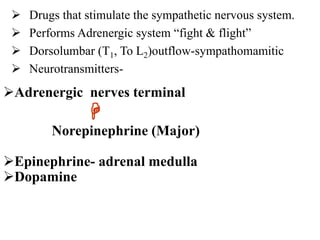
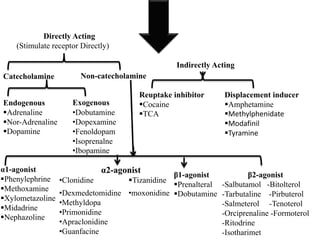
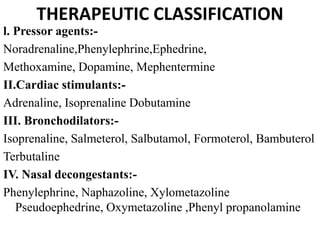
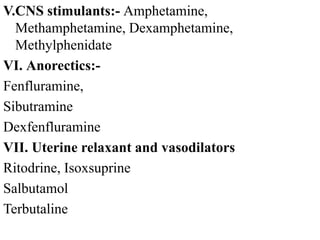
The document discusses the sympathetic nervous system and adrenergic receptors. It describes:
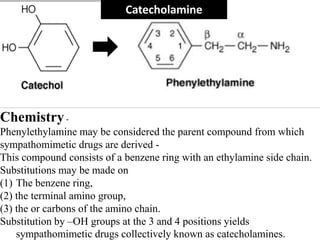
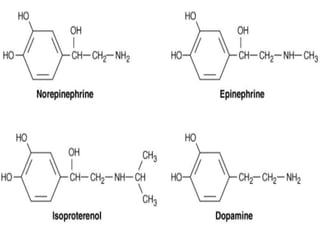
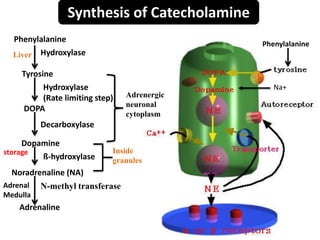
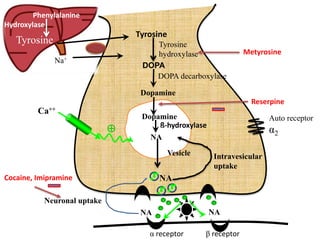
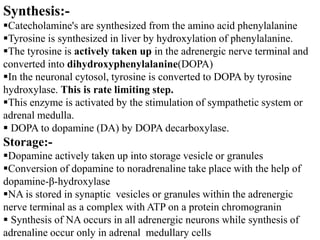
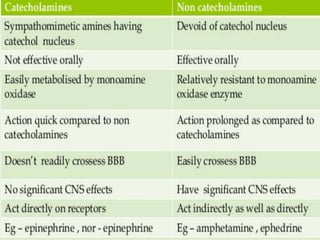
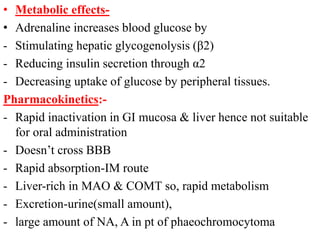
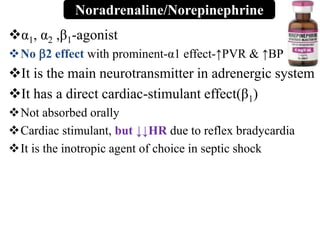
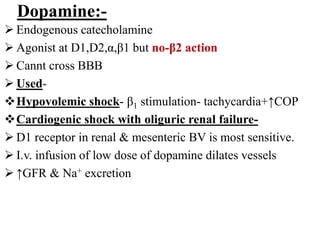
1) How catecholamines like norepinephrine and epinephrine are synthesized from phenylalanine and tyrosine and stored in vesicles for release.
