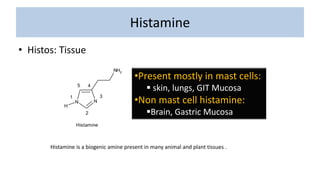
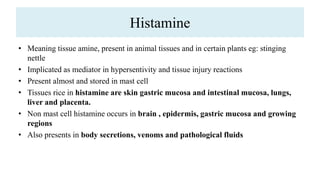
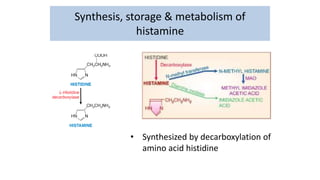
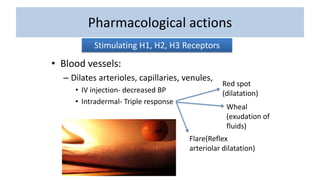
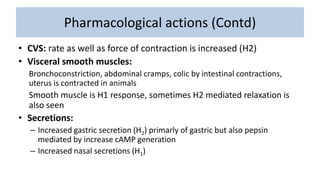
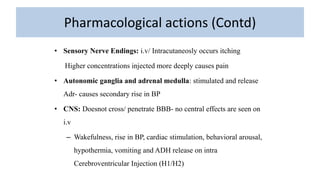
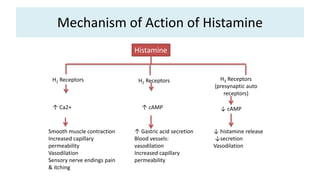
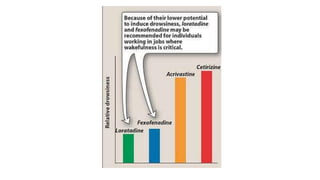
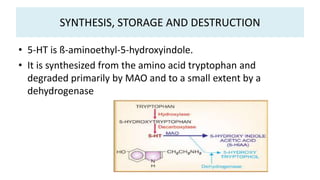
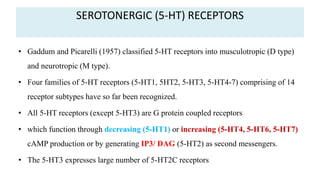
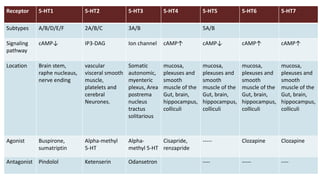
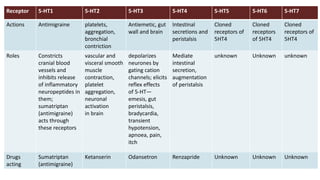
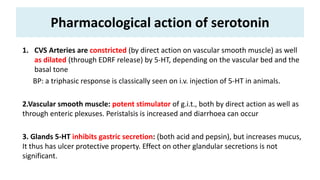
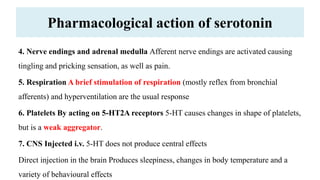
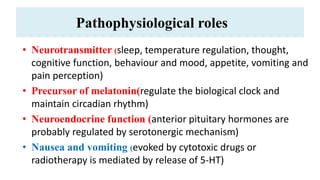
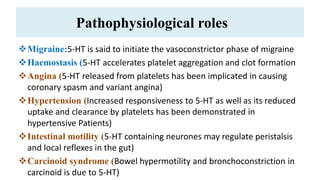
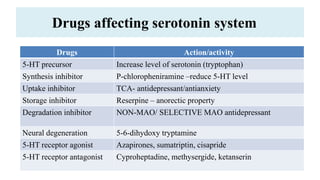
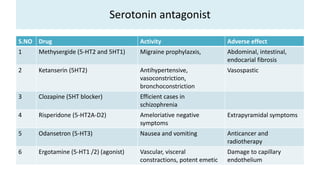
Histamine is a biogenic amine present in many animal and plant tissues. It is implicated as a mediator in hypersensitivity and tissue injury reactions. Histamine is present and stored in mast cells, especially in the skin, lungs, and gastrointestinal mucosa. It is synthesized from the amino acid histidine and acts on H1, H2, and H3 receptors to cause various pharmacological effects like vasodilation, increased capillary permeability, smooth muscle contraction, and increased gastric acid secretion. Serotonin is another amine present in enterochromaffin cells of the gastrointestinal tract. It is synthesized from tryptophan and acts on multiple 5-HT receptor subtypes to cause vasoconstriction, intestinal per