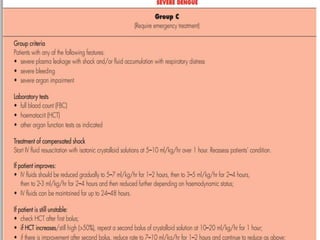
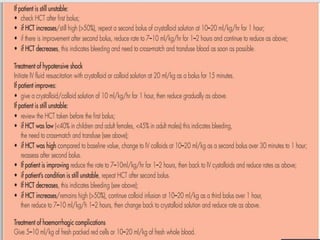
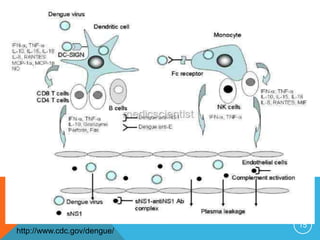
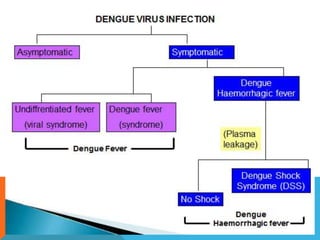
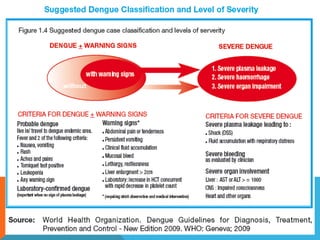
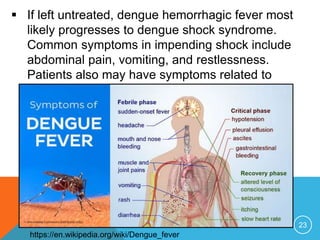
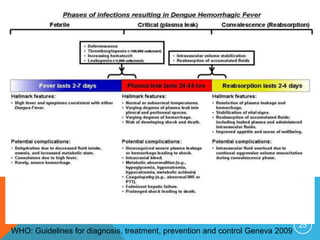
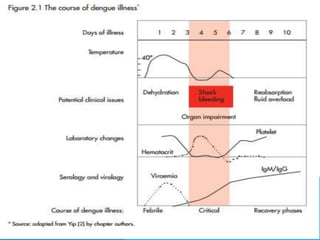
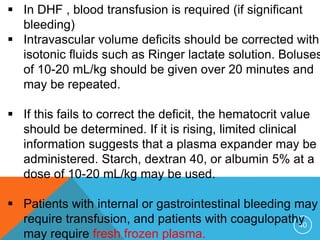
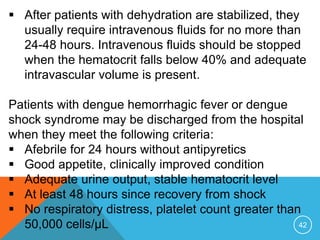
This document provides an overview of dengue fever, including its epidemiology, etiology, pathophysiology, classification, clinical presentation, diagnosis, management, prevention, and vaccines. Dengue fever is caused by infection with one of four dengue virus serotypes and transmitted by Aedes mosquitoes. It presents as an acute febrile illness and can develop into severe dengue hemorrhagic fever or dengue shock syndrome in some cases. Diagnosis involves virus or antibody detection tests. Management focuses on treatment of symptoms, and prevention through mosquito control measures and vaccine development.



![48
Vaccines :
No vaccine is currently approved for the prevention
of dengue infection.
Because immunity to a single dengue strain is the
major risk factor for dengue hemorrhagic fever and
dengue shock syndrome, a vaccine must provide
high levels of immunity to all 4 dengue strains to be
clinically useful.
Tetravalent LA dengue virus strains based on yellow
fever –dengue virus [CYD-TDV]
Future directions : TV003 a single dose of LATV –
induced a trivalent or greater Nab response in 90%
of flavivirus-naive adults](https://image.slidesharecdn.com/denguefever-160122140425/85/Dengue-fever-presentation-48-320.jpg)