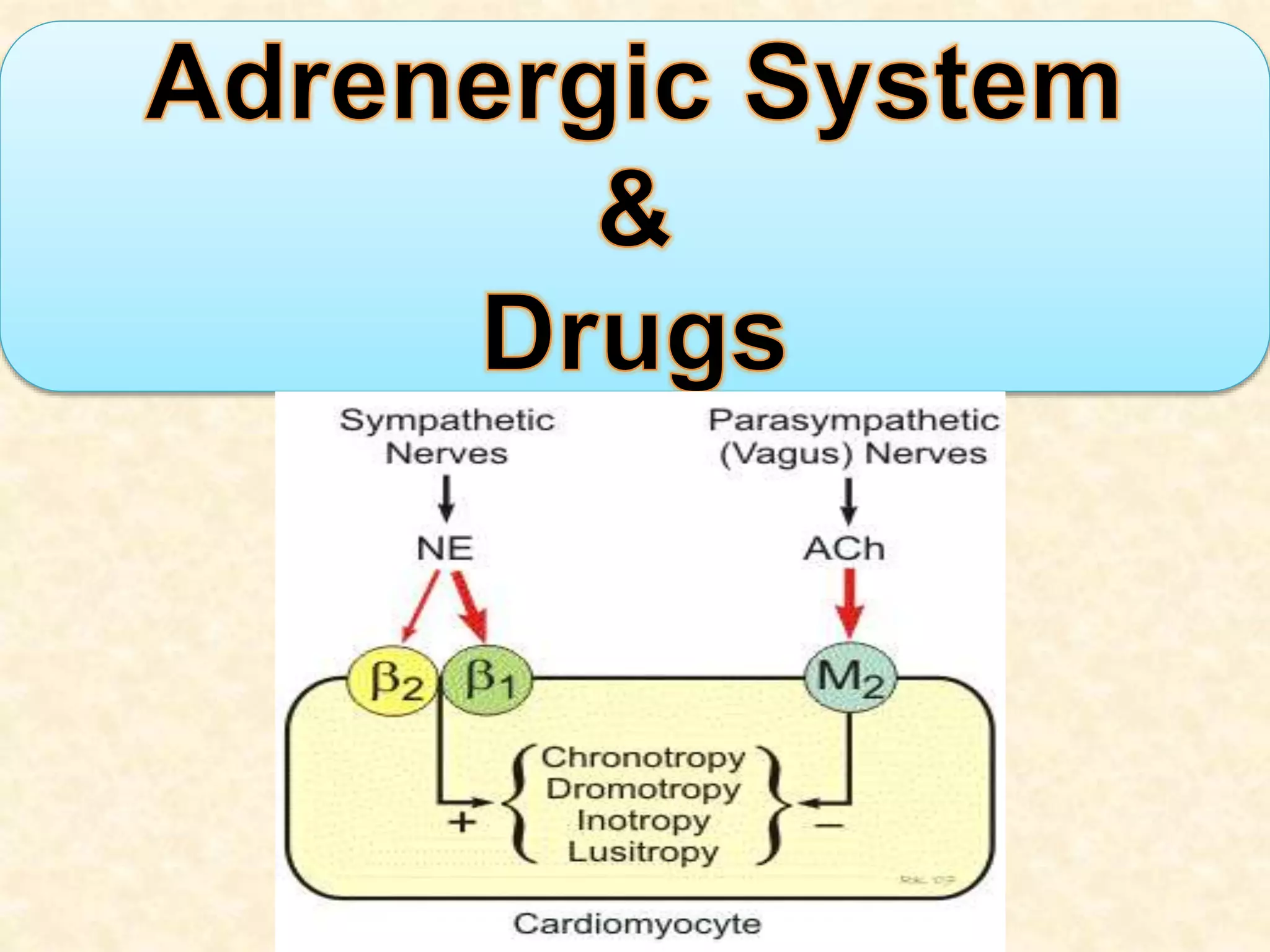
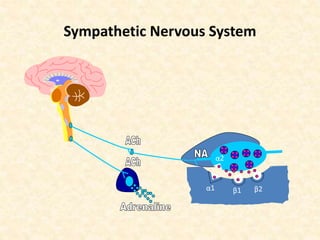
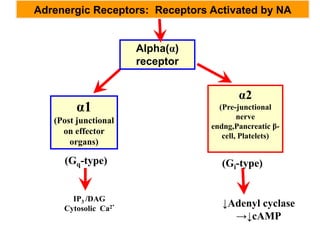
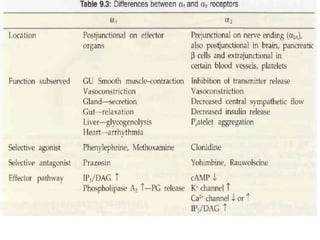
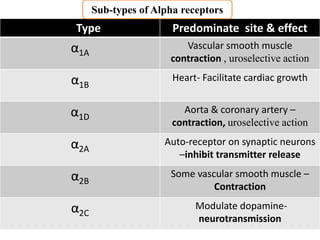
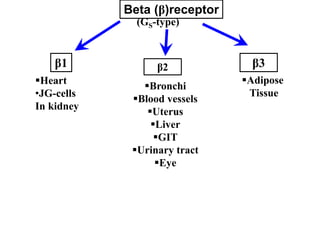
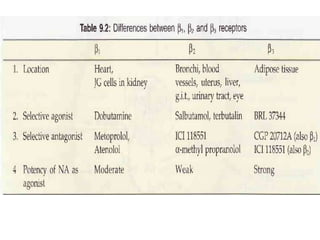
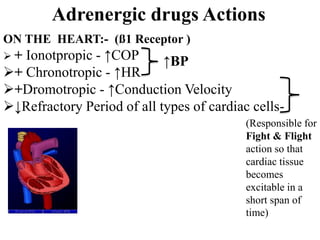
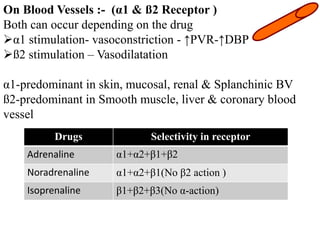
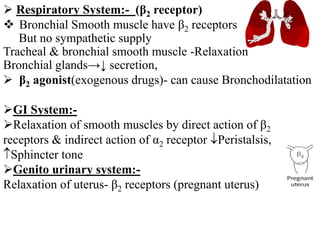
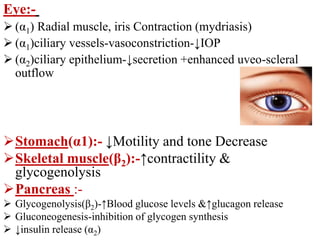
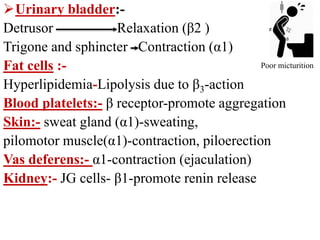
