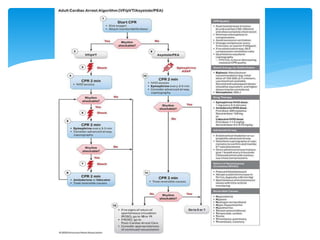
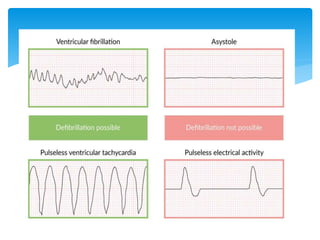
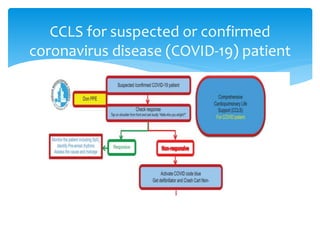
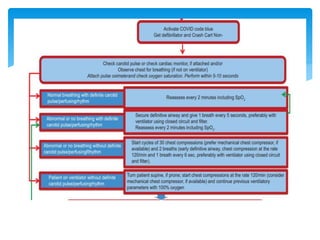
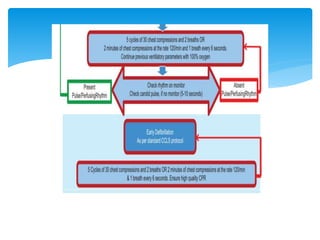
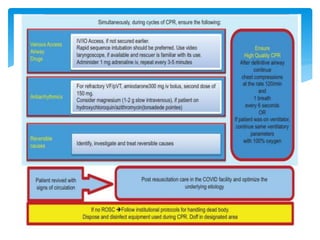
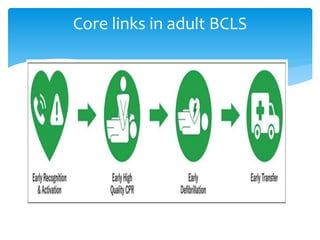
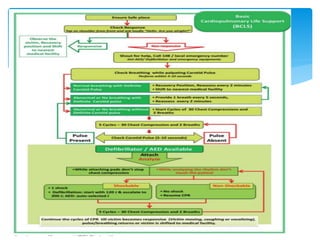
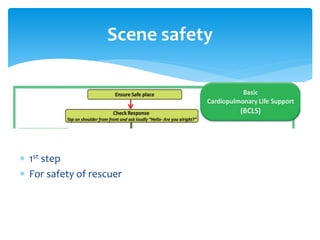
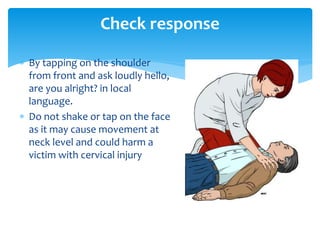
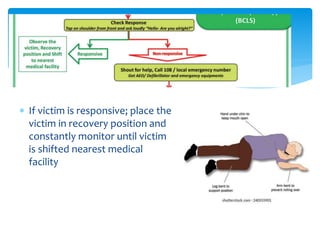
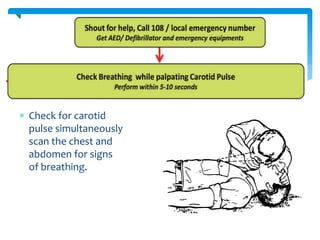
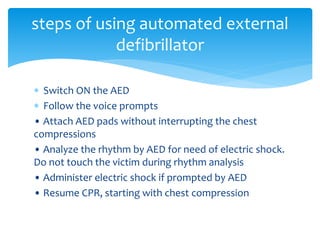
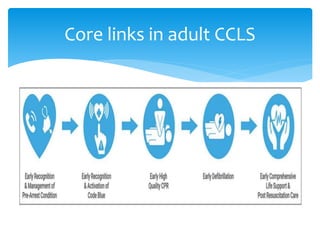
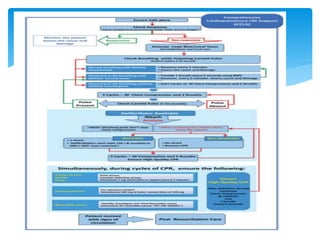
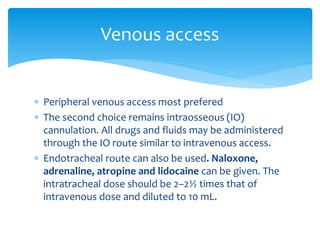
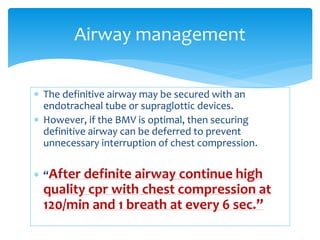
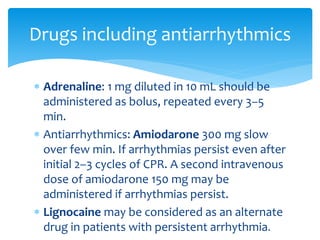
This document discusses basic and advanced cardiovascular life support. It defines cardiac arrest as the sudden cessation of heart function and outlines the management of out-of-hospital and in-hospital cardiac arrest. For out-of-hospital cardiac arrest, it describes the steps of basic cardiopulmonary life support including calling for help, checking response, pulse and breathing, performing chest compressions and rescue breathing, using an automated external defibrillator, and positioning the victim for recovery. For in-hospital cardiac arrest, it outlines the steps of comprehensive cardiopulmonary life support including establishing intravenous access, airway management, medication administration, and treating reversible causes of arrest.
![ ‘HIT THE TARGET’
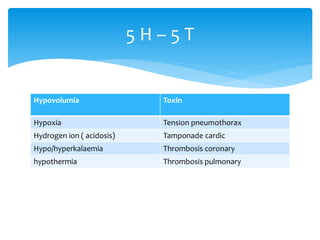
• H – Hypoxia,
• I – Increased H Ions [Acidosis],
• T – Tension Pneumothorax,
• T – Toxins/Poisons
• H – Hypovolaemia,
• E – Electrolyte Imbalance [Hypo-/Hyperkalaemia],
• T – Tamponade Cardiac,
• A – Acute Coronary Syndrome,
• R – Raised Intracranial Pressure [Subarachnoid Haemorrhage],
• G – Glucose [Hypo-/hyperglycaemia],
• E – Embolism (Pulmonary Thrombosis),
• T – Temperature [Hypothermia]).
Assess and manage the reversible
causes](https://image.slidesharecdn.com/basicandadvancecardiaclifesupport-220215144903/85/Basic-and-advance-cardiac-life-support-38-320.jpg)