This document provides information on Dengue fever, including:
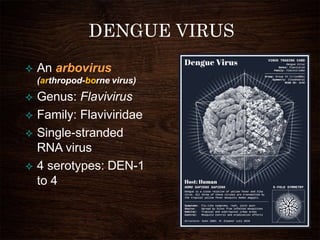
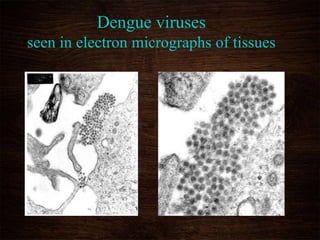
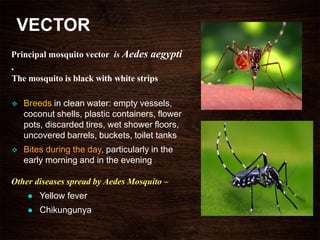
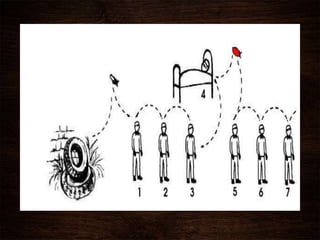
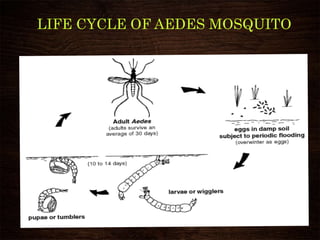
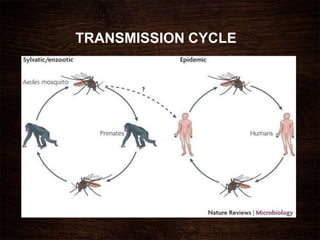
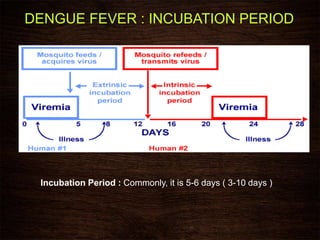
- It is caused by Dengue viruses 1-4 and transmitted by Aedes mosquitoes. Infection provides lifetime immunity to one serotype but not others.
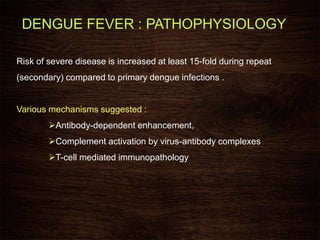
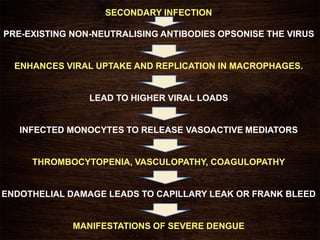
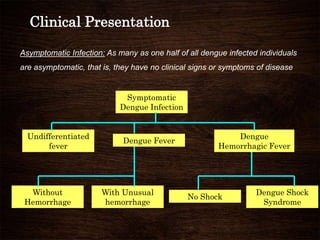
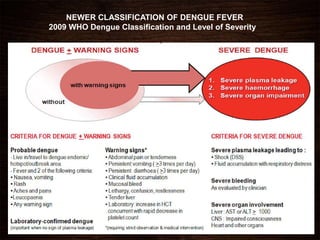
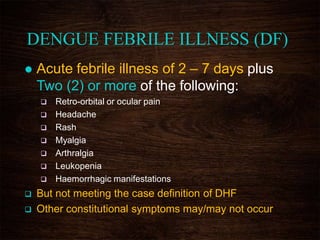
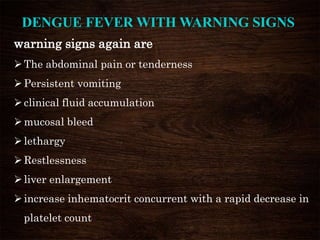
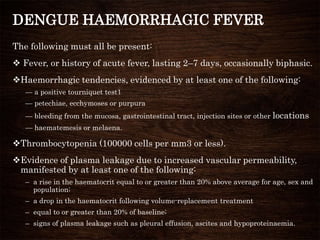
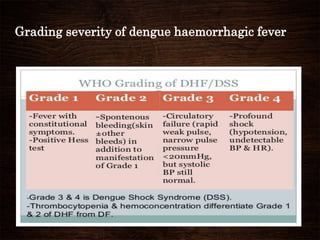
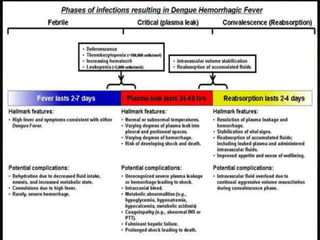
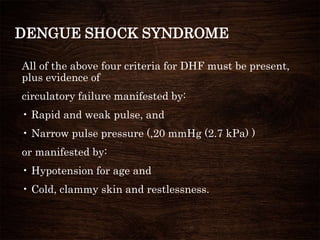
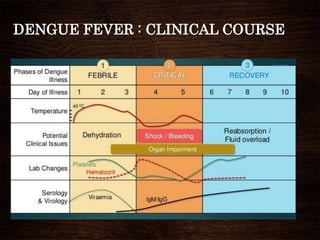
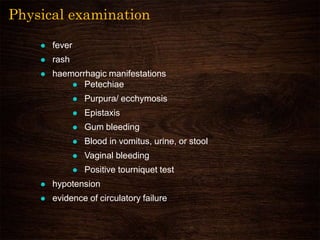
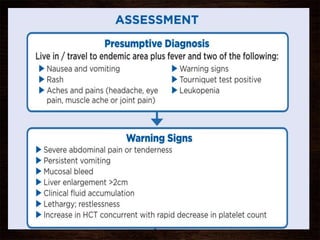
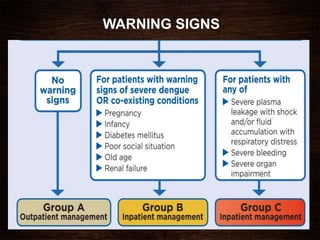
- Symptoms range from mild fever to severe dengue hemorrhagic fever/dengue shock syndrome. Secondary infections carry higher risk of severe disease.
