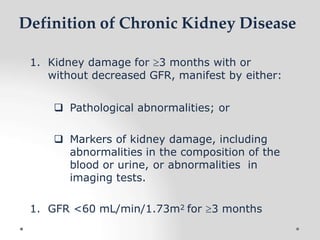
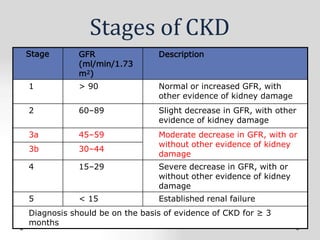
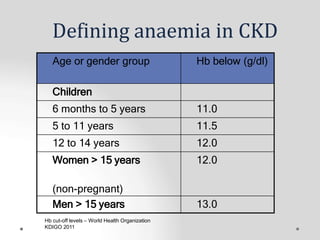
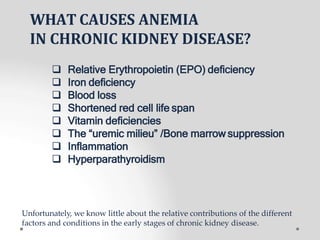
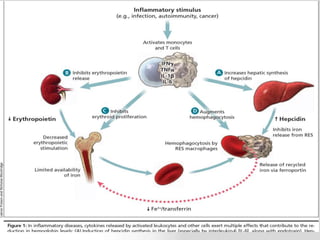
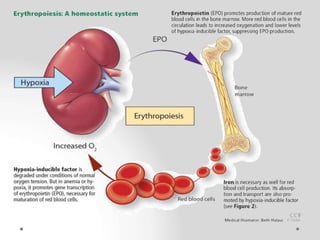
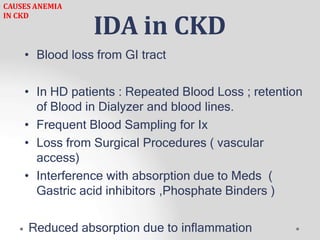
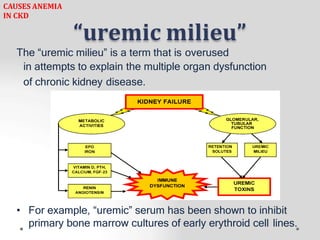
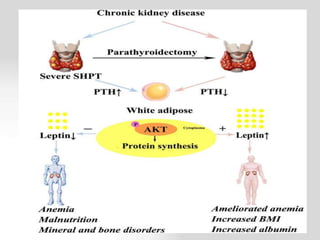
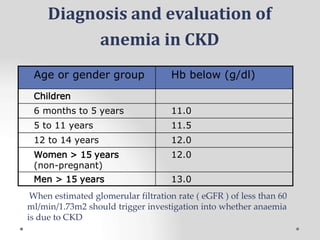
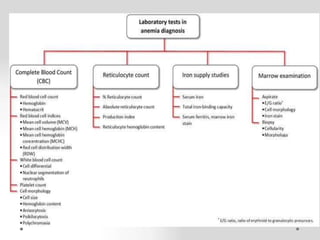
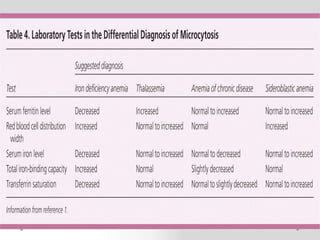
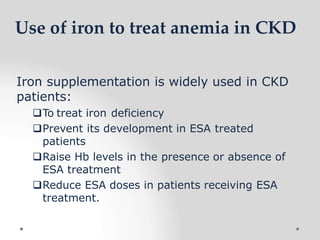
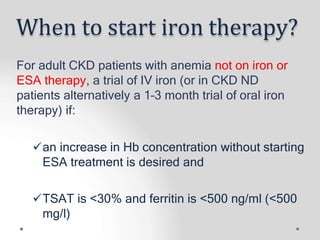
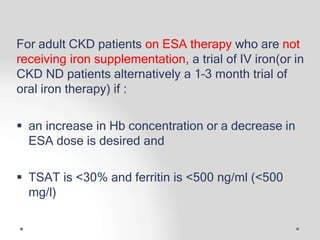
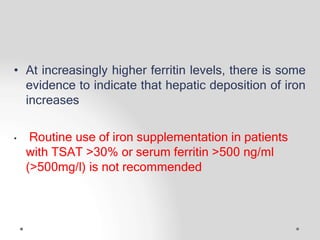
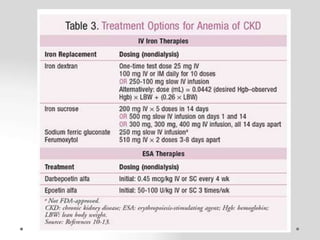
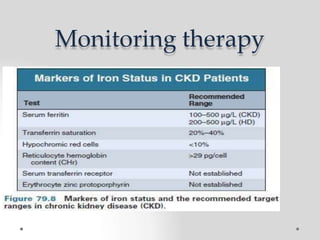
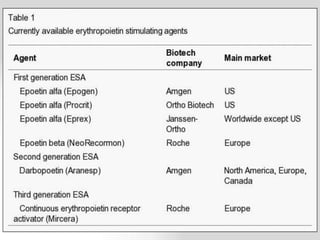
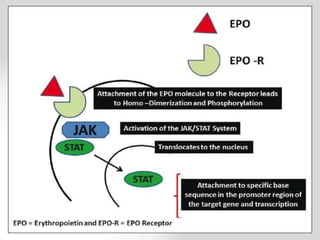
