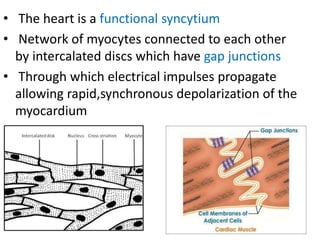
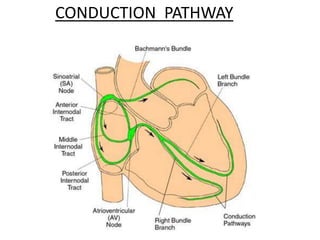
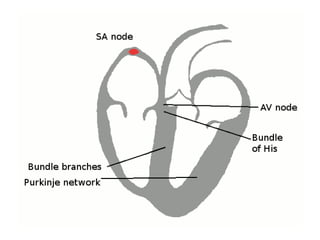
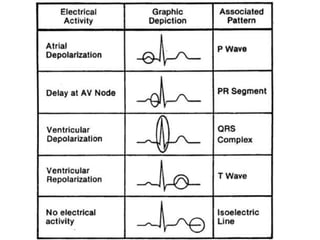
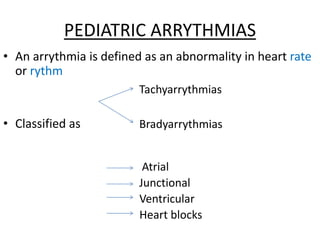
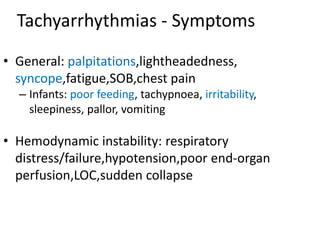
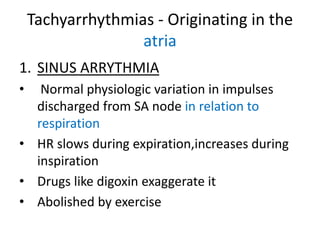
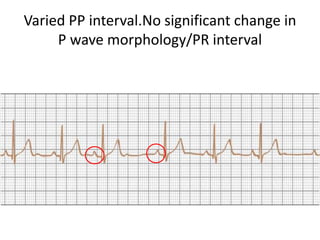
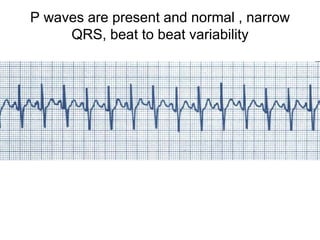
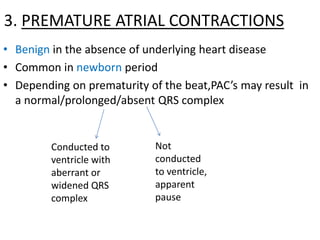
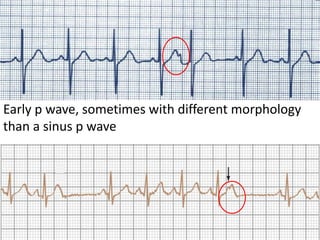
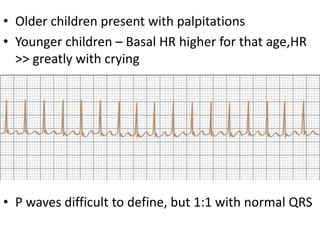
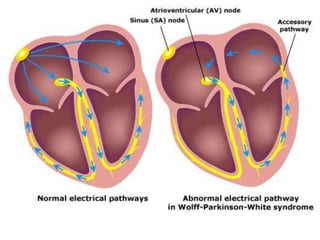
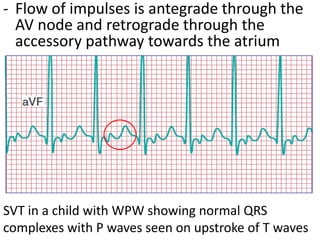
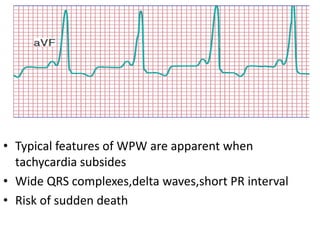
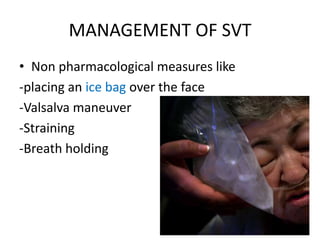
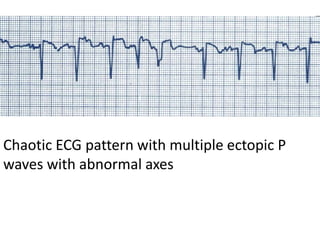
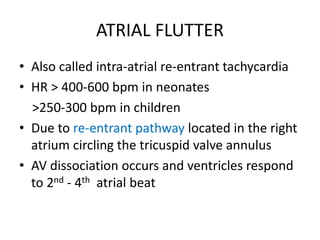
