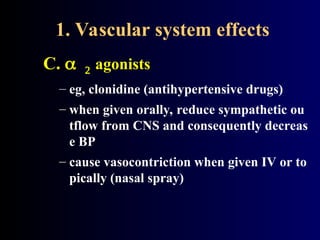
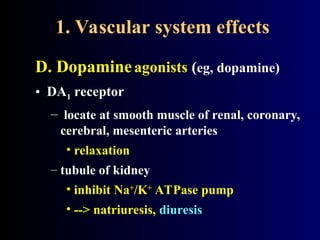
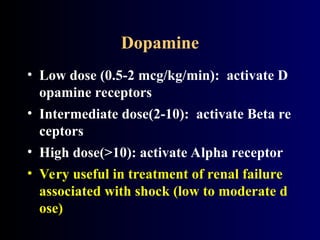
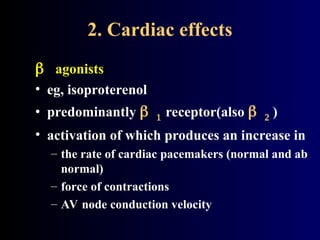
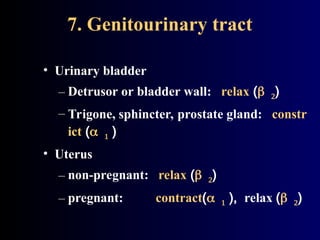
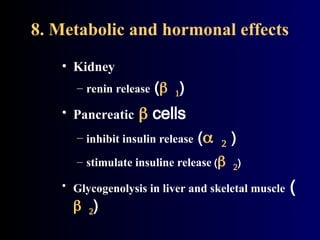
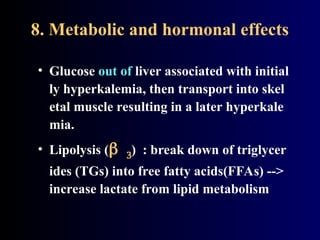
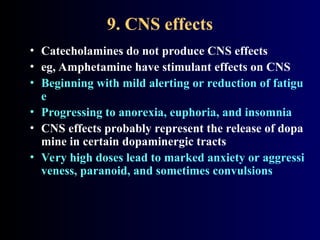
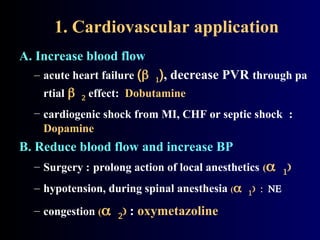
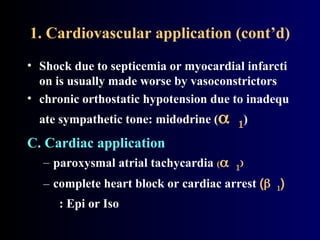
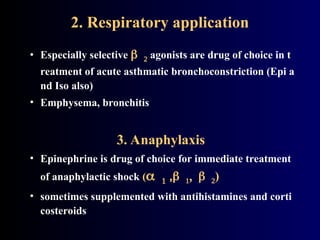
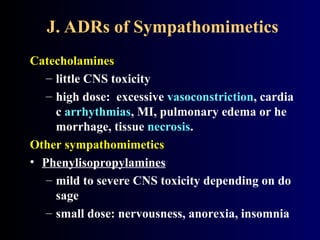
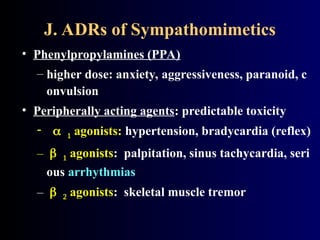
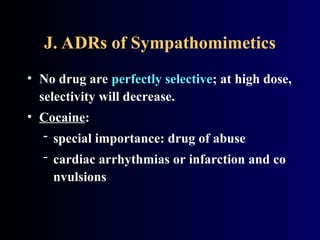
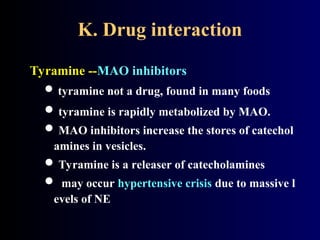
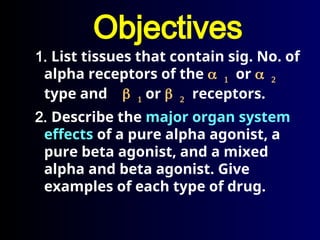
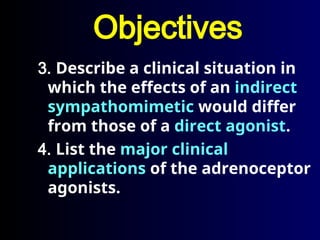
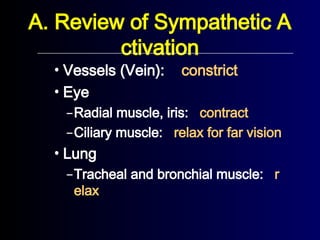
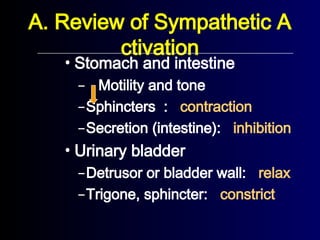
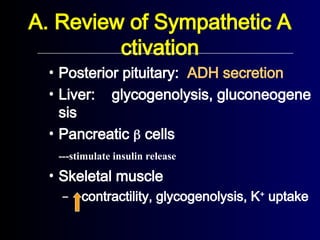
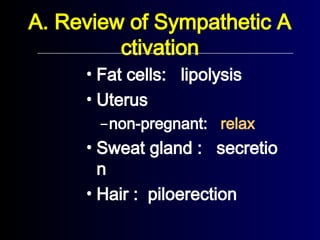
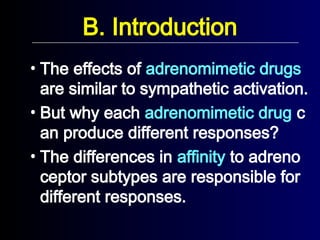
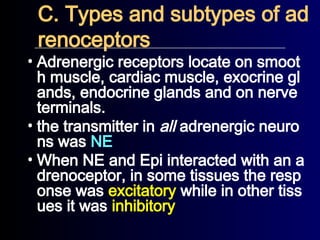
