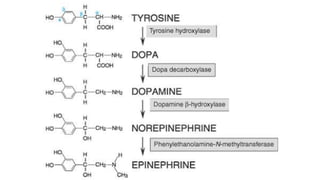
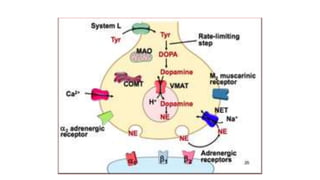
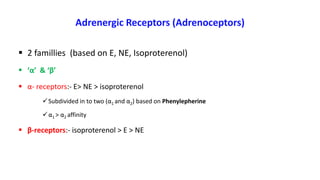
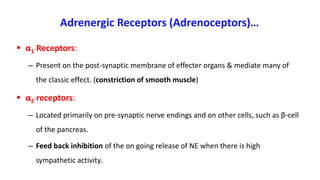
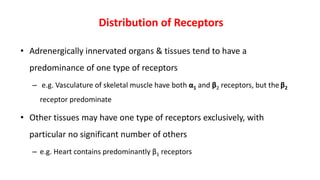
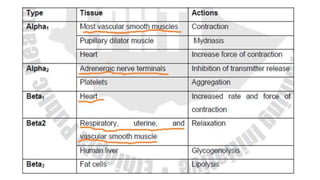
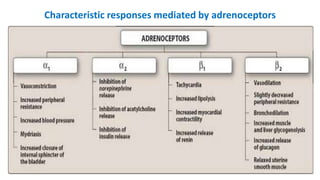
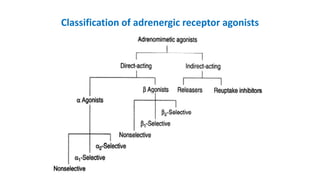
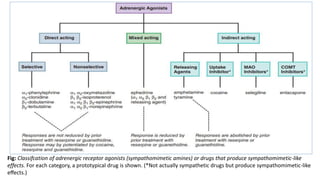
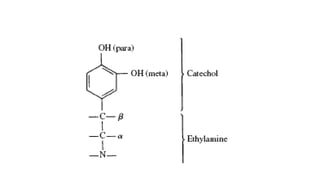
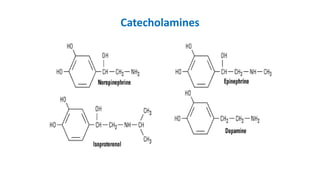
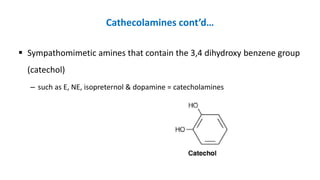
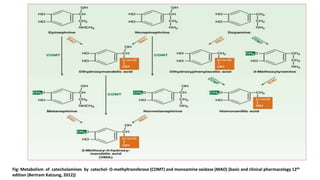
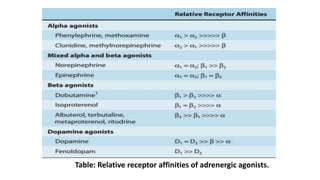
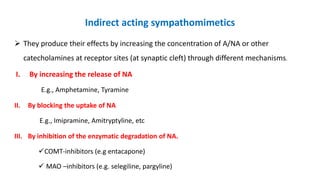
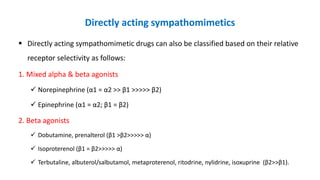
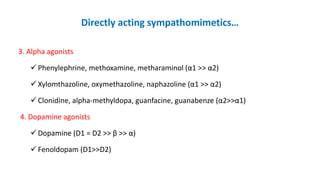
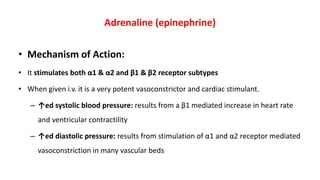
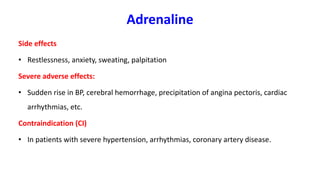
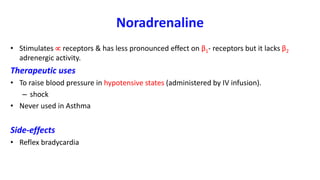
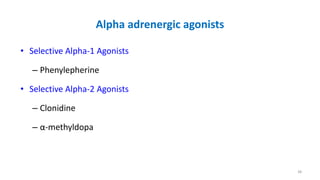
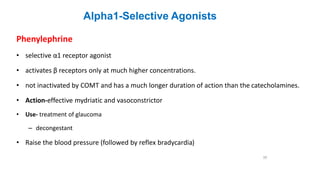
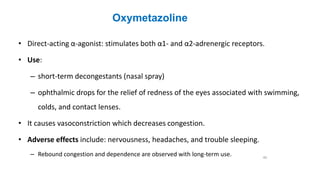
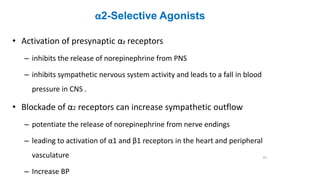
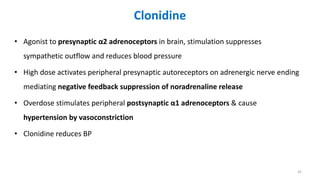
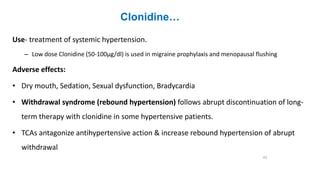
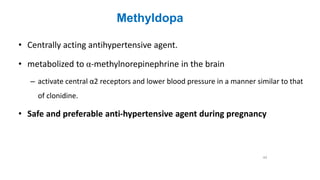
