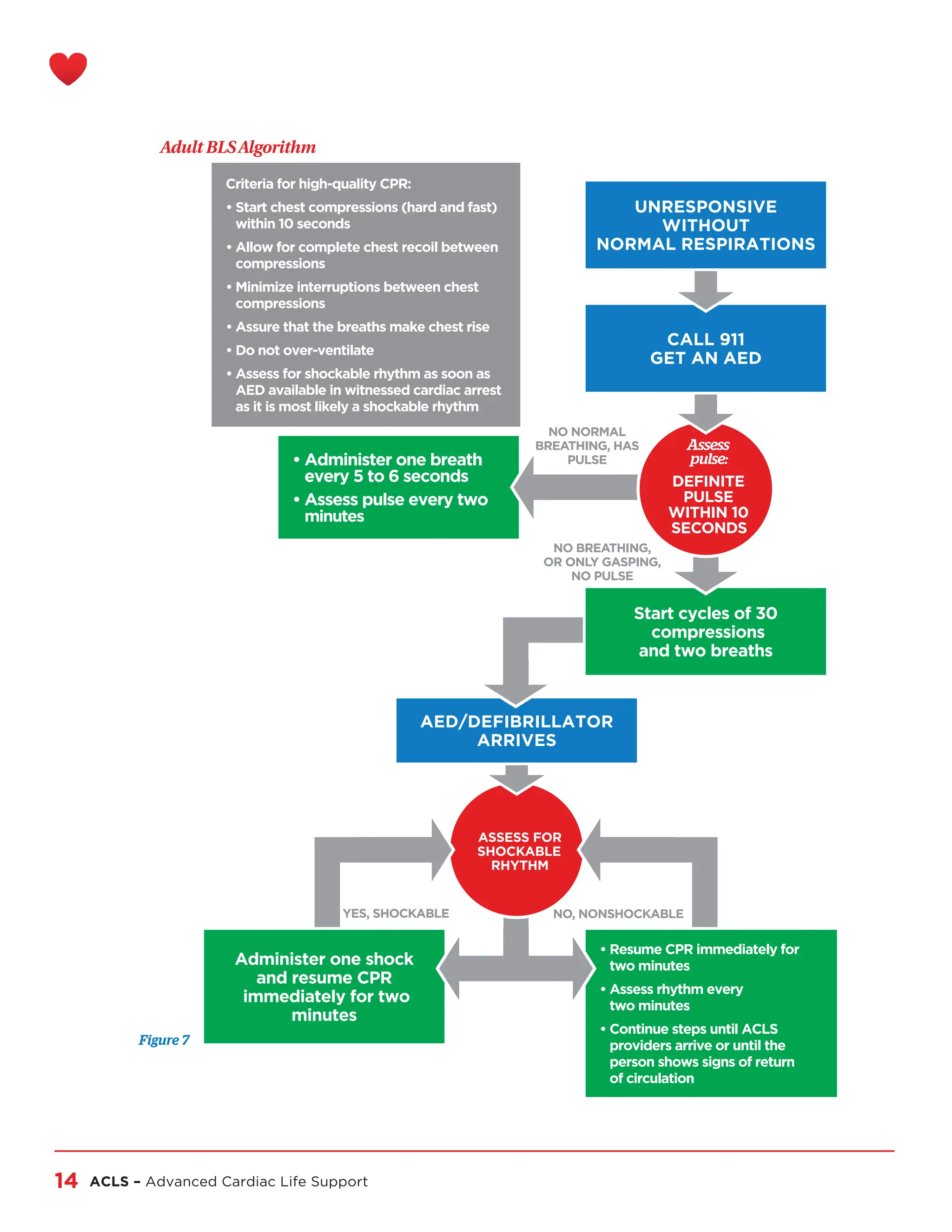
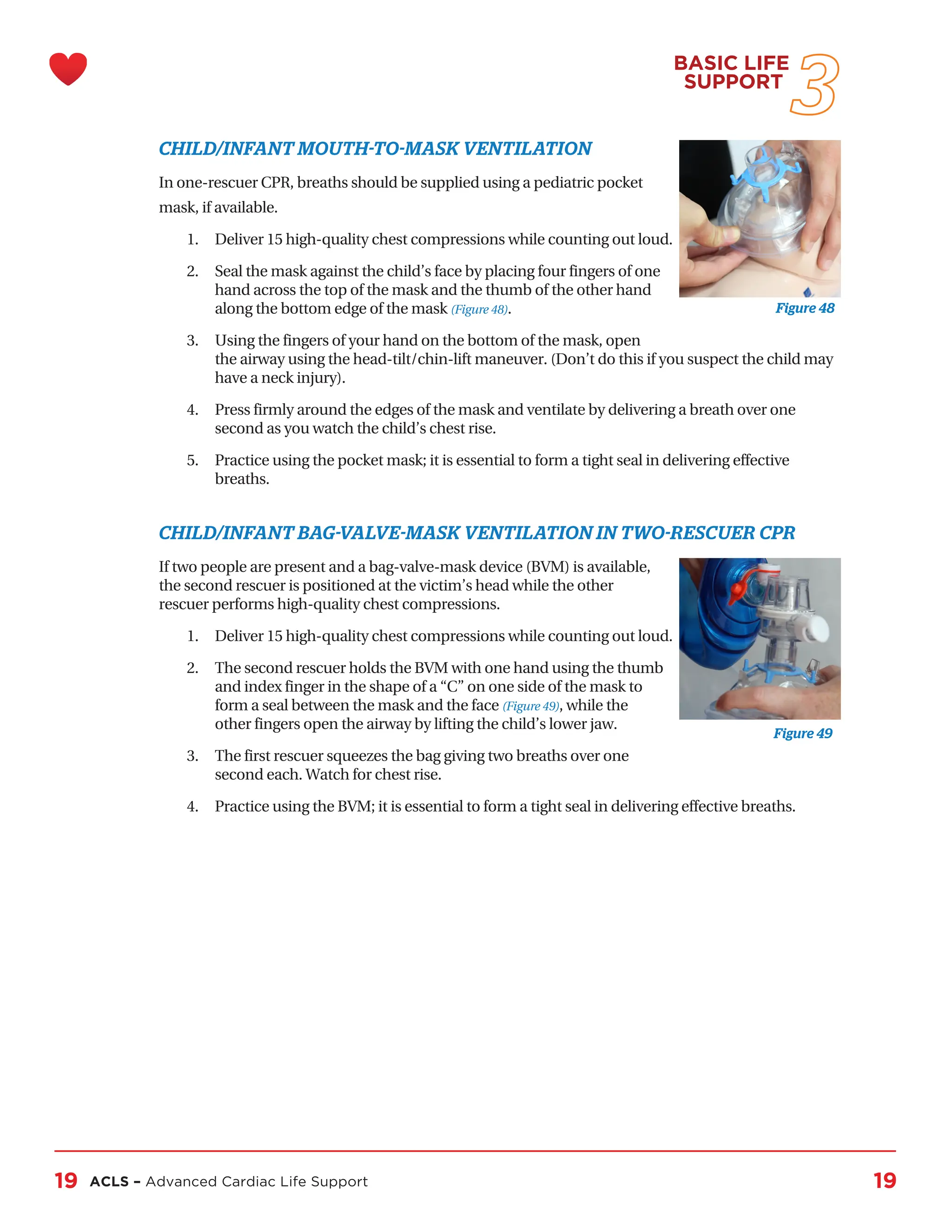
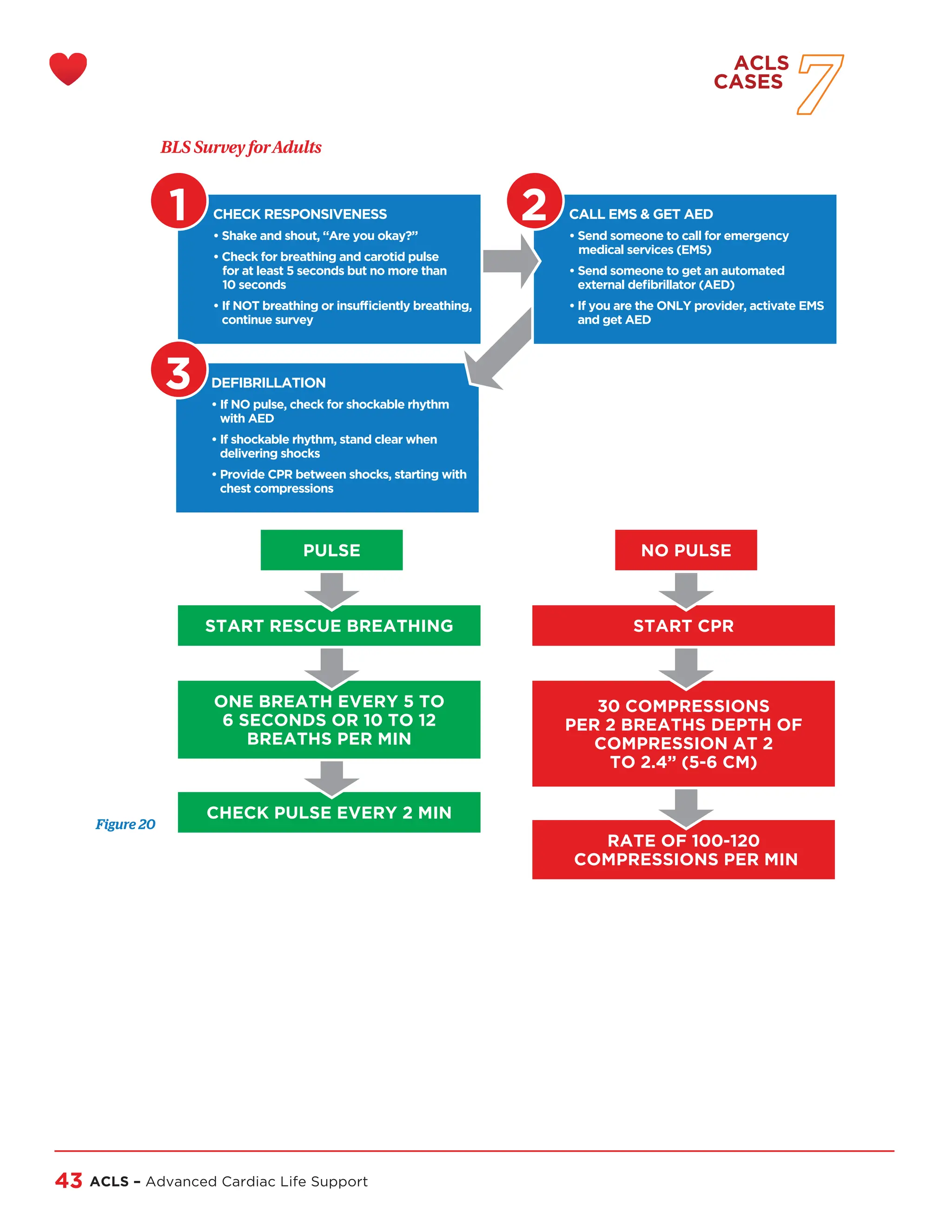
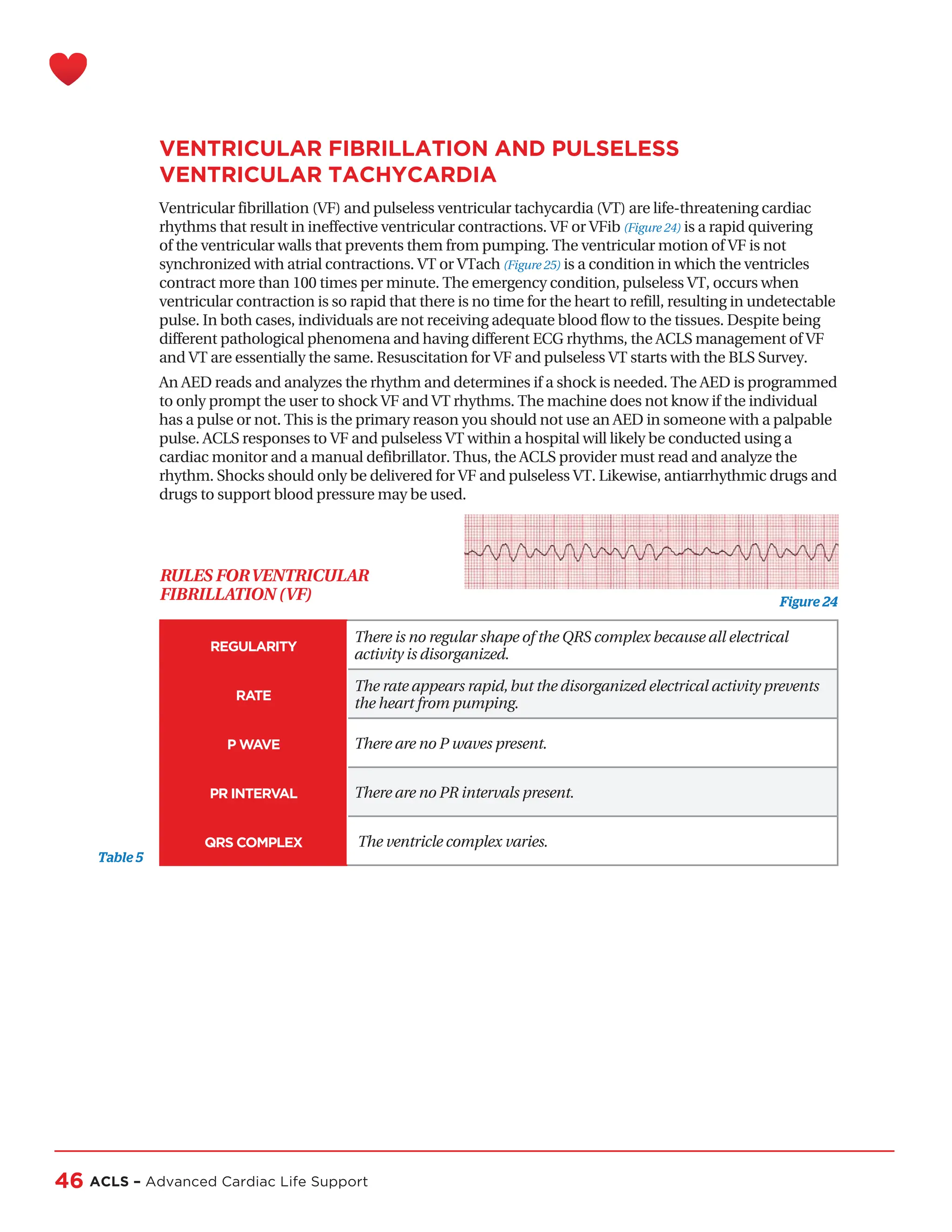
