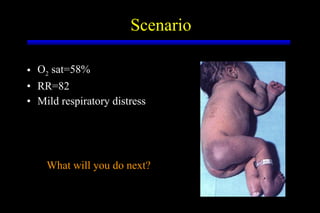
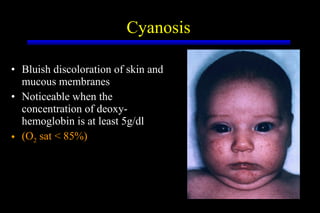
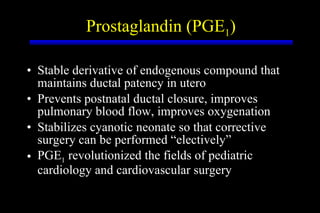
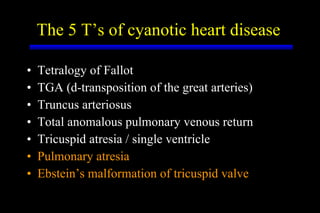
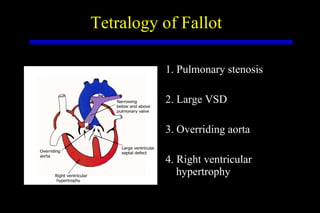
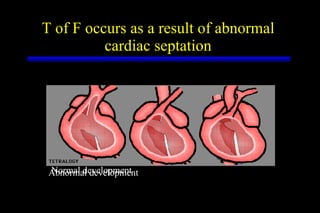
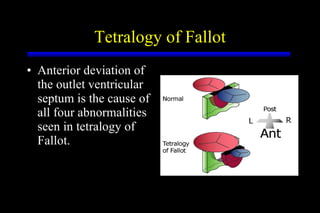
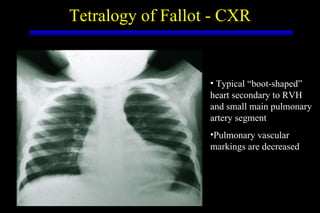
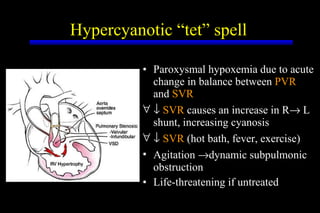
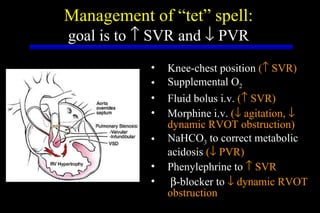
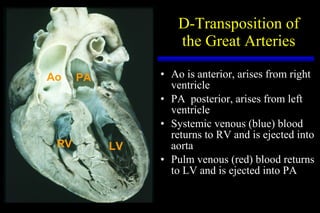
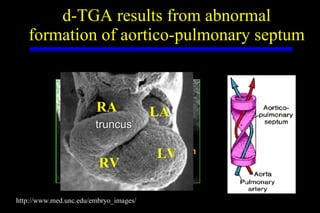
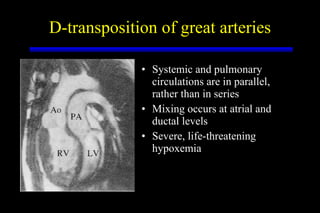
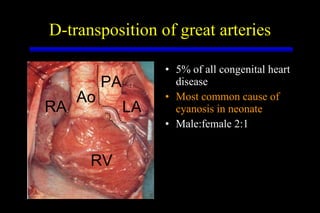
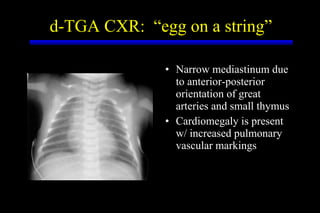
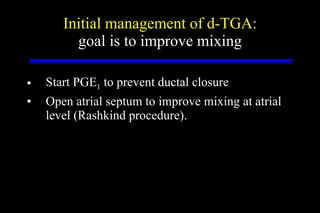
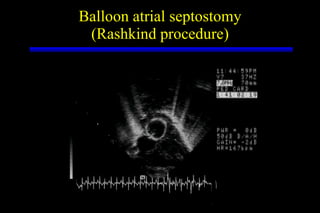
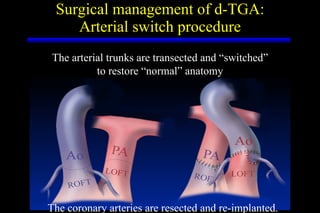
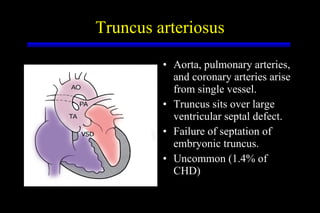
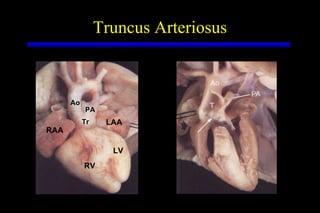
