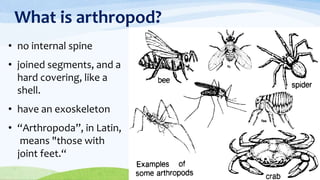
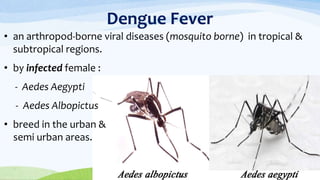
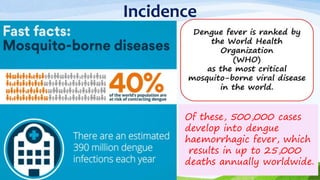
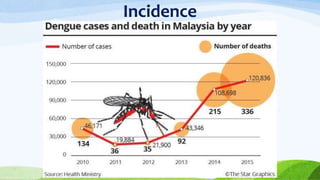
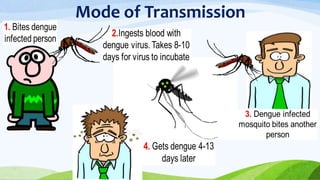
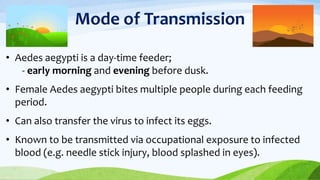
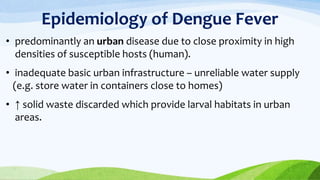
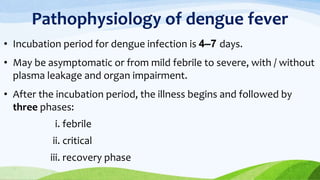
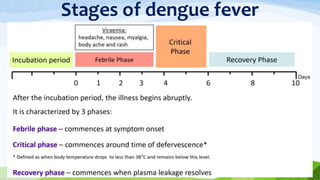
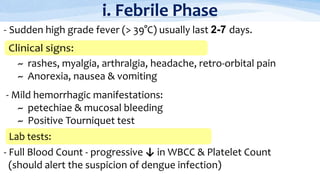
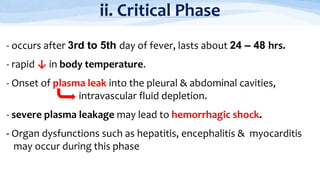
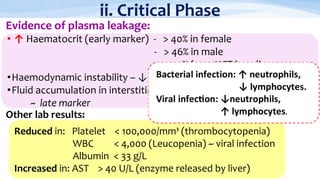
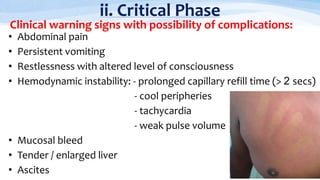
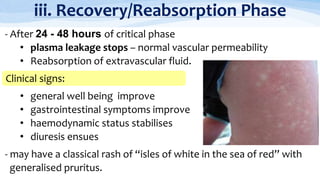
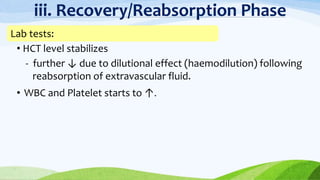
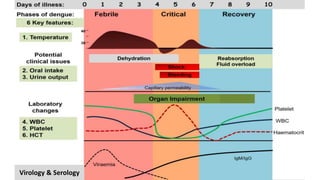
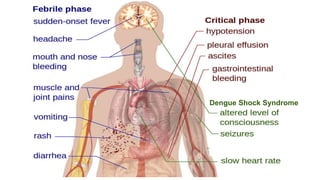
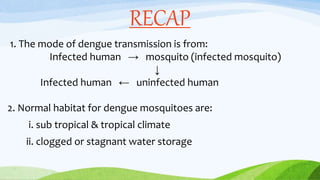
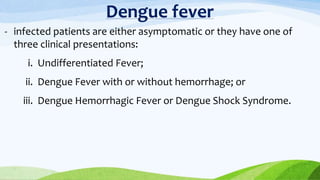
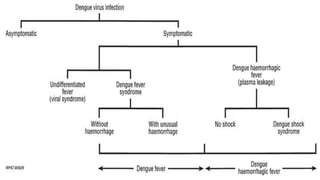
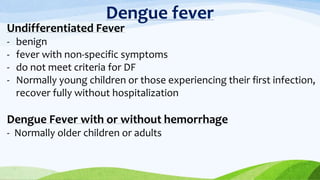
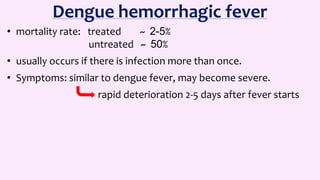