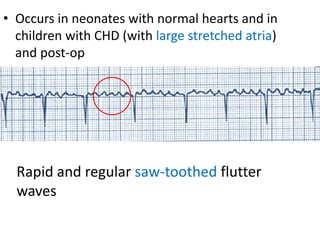
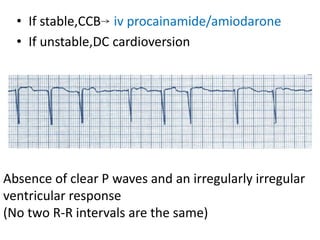
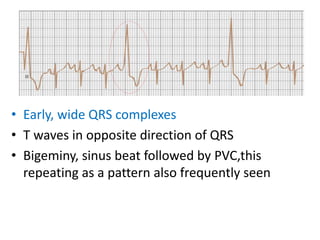
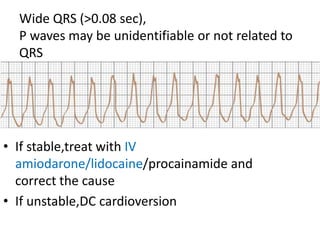
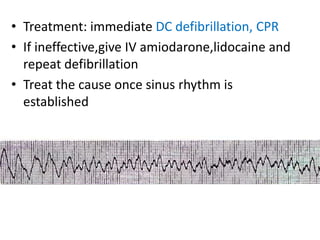
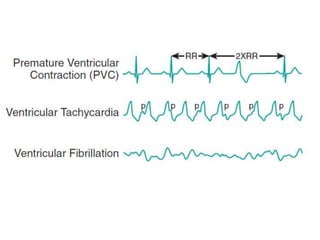
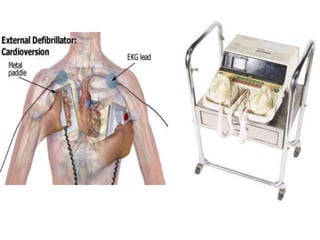
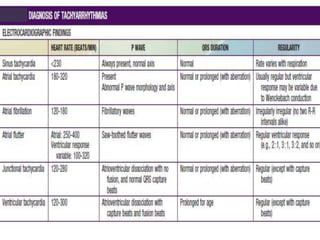
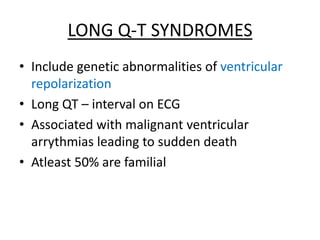
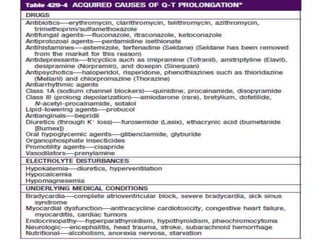
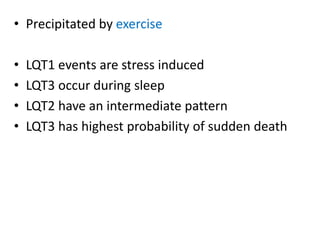
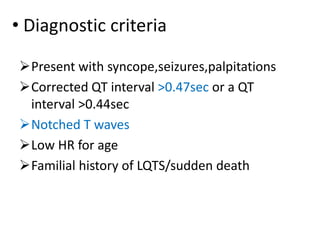
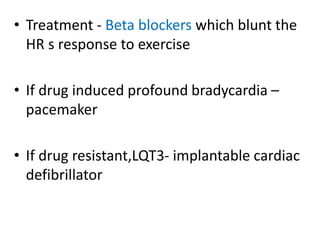
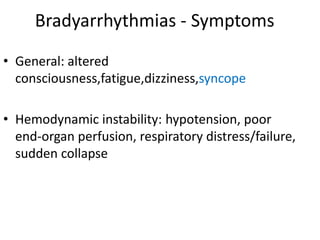
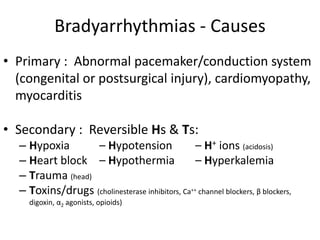
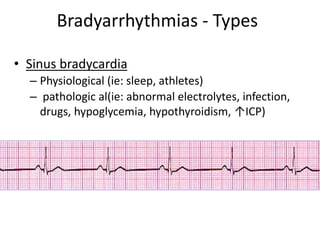
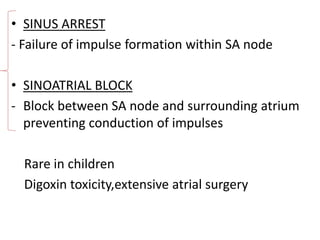
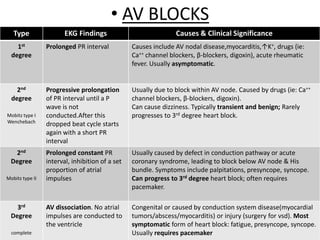
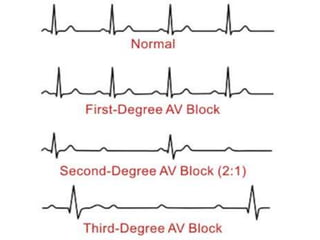
