Intracranial Vascular Bypass.pptx
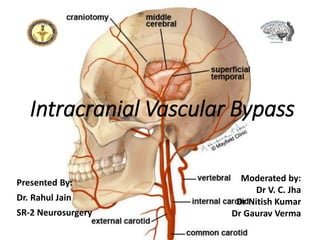
- 1. Intracranial Vascular Bypass Presented By: Dr. Rahul Jain SR-2 Neurosurgery Moderated by: Dr V. C. Jha Dr Nitish Kumar Dr Gaurav Verma
- 2. • A cerebral bypass is a surgical procedure performed to restore or revascularize blood flow to the brain. • Involves connecting a blood vessel from another psrt of brain or outside the brain to reroute blood flow around an artery that is stenosed, thrombosed or damaged. • Main goal is to provide the blood supply to target region of brain and prevent stroke. • On October 30, 1967, Professor Yasargil famously performed the first microsurgical direct flow- augmentation bypass by anastomosing the superficial temporal artery to the middle cerebral artery (STA-MCA) of a 20-year-old man suffering from Marfan’s syndrome with left M1 segment occlusion.
- 3. Who is candidate • An aneurysm, tumor, or atherosclerotic plaque that is not treatbale by endovascular or other means. • Failure of medical management to control TIA symptoms or stroke. • CTA, MRA or Angiogram suggestive of arterial stenosis or occlusion. • Cerebral blood flow studies like CT perfusion, PET, SPECT showing arterial stenosis causing insufficient blood flow to brain.
- 4. Cerebral bypass may be helpful in restoring blood flow and reducing the risk of stroke in conditions such as: • Moyamoya disease: a narrowing of the internal carotid arteries at the base of the brain that can cause multiple strokes or hemorrhages. A bypass can restore blood flow to the brain and prevent future strokes. • Aneurysm: a bulge or ballooning of an artery wall. Some giant, fusiform, or dissecting aneurysms cannot be treated with surgical clipping or endovascular coiling. In such cases, the parent artery must be sacrificed and the blood flow bypassed for the aneurysm to be effectively treated. • Skull base tumor: a tumor can grow where the major vessels enter the skull and surround or invade the artery. Removing the tumor may require sacrificing the encased artery and bypassing the blood flow.
- 5. • Carotid artery stenosis or occlusion: a narrowing or blockage of the carotid artery in the neck caused by atherosclerotic plaque deposits in the vessel wall. • Intracranial arterial stenosis: a narrowing or blockage of an artery inside the skull that supplies blood to specific areas within the brain.
- 6. WHEN IS THE COLLATERAL CIRCULATION INADEQUATE AND BYPASS NECESSARY? Anterior Circulation • Elective ICA occlusion has been associated with ischemic complications in 30%–45% of cases, and experience with Balloon Test Occlusion suggests that a majority of patients are likely to tolerate ICA occlusion in the short term. • Many studies argue for a universal approach, advocating for bypass in all patients who undergo ICA occlusion. This strategy is intended to avoid the risk of the BTO procedure, to mitigate the potential for false negative BTO results, to minimize the risk for delayed or chronic cerebral ischemia, and to avoid inducing new aneurysms on collateral vessels.
- 7. Posterior Circulation • Unclippable and uncoilable posterior circulation aneurysms may require vertebral artery occlusion. • Bilateral vertebral artery or basilar artery occlusion is associated with a much higher risk for ischemia and should be considered only if both posterior communicating arteries are of sufficient size and collateral flow. • Proximal PCA occlusion for aneurysm treatment appears to be well tolerated, with development of an ischemic deficit, such as hemianopia, reported in only a few cases.
- 8. Distal Arterial Branches • proximal occlusion of major arteries is more likely to be tolerated than occlusion of distal arterial branches. • Revascularization of these terminal branches should be considered when these distal arteries that supply likely eloquent areas must be occluded. • When technically feasible, we plan revascularization in such cases without attempting BTO, owing to the technical difficulties and safety concerns associated with temporary balloon occlusion of these smaller, more distal arteries.
- 9. Categories of bypass procedures 1. Purpose of the bypass: flow-augmentation versus flow-preservation. • Indications for flow-augmentation bypass include moyamoya vasculopathy, chronic steno-occlusive disease, and acute ischaemic stroke. • Indications for flow preservation typically include intracranial aneurysm surgery and tumour surgery. 2. Direct, Indirect, and Combined procedures • Indirect procedures rely on the overlay of vascularized tissue (i.e., muscle, dura, pericranium, and omentum) onto the cerebral cortex to promote neoangiogenesis over time and achieve a delayed revascularization
- 10. • direct bypass instantly stimulates blood flow to the brain by direct microvascular anastomosis between a donor artery (or graft interposition, i.e., connected to a donor artery) and an intracranial recipient artery. • Combined procedures consist of applying both direct and indirect techniques in the same surgical session. A. Depending on the choice of the donor artery (extracranial vs. intracranial donor), a direct bypass is further classified into extra- to intracranial (EC-IC) versus intra- to intracranial (IC-IC). B. Lastly, direct bypass procedures are categorized according to the rate of flow (capacity) the bypass can carry: low capacity (<50 mL/min), intermediate (50–100 mL/min), or high capacity (>100 mL/min)
- 12. TYPES OF REVASCULARIZATION PROCEDURES • Technical considerations for cerebral revascularization include • the donor site, • the recipient site, • the conduit, and • the quantity of flow to be replaced. • Donor sites are commonly either extracranial carotid or vertebral arteries, or involved or adjacent intracranial cerebral arteries. Common vessels used as a graft are the saphenous vein in the leg or the radial or ulnar arteries in the arm- for high flow. The other type does not use a vessel graft but a healthy donor artery.