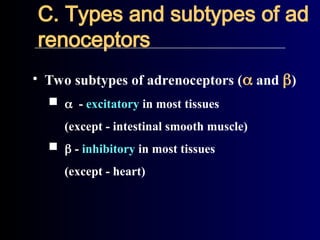
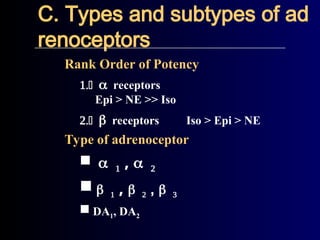
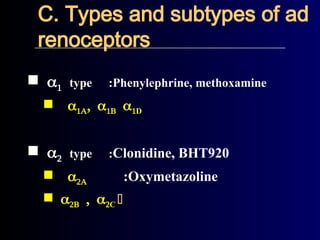
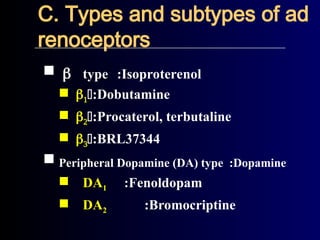
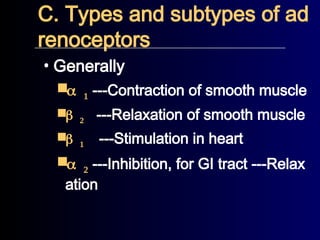
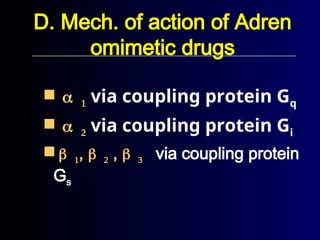
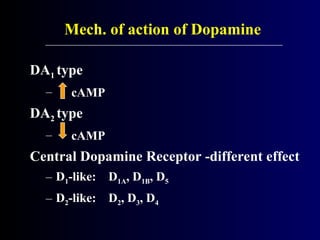
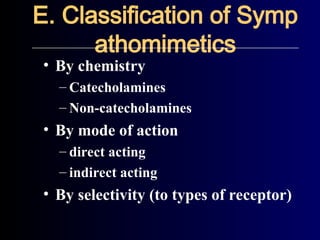
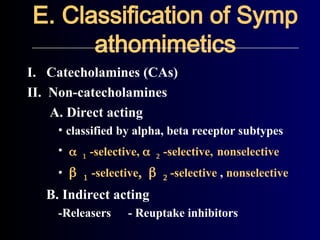
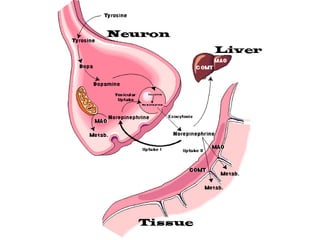
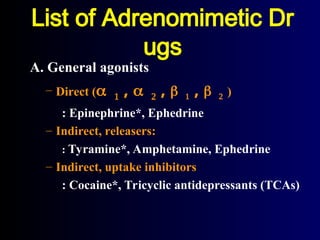
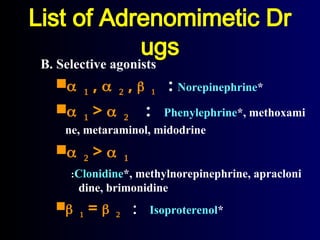
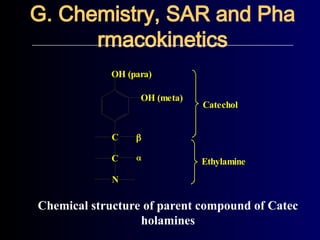
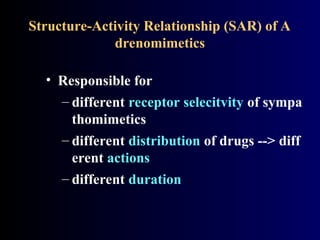
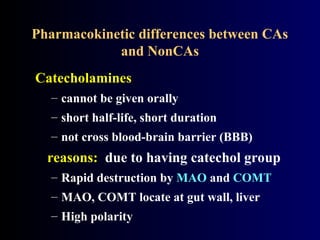
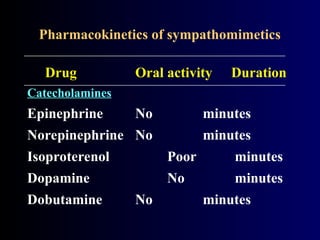
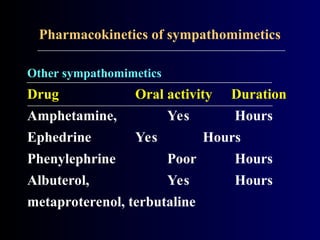
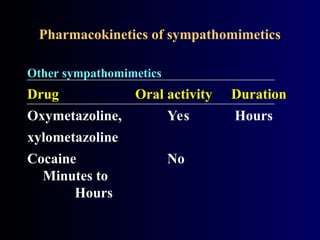
The document provides an extensive overview of sympathomimetic drugs, including their classifications, mechanisms of action, and effects on various organ systems. It outlines the roles of different adrenoceptors, the physiological responses