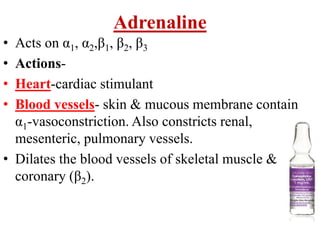
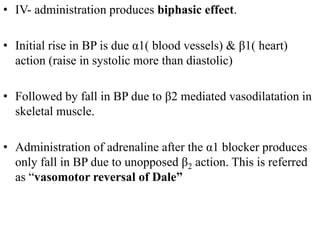
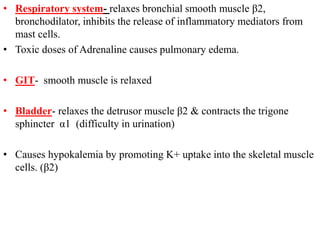
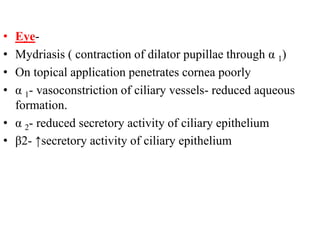
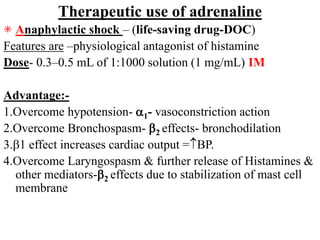
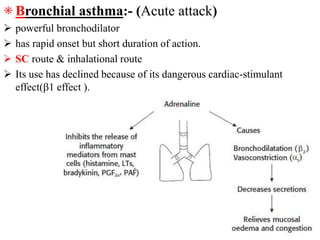
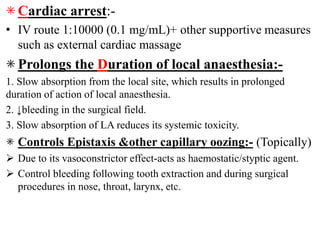
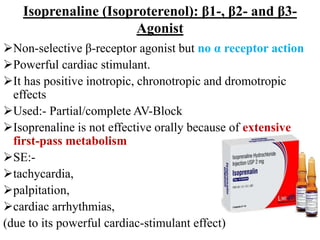
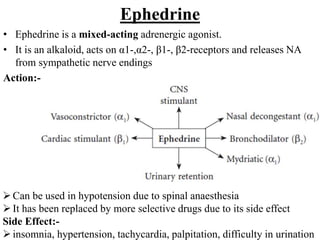
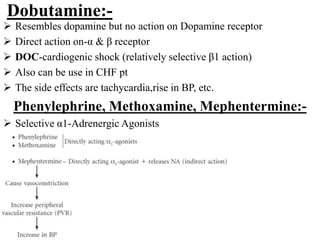
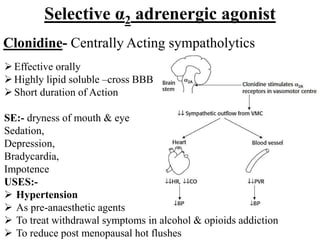
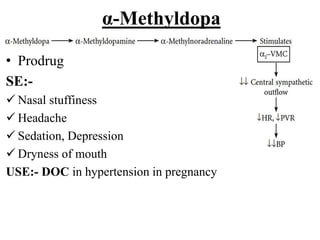
