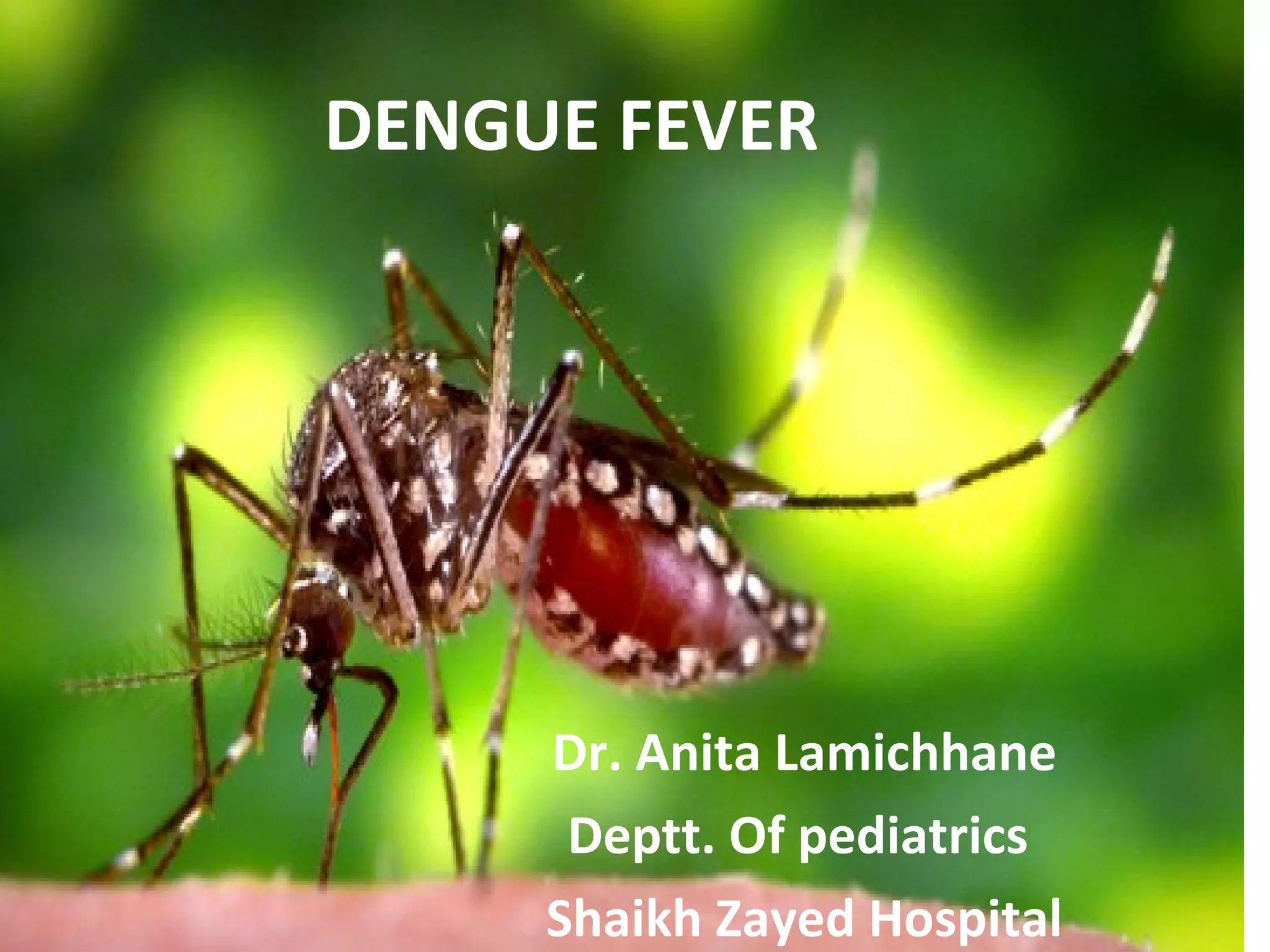
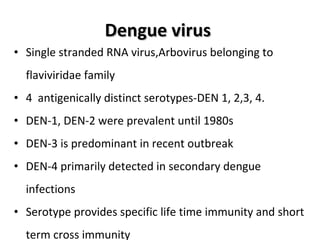
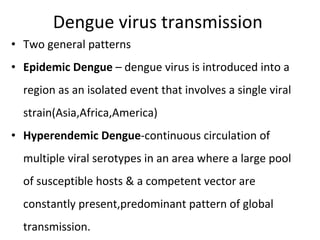
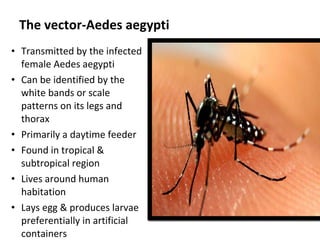
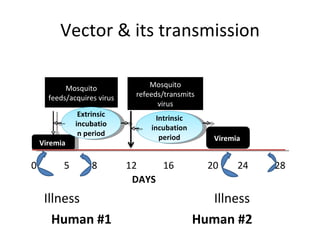
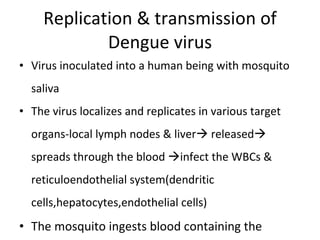
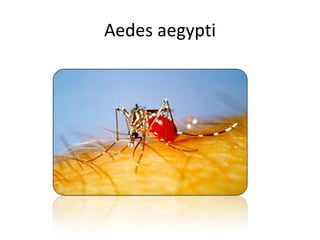
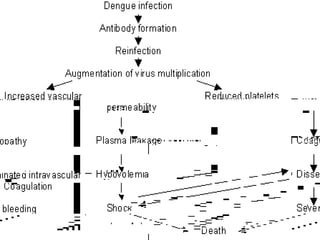
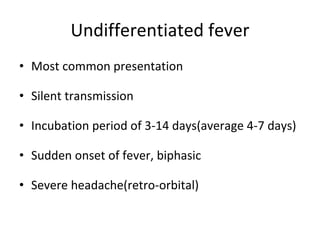
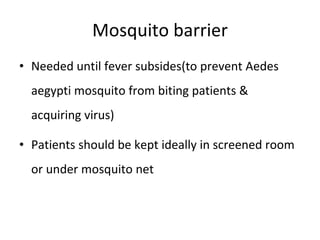
Dengue fever is caused by the dengue virus, which is transmitted by the Aedes aegypti mosquito. It has four distinct serotypes. The virus replicates in the mosquito and humans, who serve as the primary reservoir of infection. Symptoms range from a mild fever to the potentially lethal dengue hemorrhagic fever. There is no vaccine, so prevention depends on controlling the mosquito population and avoiding bites.