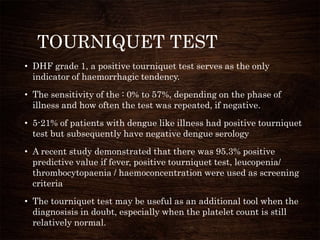
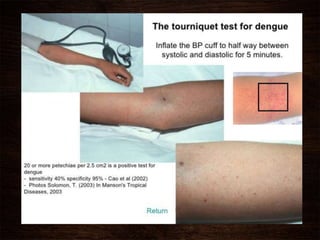
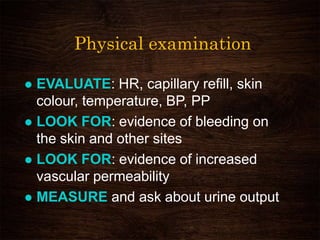
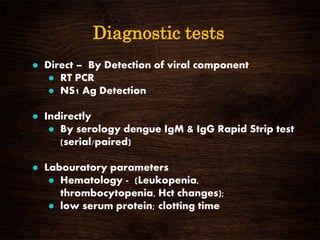
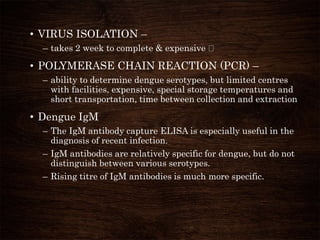
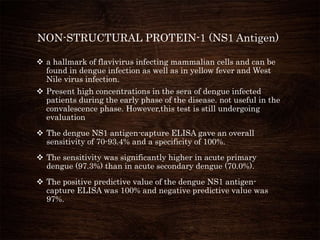
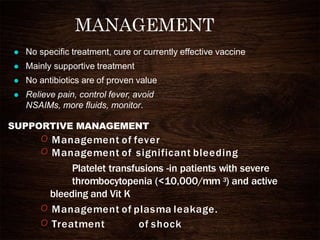
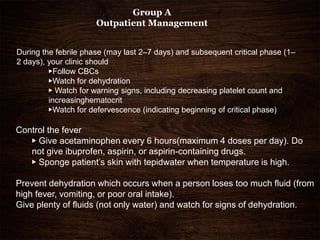
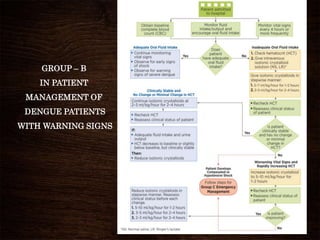
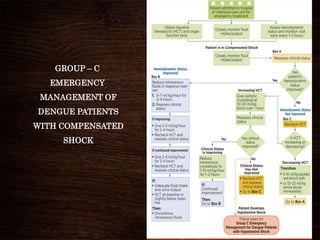
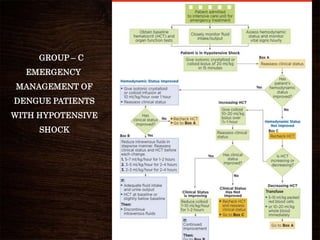
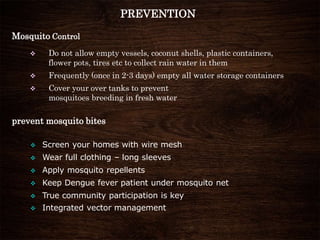
- Diagnosis involves physical exam, laboratory tests like platelet count and serology. There is no vaccine or antiviral treatment, only supportive care like fluids and fever control. Prevention focuses on mosquito control and avoidance of bites.