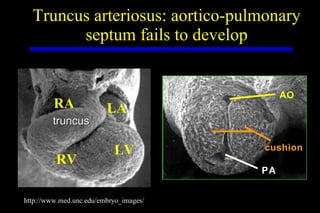
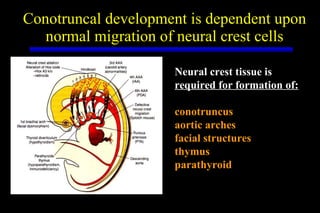
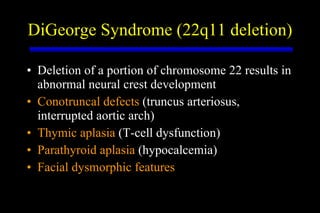
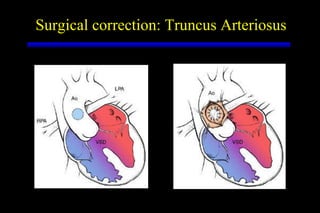
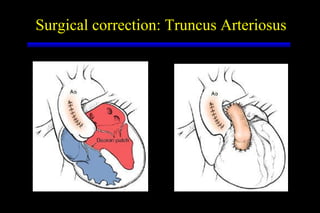
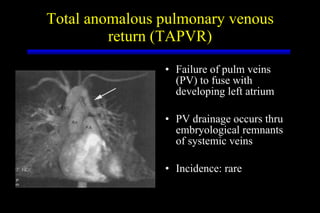
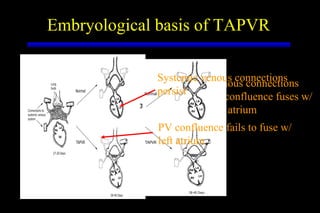
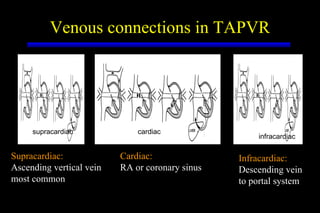
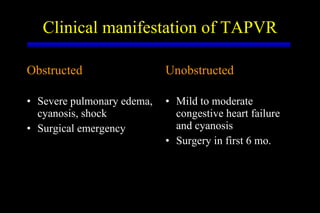
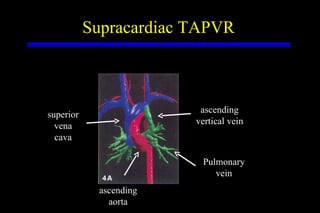
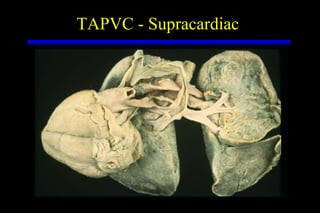
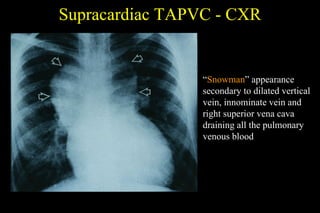
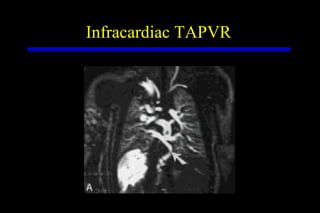
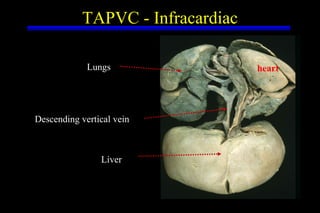
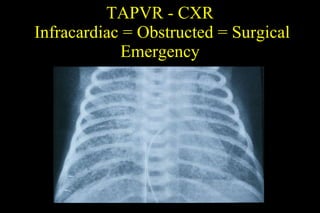
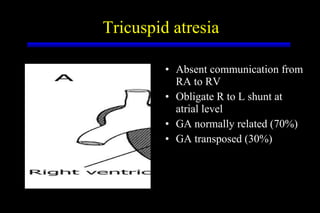
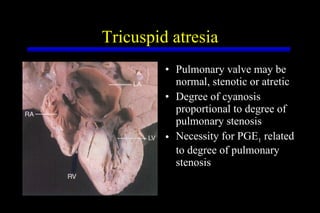
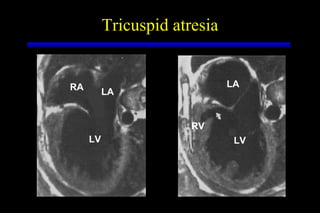
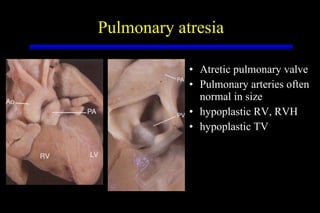
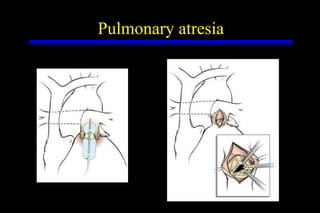
