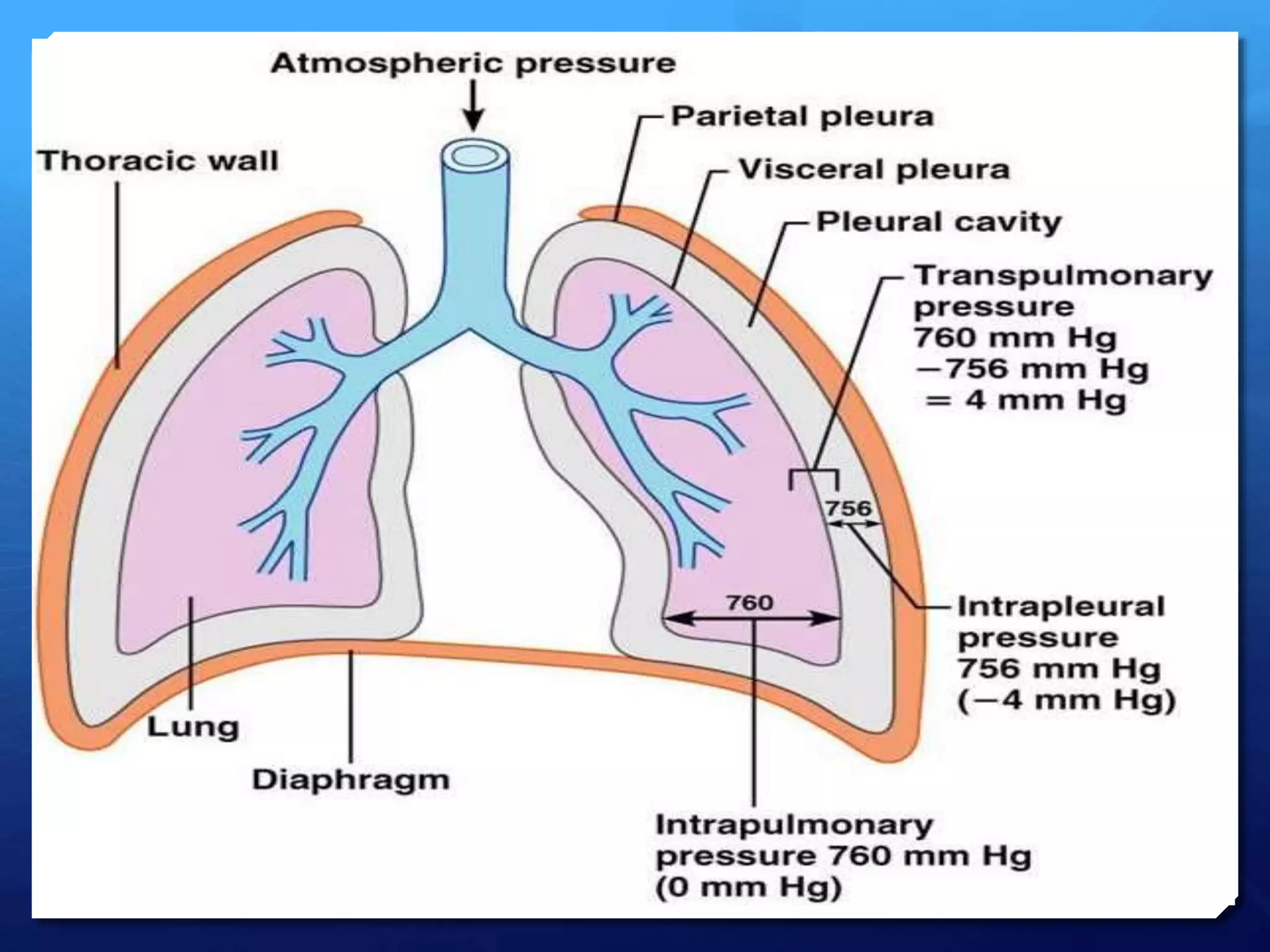
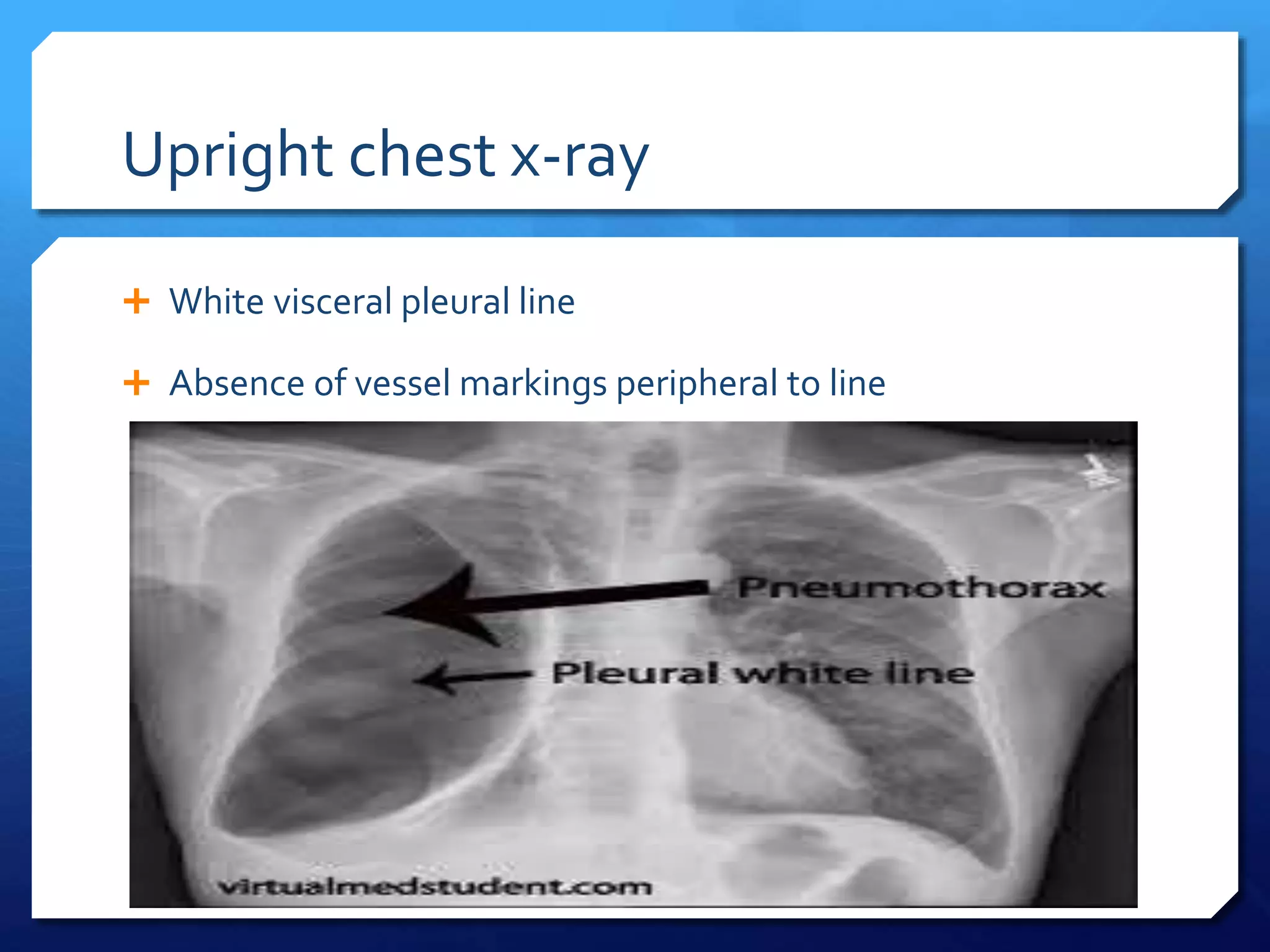
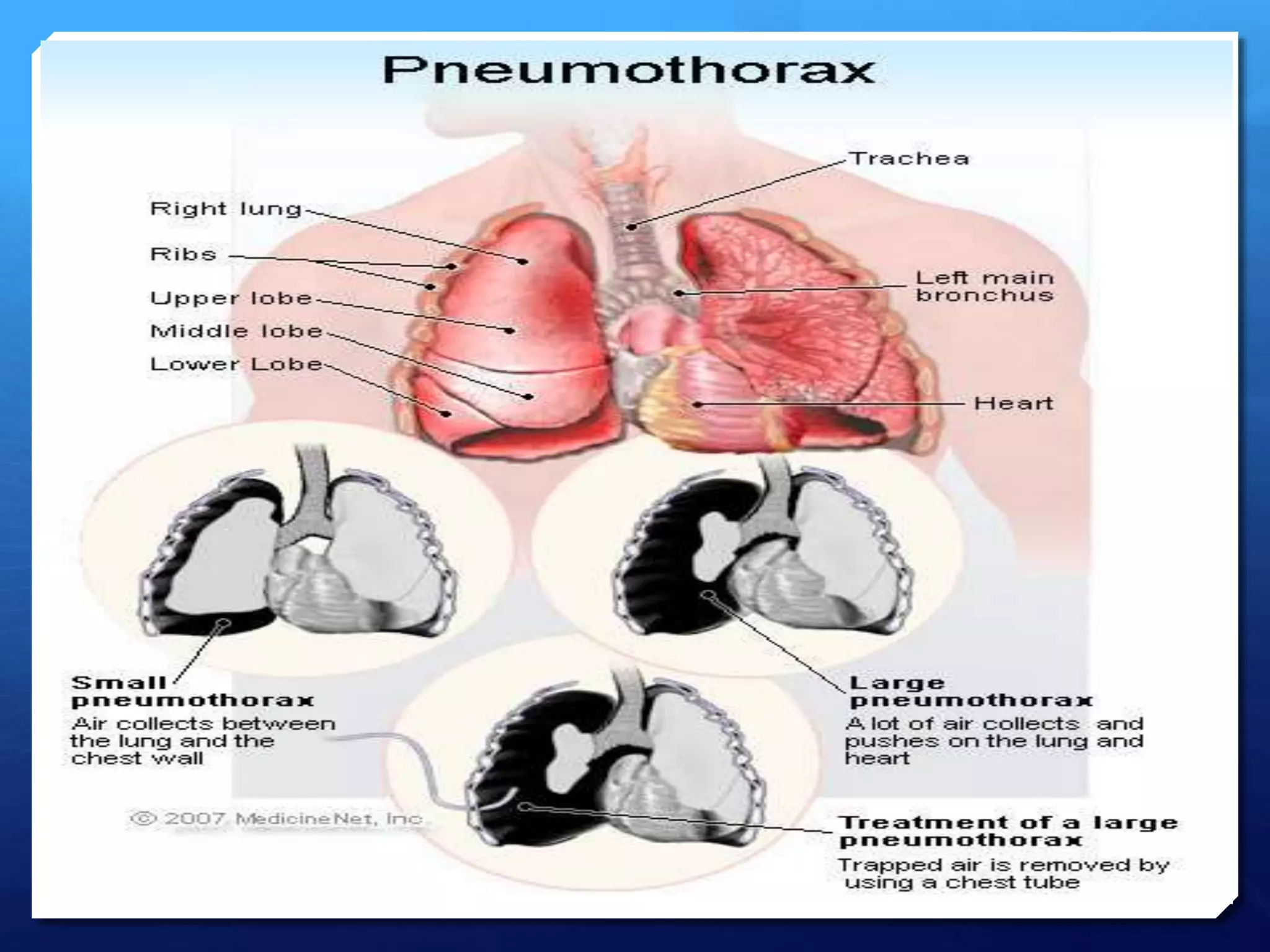
