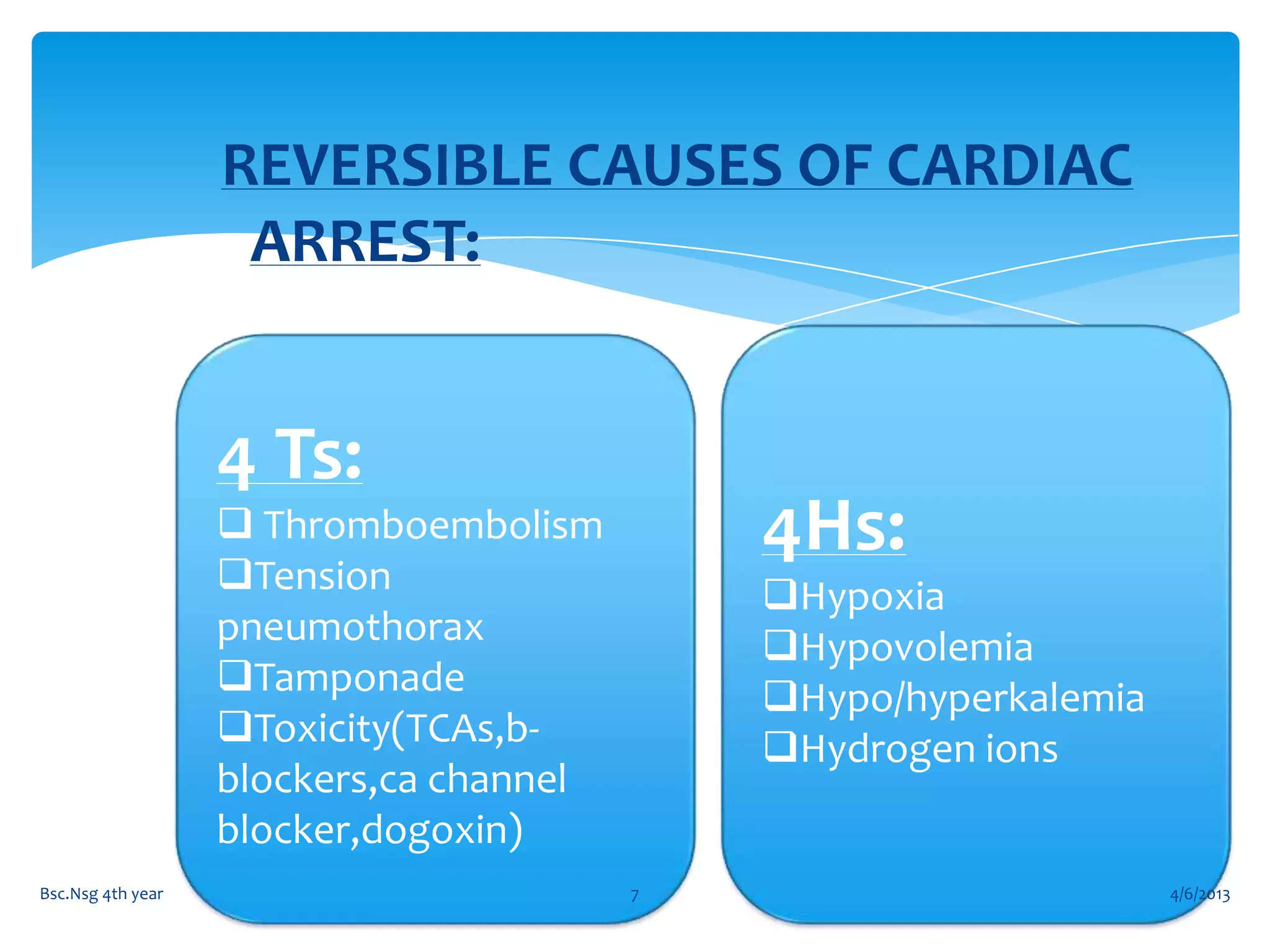
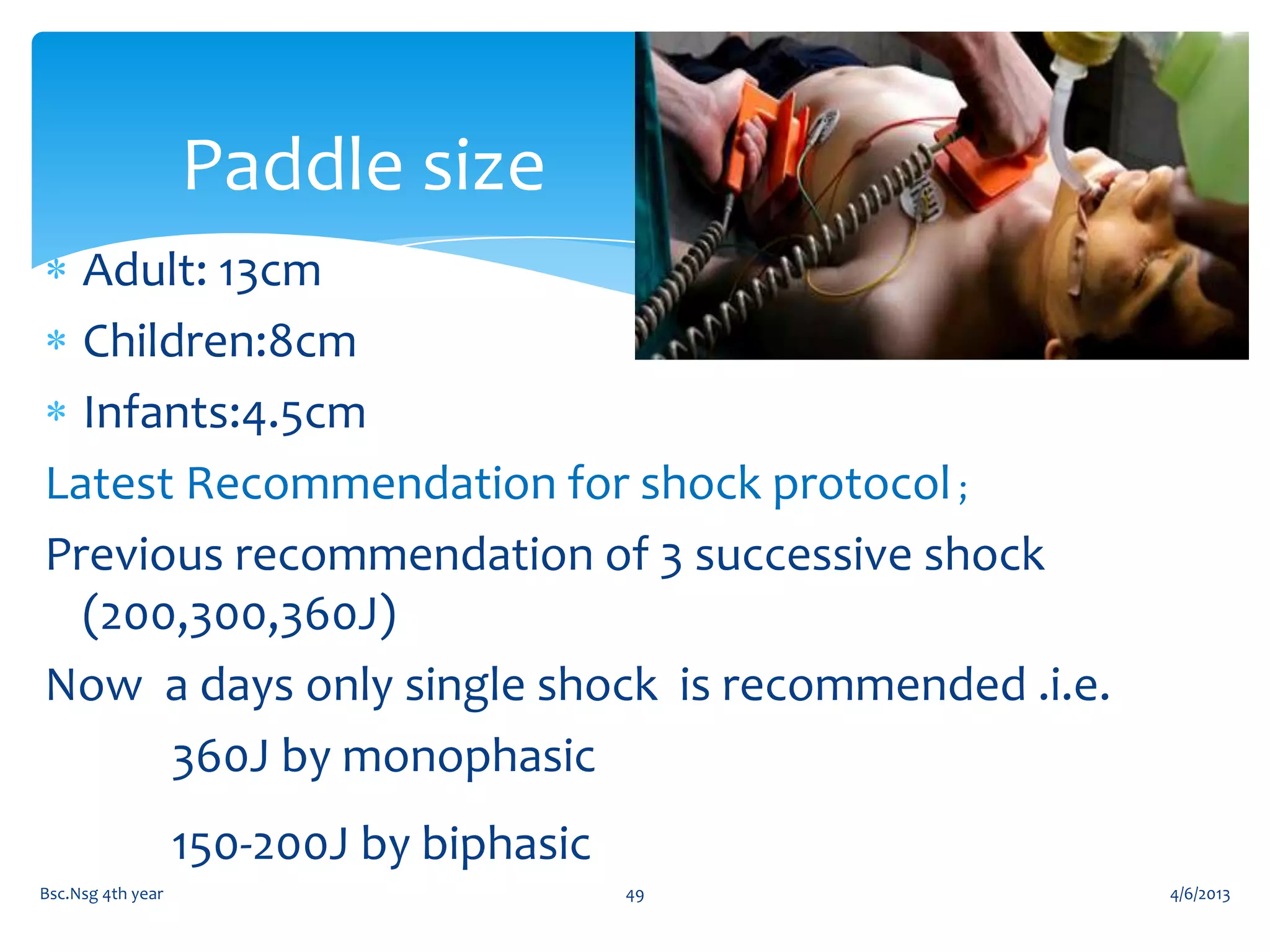
The document outlines an educational program on cardiac arrest for 4th year nursing students. The objectives are to review cardiac arrest, basic life support, advanced life support, and demonstrate skills like basic life support, airway insertion, and defibrillation. The program agenda includes topics on cardiac arrest, basic and advanced life support, defibrillation, drugs used in advanced life support, and demonstrations of skills. It provides details on cardiac arrest, basic life support procedures like chest compressions and rescue breathing, and advanced life support including defibrillation and drugs.