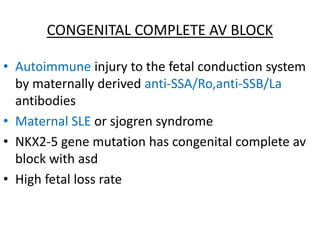
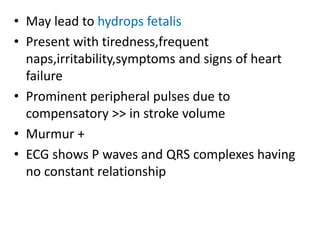
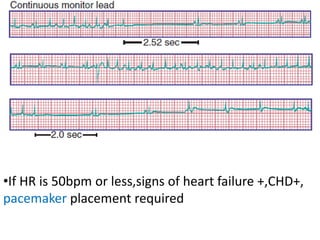
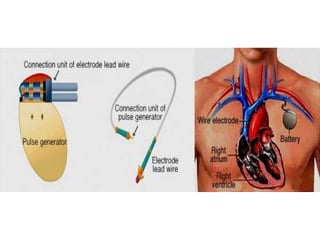
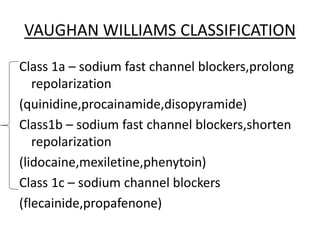
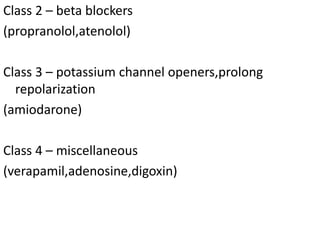
This document discusses various types of arrhythmias that can occur in children. It begins by describing the normal electrical conduction system of the heart and then discusses different types of tachyarrhythmias and bradyarrhythmias. Common pediatric tachyarrhythmias mentioned include supraventricular tachycardia, atrial flutter, atrial fibrillation, ventricular tachycardia, and ventricular fibrillation. Long QT syndrome is also summarized. Treatment options for unstable and stable rhythms are provided.