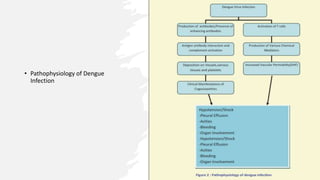
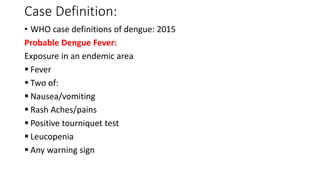
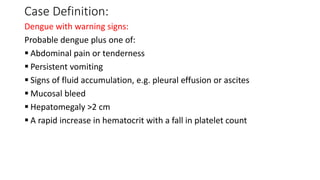
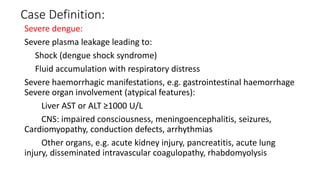
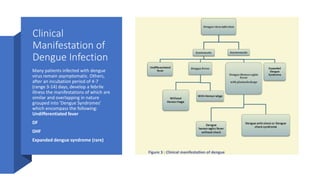
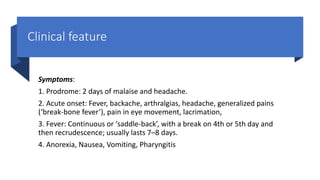
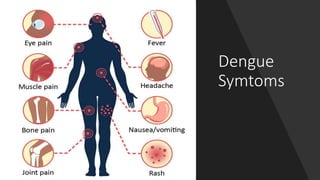
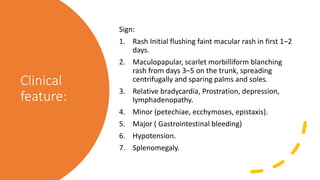
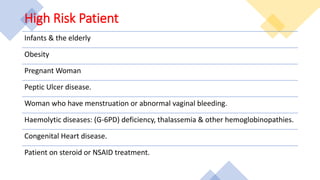
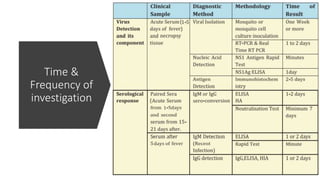
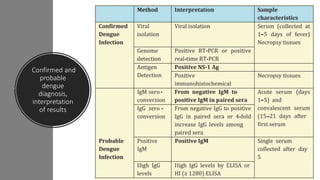
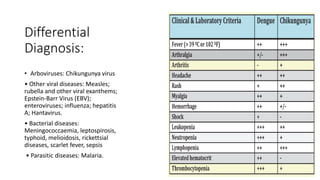
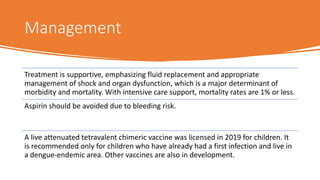
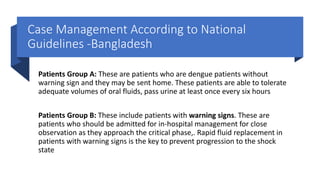
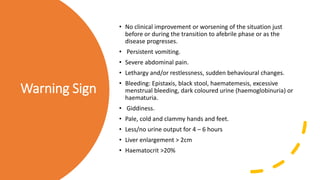
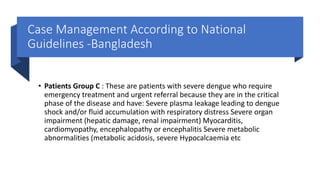
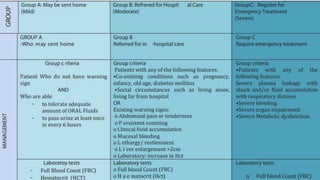
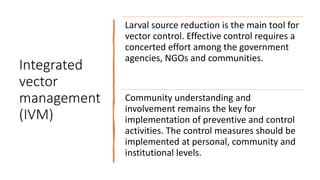
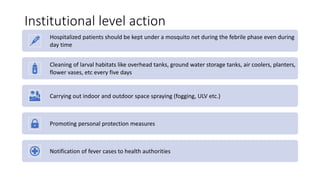
The document provides an extensive overview of dengue fever, an acute viral disease transmitted by Aedes mosquitoes, highlighting its epidemiology, transmission, clinical presentation, diagnosis, and management. It underscores the significance of vector control, community involvement in prevention, and outlines various patient management groups based on severity of symptoms. Additionally, it discusses the recommendations for vaccine usage and integration of preventive measures at household and community levels to combat dengue outbreaks.