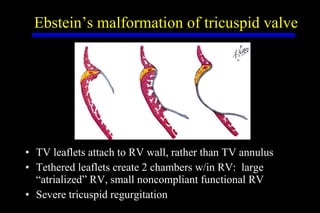
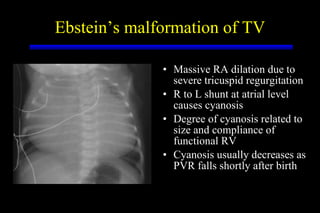
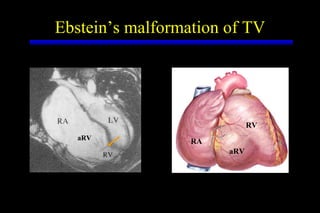
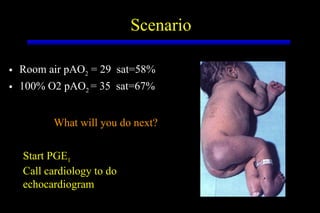
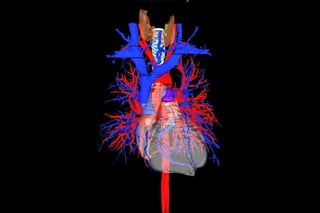
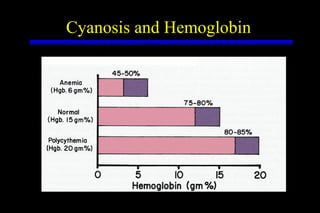
The document summarizes various congenital heart defects that can cause cyanosis in infants, including tetralogy of Fallot, transposition of the great arteries, truncus arteriosus, total anomalous pulmonary venous return, tricuspid atresia, pulmonary atresia, and Ebstein's anomaly. It describes the characteristic features, causes, evaluations, and treatments for each condition. For the scenario presented, the assistant would start prostaglandin E1 treatment and call cardiology to perform an echocardiogram to determine the specific heart defect.