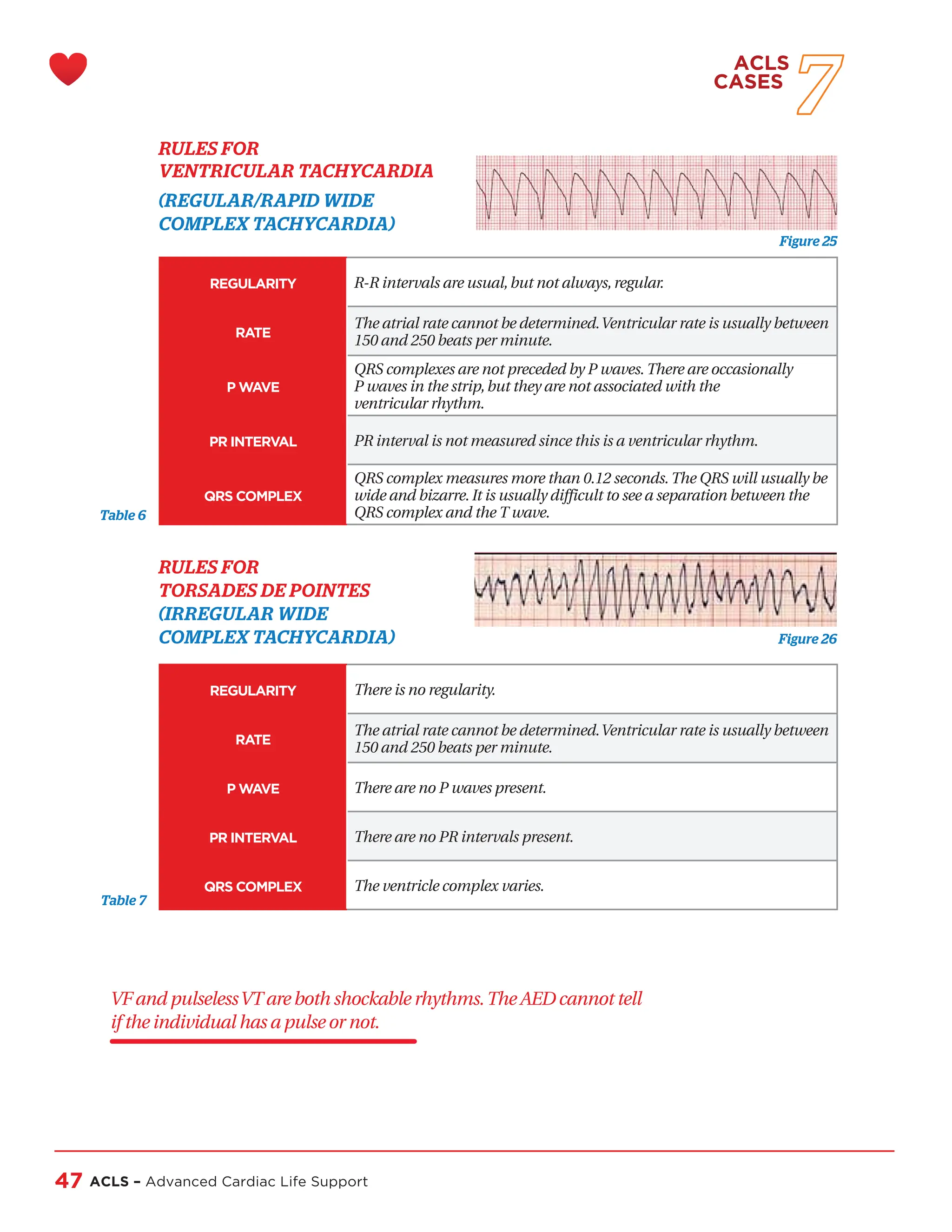
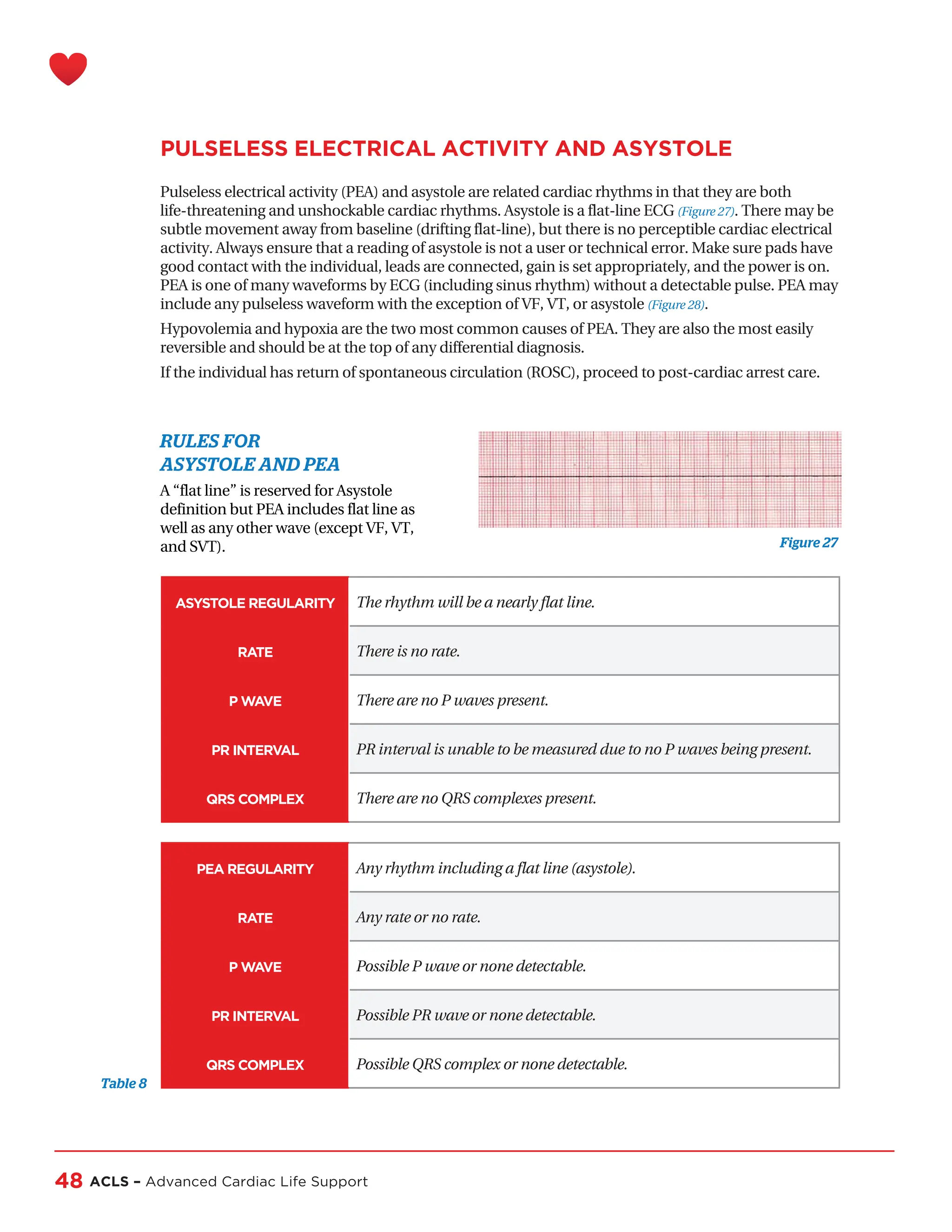
The document is the Advanced Cardiac Life Support (ACLS) Provider Handbook, detailing guidelines and protocols for responding to life-threatening cardiac events. It emphasizes the importance of early intervention, proper assessment, and the systematic application of both Basic Life Support (BLS) and ACLS protocols to improve patient outcomes. Updated guidelines from the International Liaison Committee on Resuscitation (ILCOR) are included to ensure that healthcare providers apply the most current practices in emergency situations.