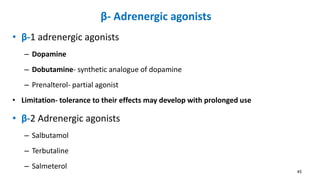
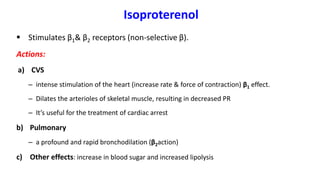
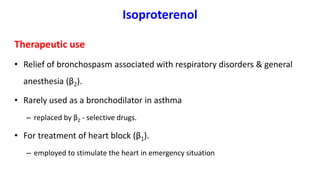
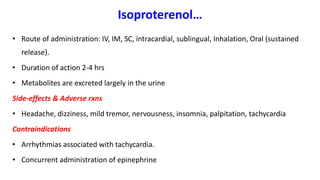
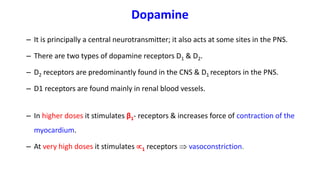
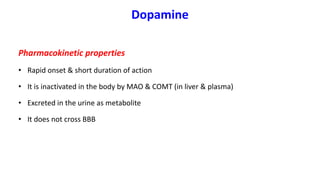
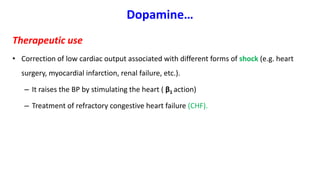
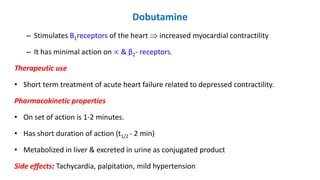
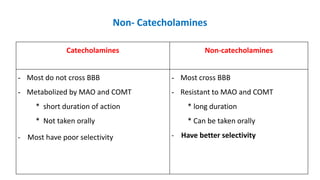
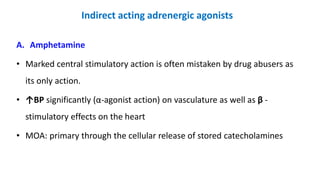
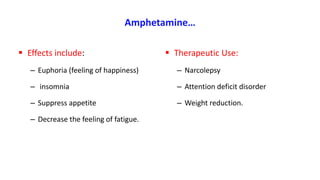
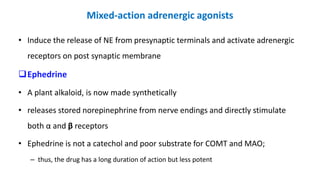
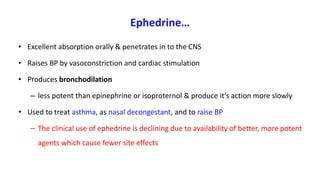
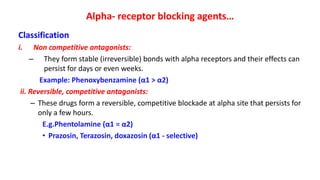
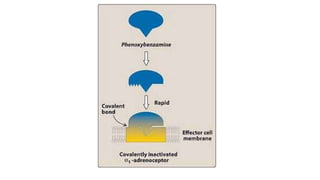
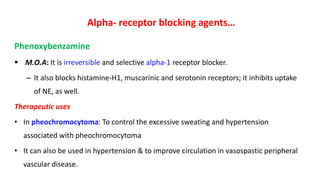
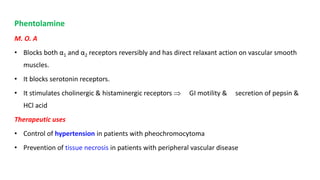
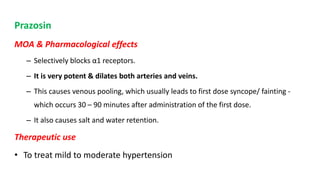
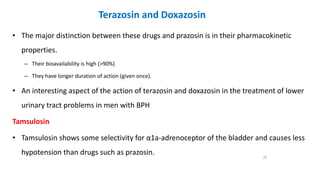
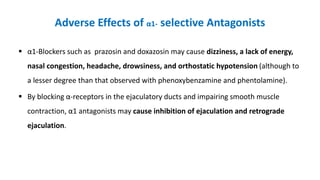
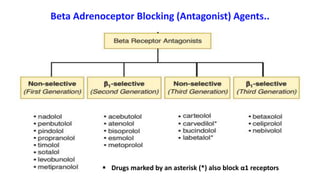
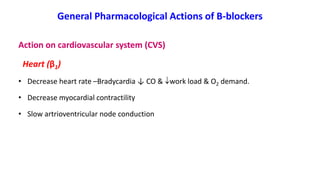
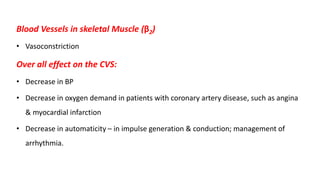
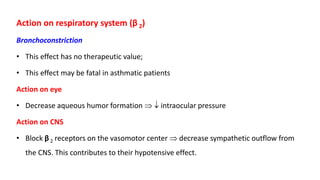
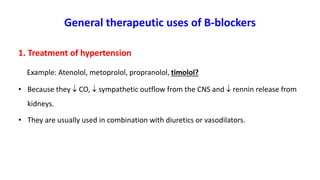
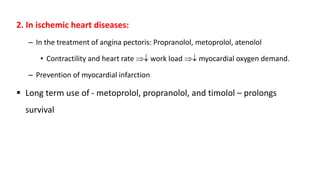
