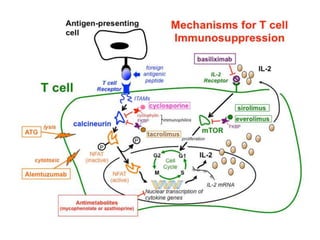
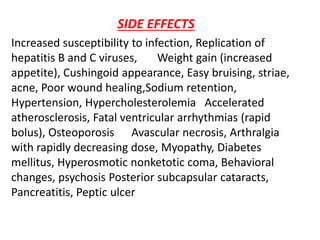
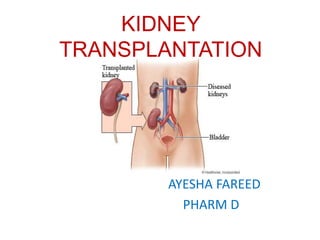
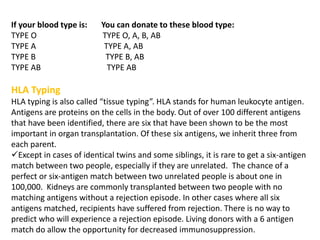
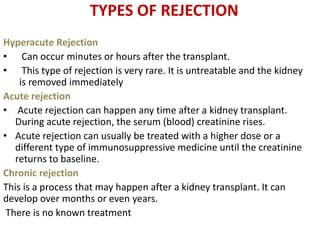
Kidney transplantation involves the surgical implantation of a healthy kidney into a patient with end-stage renal disease and can involve living or deceased donors. Successful transplantation relies on proper donor-recipient matching, which includes blood type and tissue typing, as well as management of potential rejection, which can occur in different forms post-surgery. Immunosuppressive therapies, including induction and maintenance therapies, are critical for preventing rejection and ensuring the success of the transplant.
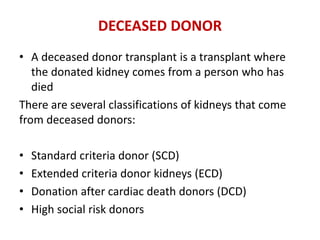

![DRUGS USED IN KIDNEY TRANSPLANT
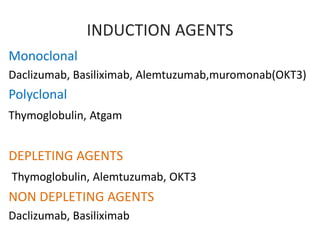
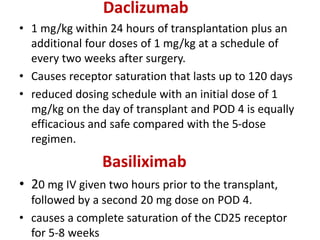
INDUCTION THERAPY
1)monoclonal antibodies:
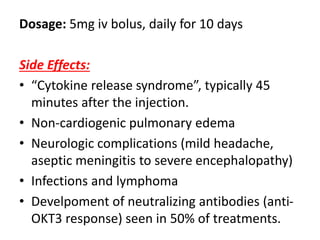
muromonab-CD3,
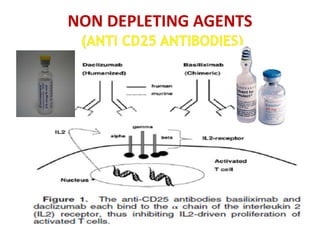
basiliximab
DaclizumaB
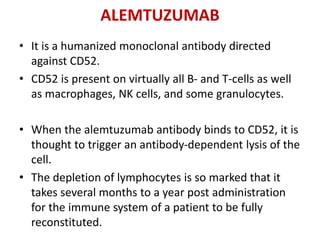
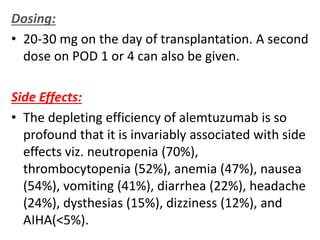
Alemtuzumab
2) polyclonal antibodies:
Antithymocyte globulin
[equine] Antithymocyte
globulin [rabbit])
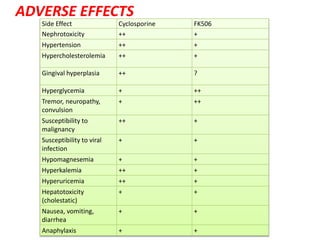
MAINTENANENCE THERAPY
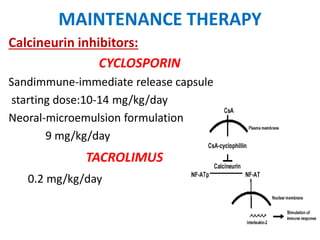
1)Calcineurin inhibitors
– Cyclosporine
– Tacrolimus
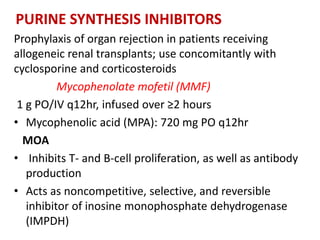
2)Purine synthesis
inhibitors/APA
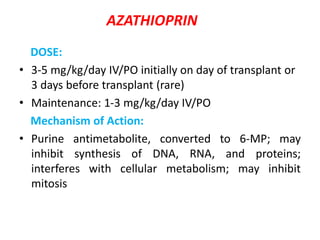
– Azathioprine
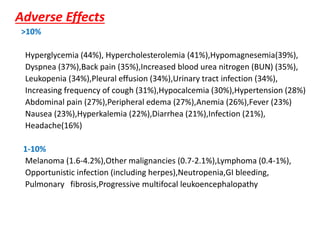
– Mycophenolate mofetil
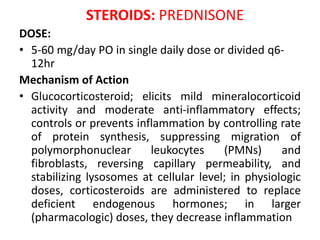
3)steroids
– prednisone
4)mTOR inhibitors
– Sirolimus](https://image.slidesharecdn.com/kt-160315162644/85/KIDNEY-TRANSPLANTATION-SEMINAR-PRESENTATION-9-320.jpg)