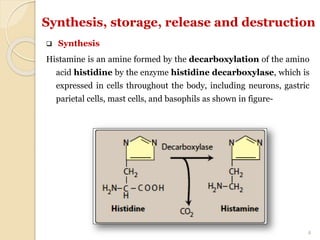
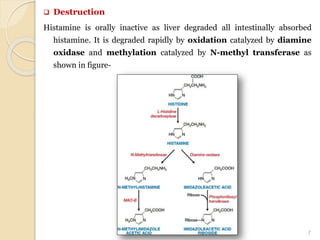
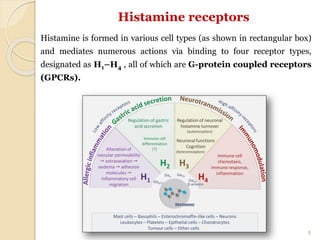
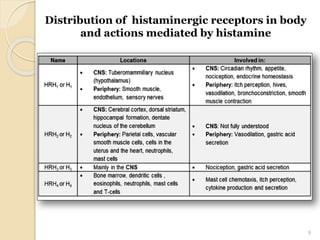
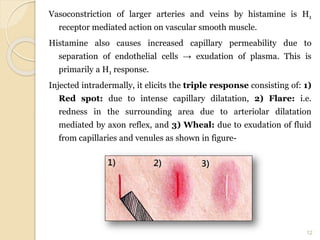
The document provides a detailed overview of histamine, including its synthesis, storage, release, and destruction, as well as its receptors and pharmacological actions. Histamine plays significant roles in allergic reactions, gastric secretion, and the central nervous system, while also influencing various physiological processes. While it has no modern clinical uses, historic applications included testing gastric acid secretion and bronchial hyperreactivity, and the document also mentions histamine analogues like betahistine that serve specific therapeutic effects.