elicited by synthetic and natural sympathomimetics, and their clinical applications along with potential side effects. It emphasizes the importance of receptor selectivity and the pharmacokinetics of different drug classes in therapeutic settings.

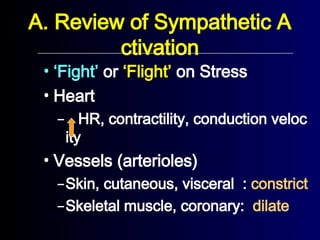
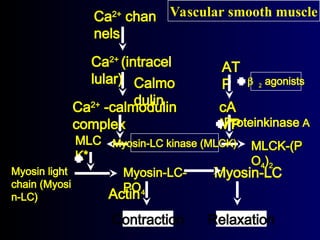
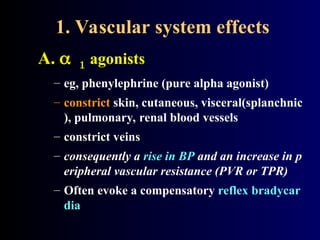
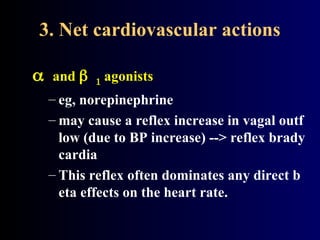
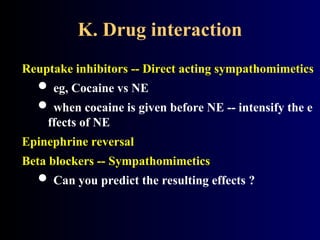
![1. Vascular system effects
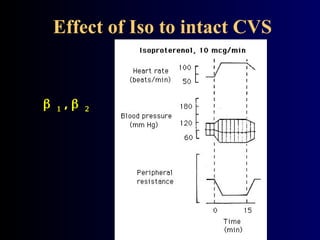
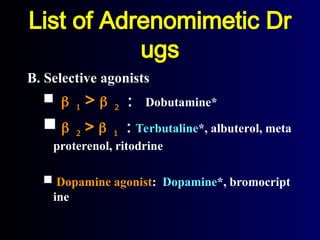
B. agonists
– eg, terbutaline (pure beta agonist)
– dilate arterioles in skeletal muscle, coronary arteries
– consequently reduce PVR and BP.
– [Voluntary muscle ----> tremor ()]
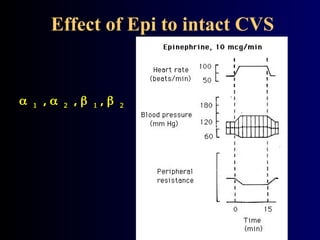
–Low dose of Epi: Beta2 activation is
dominant.](https://image.slidesharecdn.com/adrenergicagents1-240920121228-4426ebea/85/adrenergic_agents-1-hhhhhhhhhhhhhhhhh-ppt-42-320.jpg)