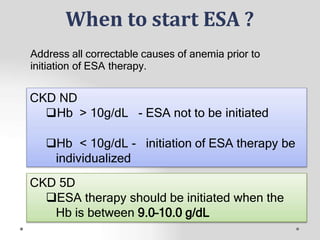
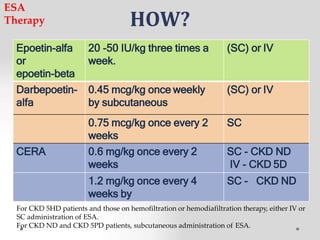
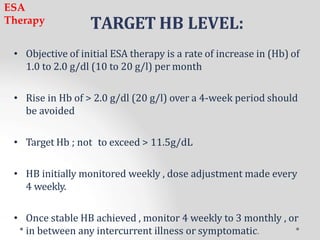
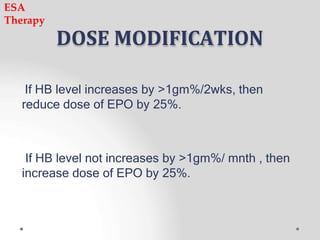
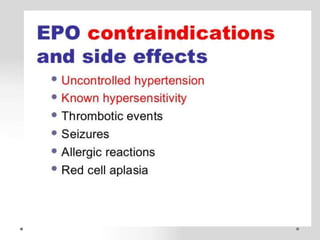
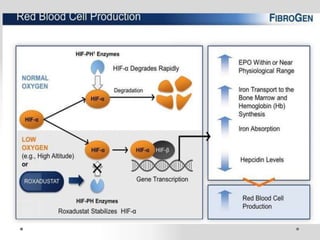
This document discusses chronic kidney disease (CKD), anemia in CKD, and treatments for anemia in CKD. It defines CKD and its stages based on glomerular filtration rate and kidney damage. Anemia in CKD is defined based on hemoglobin levels. Causes of anemia in CKD include relative erythropoietin deficiency, iron deficiency, blood loss, shortened red blood cell lifespan, and the "uremic milieu." Iron therapy and erythropoiesis-stimulating agents (ESAs) are discussed as treatments for anemia in CKD, including criteria for starting therapy, drug options, dosing, monitoring, and dose adjustment.