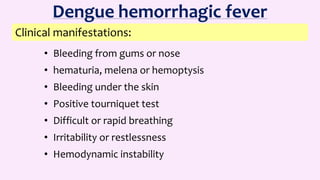
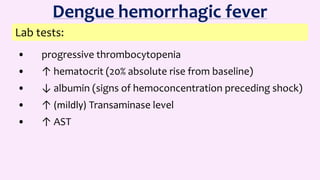
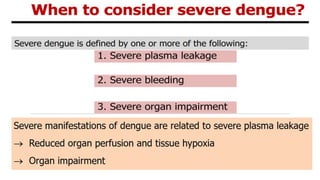
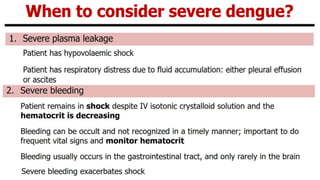
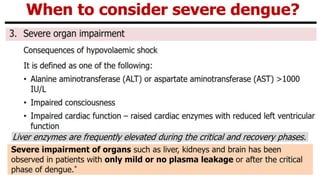
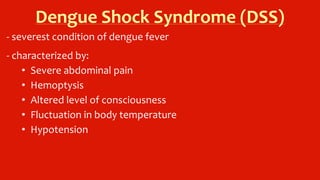
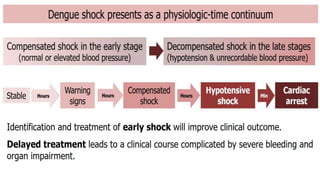
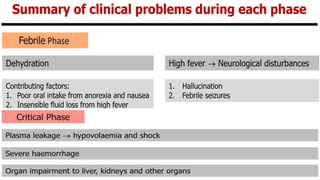
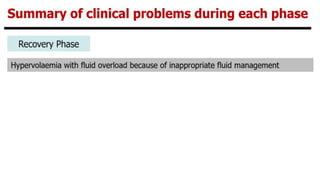
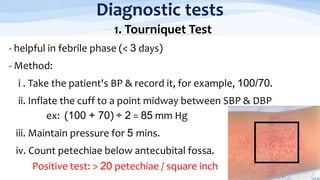
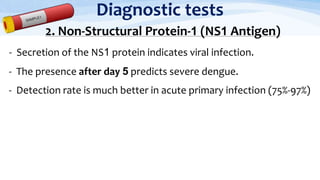
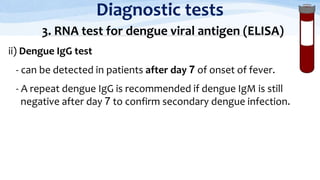
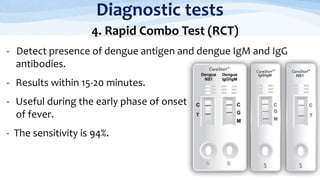
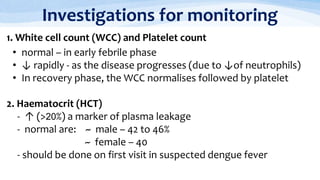
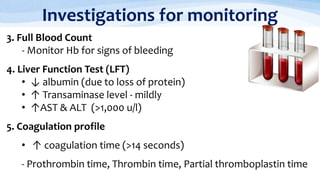
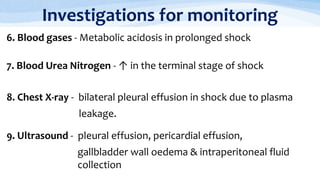
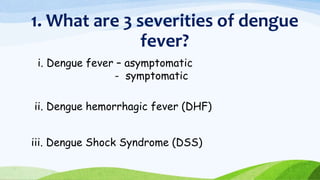
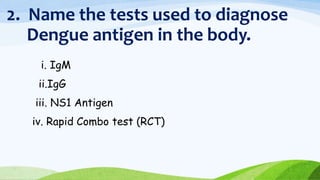
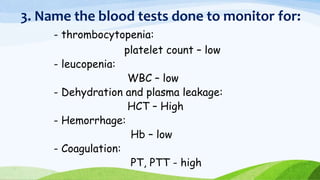
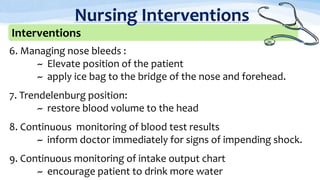
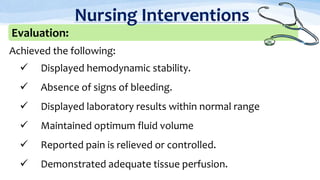
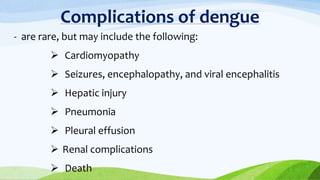