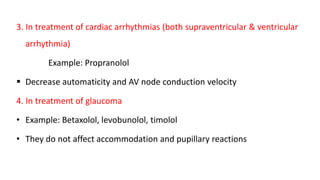
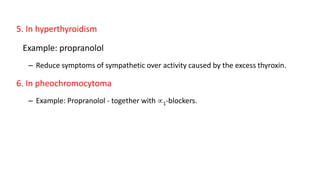
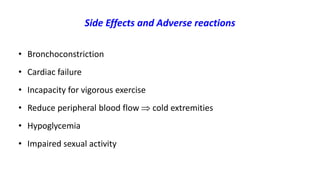
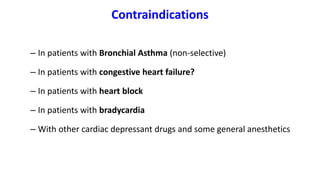
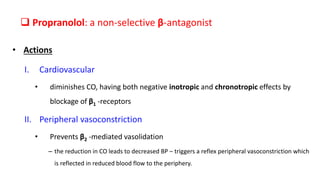
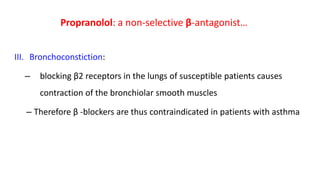
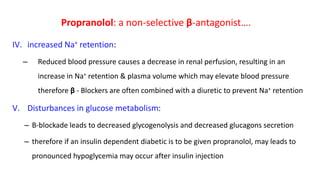
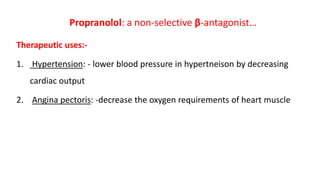
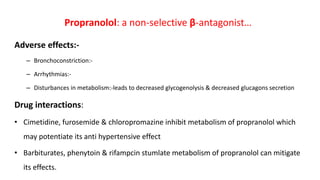
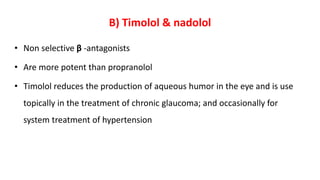
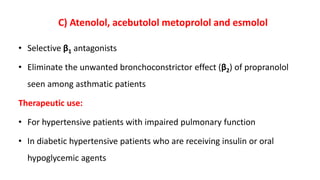
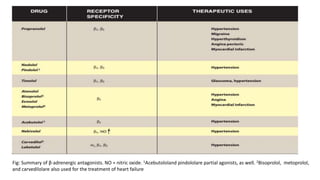
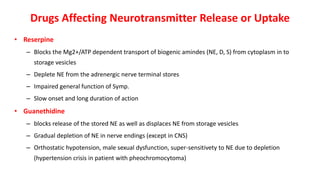
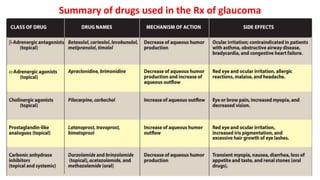
This document provides an extensive overview of adrenergic agonists and antagonists, detailing their classifications, mechanisms, and clinical applications. It describes the different types of adrenergic receptors, including α and β receptors, and discusses the pharmacokinetics and therapeutic uses of various sympathomimetic and antiadrenergic drugs. Additionally, it covers specific medications such as epinephrine, norepinephrine, dopamine, and their roles in treating conditions like hypertension, asthma, and cardiac arrest.