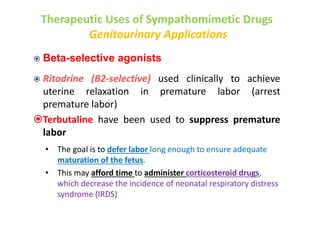
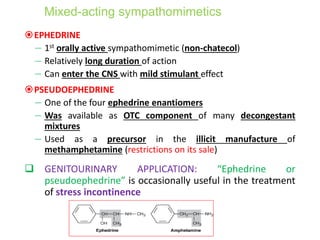
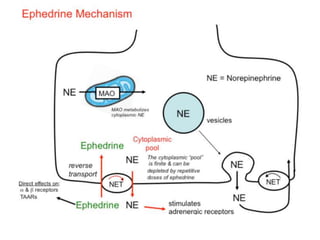
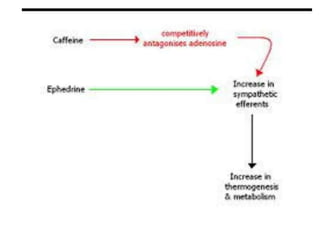
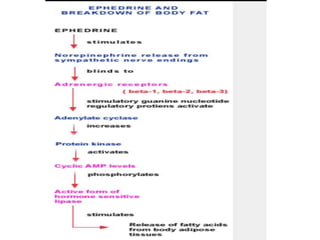
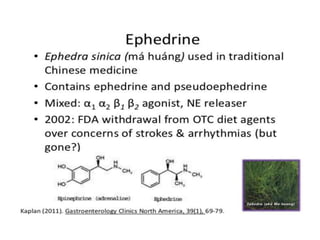
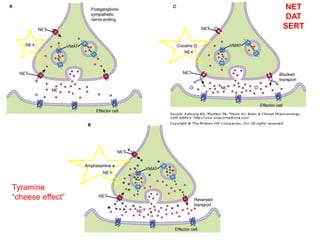
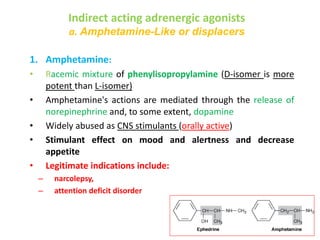
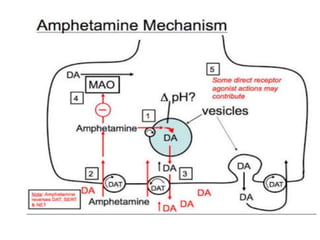
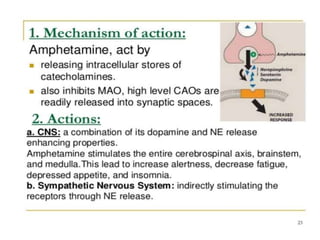
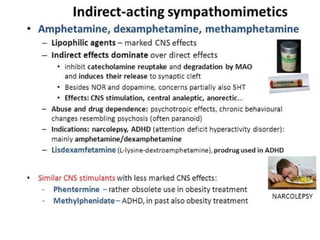
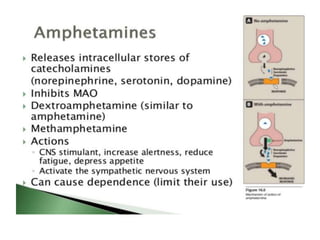
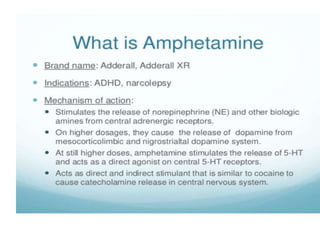
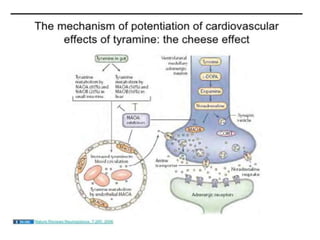
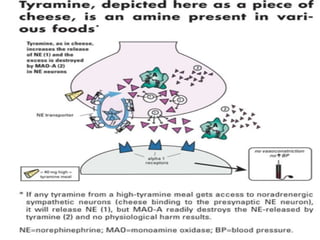
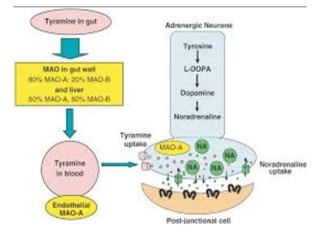
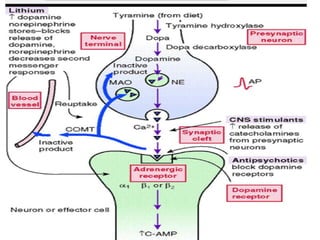
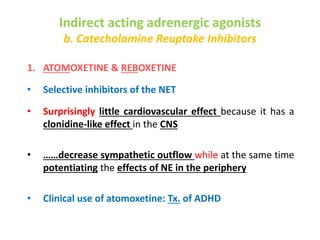
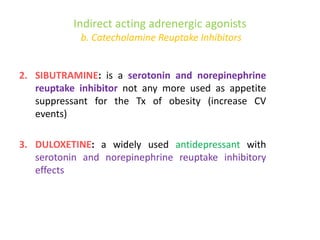
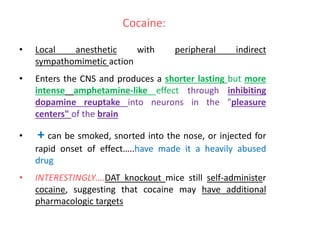
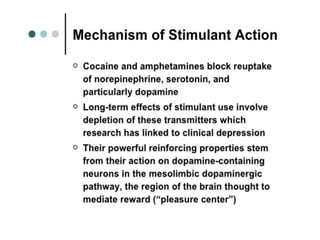
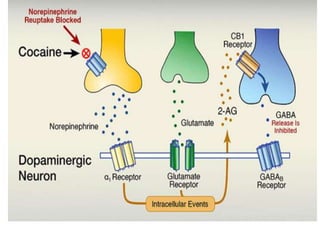
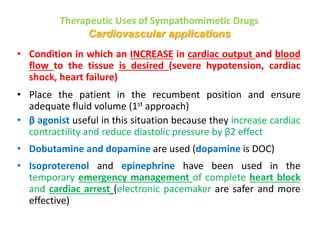
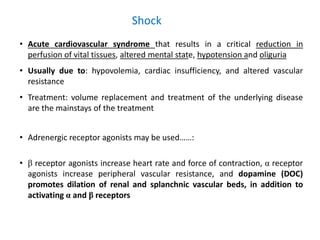
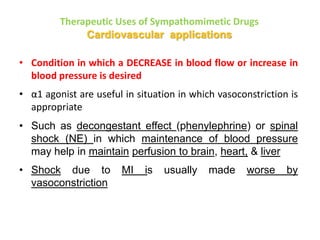
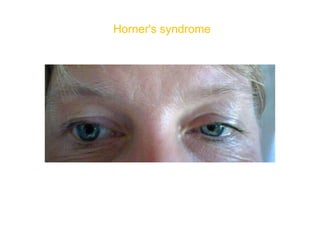
The document discusses adrenoceptor agonists and sympathormimetic drugs. It begins by overviewing the sympathetic nervous system and adrenergic receptors. It then describes the two main types of adrenergic receptors, α and β, which are G protein-coupled receptors. It also discusses the subtypes and selectivity of agonists and antagonists. Finally, it summarizes the organ system effects of sympathormimetic drugs and their mechanisms of action.