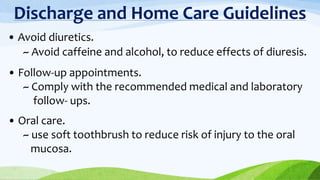
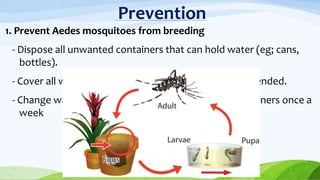
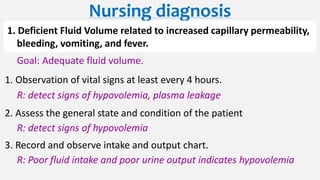
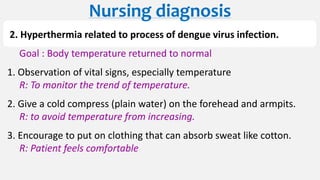
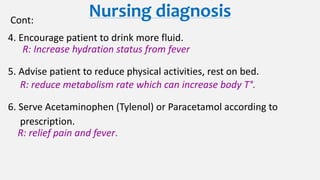
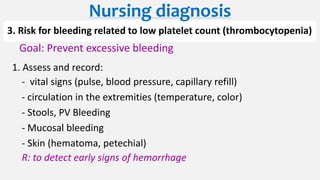
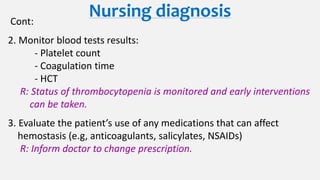
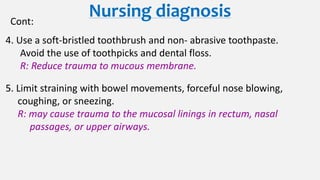
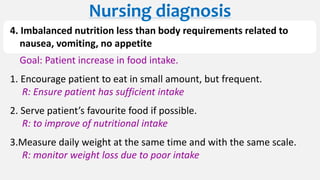
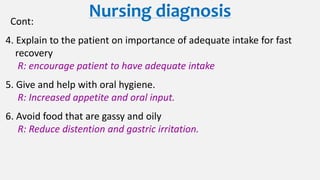
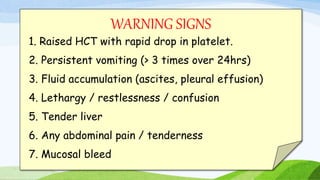
The document provides a detailed overview of dengue fever, including its definition, pathophysiology, clinical manifestations, diagnosis, and management strategies. It outlines the various stages of the disease, transmission methods, and the importance of nursing interventions for patient care. Additionally, it emphasizes preventive measures and outlines complications associated with dengue hemorrhagic fever and shock syndrome.