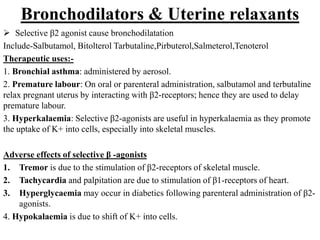
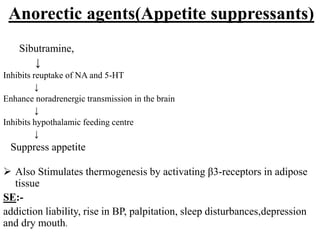
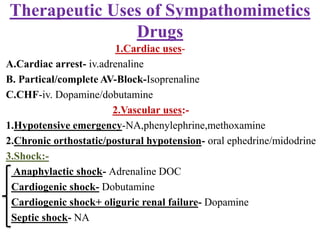
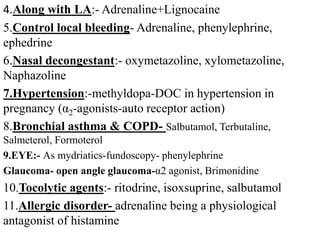
2) The different types of adrenergic receptors - alpha1, alpha2, beta1, beta2, and beta3 - and their locations and effects.
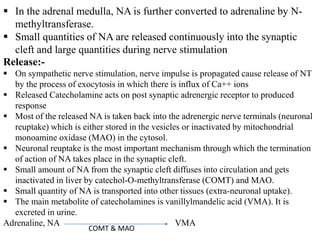
3) How catecholamines are released from neurons upon stimulation and their actions on various organs via receptor activation or reuptake.