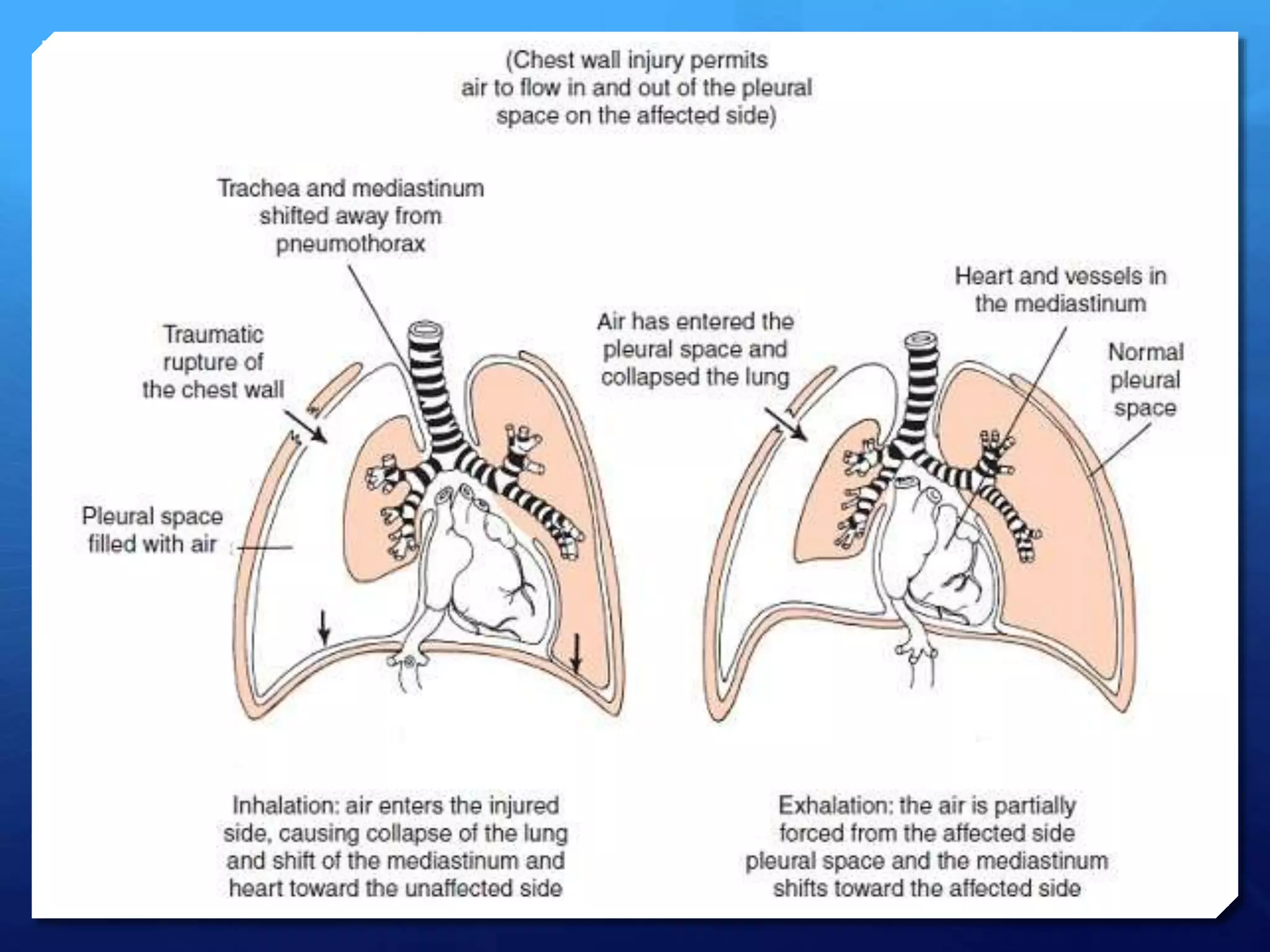
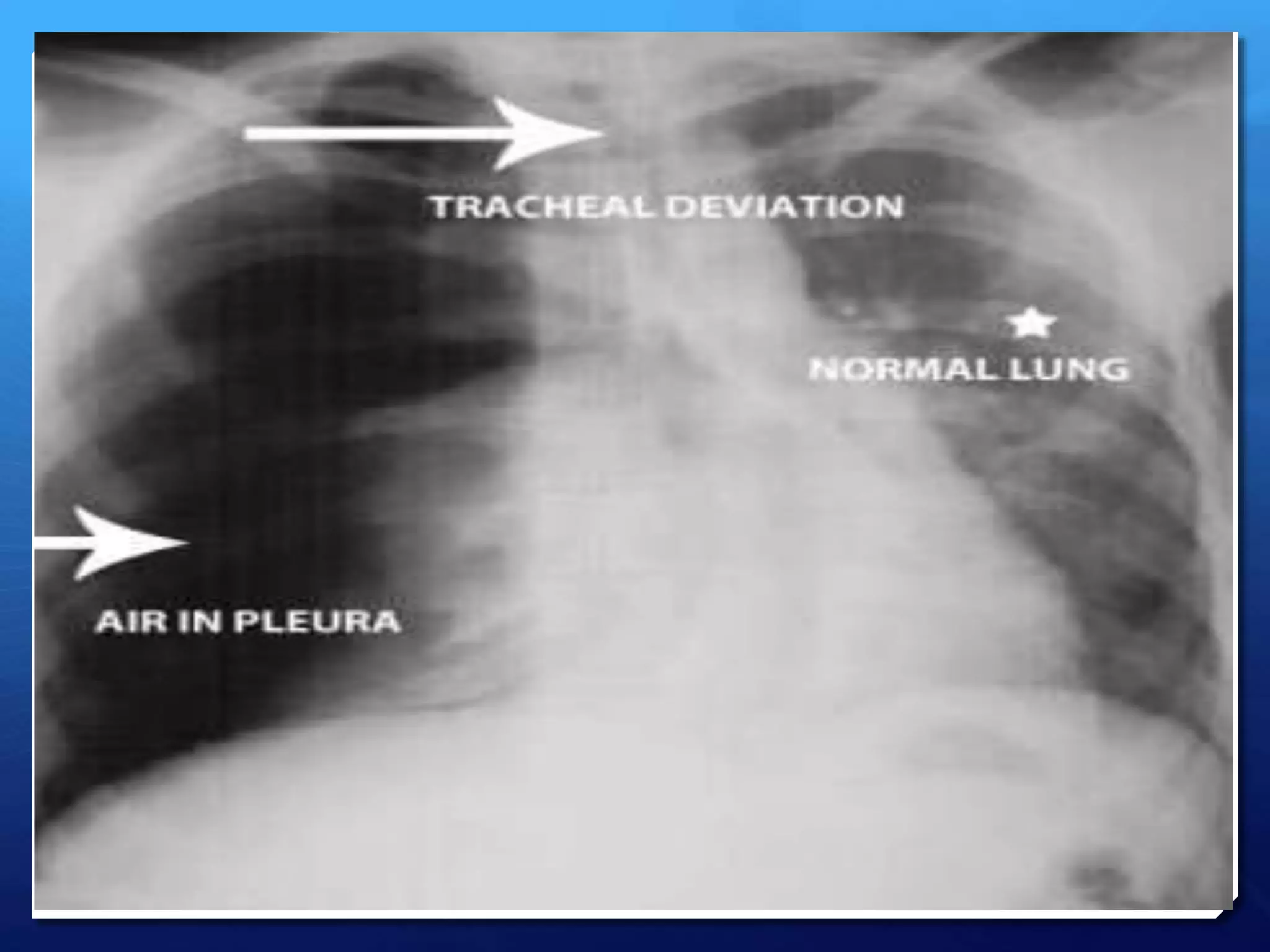
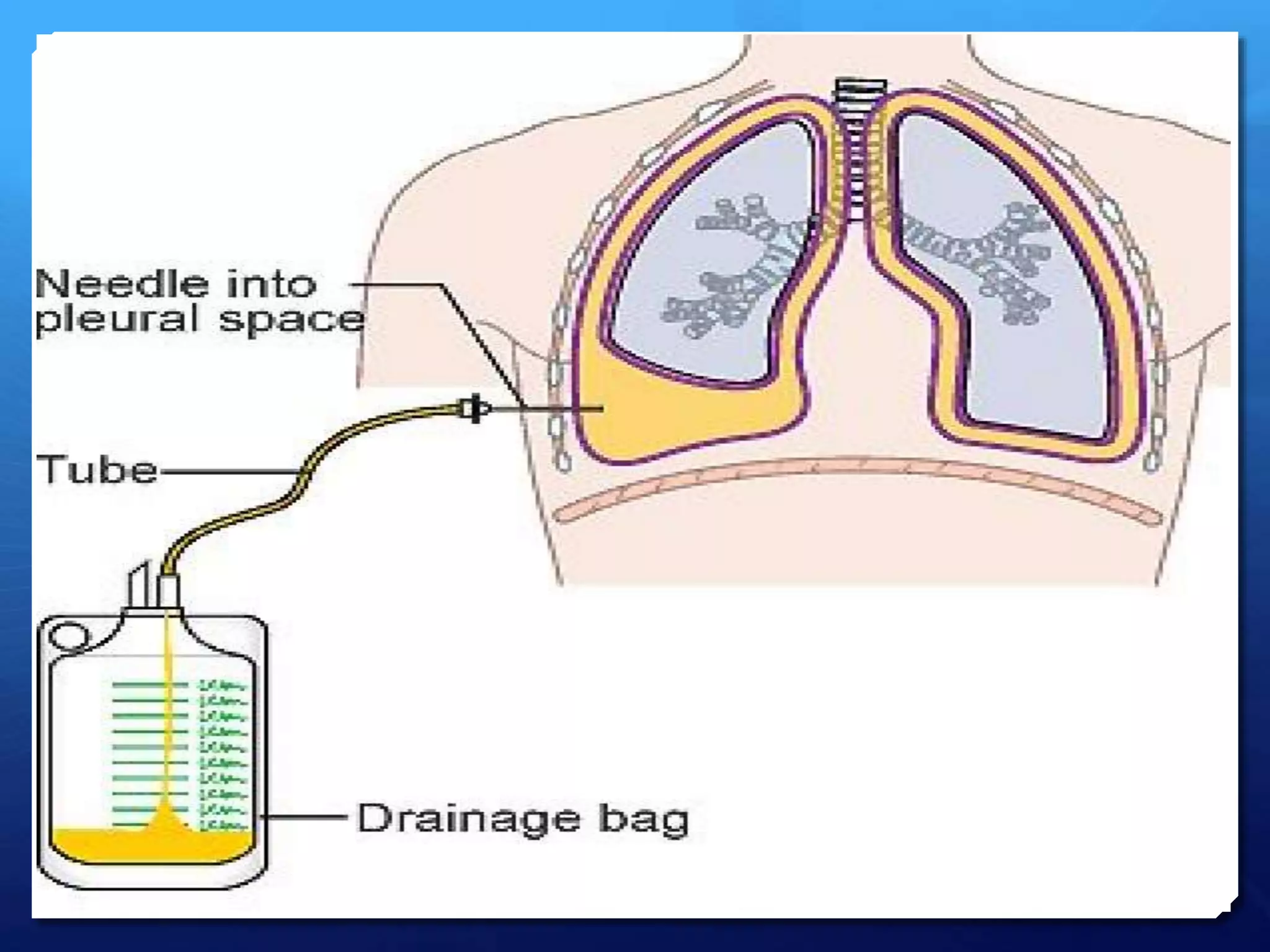
This document discusses pneumothorax and hemothorax. It defines pneumothorax as a collection of air in the pleural space, which can be spontaneous or traumatic. Tension pneumothorax is a life-threatening condition where air builds up pressure in the pleural space. Hemothorax is defined as a collection of blood in the pleural space. The document covers causes, pathogenesis, clinical presentations, and treatment approaches for pneumothorax and hemothorax.