- 13. • Donor artery is detached from its normal position on one end, redirected to the inside of the skull, and connected to an artery on the surface of the brain – for low flow. • Recipient sites are generally those arteries immediately distal to the pathology in question, though recipient sites can also be remote to the lesion, relying on retrograde redistribution of flow after bypass. • Conduit options include interposition grafts such as radial artery or saphenous vein, pedicled grafts such as STA or occipital artery (OA), or direct anastomosis with no conduit at all. • Flow demand is typically estimated by the sum of the flow measured in each of the recipient branches. Permutations of these can be classified into four types of bypass.
- 14. Type I Bypass: Intracranial-Intracranial Interposition Bypass • Connects an intracranial artery to another intracranial artery using an interposition graft. • Extent from the parent artery proximal to the site of the occlusion to the point immediately distal to the parent artery, or from a separate donor source. • Example - intracranial petrous ICA–supraclinoid ICA interposition bypass. It can be used when the ICA is resected to remove skull base tumors, or to trap giant intracavernous carotid aneurysms.
- 15. • Disadvantage - complex and requires a prolonged period of ICA occlusion. • Accordingly, it is associated with a significant complication rate related to graft occlusion and perioperative ischemic brain injury. petrous-supraclinoid internal carotid artery (ICA) skull base bypass showing a saphenous interposition graft
- 16. Type II Bypass: Extracranial- Intracranial Interposition Bypass • interposition graft between an extracranial artery and a major intracranial artery. • Indication - employed when a major arterial trunk must be occluded to treat a tumor or complex aneurysm, and the distal collateral circulation is grossly inadequate (as evidenced by the absence of communicating arteries seen angiographically or by the rapid onset of a deficit during balloon test occlusion). • bypass is planned to replace all of the circulation to a major arterial territory, and therefore a large conduit is sometimes needed.
- 17. • Blood flow through radial artery and saphenous vein grafts typically exceeds 70 mL/min and can reach well beyond 200 mL/min. • Disadvantages of interposition grafts • Vein grafts – lower long term atency, kinking, calibre mismatch between larger vein and smaller intracranial vessels. • Arterial grafts – vasospasm, pressure dilatation technique to counter vasospasm can cause endothelial damage resulting in thrombosis. • using multiple pedicled grafts is adequate for revascularization in most cases with anterior circulation aneurysms.
- 18. • Type II bypass is often required when scalp arteries are hypoplastic or cannot reach the recipient vessel. • In circumstances in which only proximal occlusion is to be performed as in the case of some dolichoectatic and fusiform aneurysms, we prefer the use of a type III bypass.
- 19. A) A clamp is passed from the cranial incision behind the root of the zygomatic arch to the cervical incision. (B) A chest tube is pulled from the cervical incision to the cranial incision. (C) The harvested saphenous vein graft is passed through the chest tube, which is removed, leaving the graft in its subcutaneous tunnel. (D) The completed bypass after end-to-end anastomosis to the internal carotid artery (ICA) and end-to- side anastomosis to the MCA. (E) Alternative technique showing end-to-side anastomosis to the external carotid artery (ECA) Extracranial Carotid Artery–Middle Cerebral Artery Interposition Graft
- 20. • For the distal anastomosis, we prefer an end-to- side anastomosis to a proximal M2 branch in the sylvian fissure. These vessels better match the size of these interposition grafts, and provide a more direct conduit to the entire MCA territory. • The alignment of the vein should be marked with a suture through the adventitia to define the proper orientation of the vein. • As suggested by Sundt and associates, the intracranial anastomosis is performed first. This sequence allows the surgeon to take advantage of slack in the graft, which can be manipulated freely while the back and front walls of the anastomosis are sutured.
- 21. Type III Bypass: Pedicled Donor Artery Extracranial-Intracranial Bypass • The STA or OA is commonly used. • Advantage – readily available, only require a single anastomosis, and have good patency rates compared with free vein or arterial grafts. • Chief drawback- lower flow rate—the STA supplies an average initial flow rate of about 15–30 mL/min. using two branches of the STA (a double-barrel bypass) to make anastomoses to two recipient branches in the target territory can increase the amount of blood supplied by the graft.
- 22. • In general, the STA can be used to revascularize the MCA territory, as well as the distal posterior circulation through the superior cerebellar artery (SCA) or PCA. • The OA is most commonly used to bypass to the PICA, but it can also be used to revascularize the anterior inferior cerebellar artery (AICA). • The preoperative angiogram should include an ECA injection to adequately define the patency, course, and caliber of the STA branches on the side on which the bypass will be performed. • STA branches are identified, largest STA branch, as identified on the preoperative angiogram, is selected as the donor vessel.
- 23. STA–MCA bypass (A) After Doppler ultrasound identification of the STA, a linear incision is made over its distal aspect. (B) The STA is exposed by cutdown technique. (C) After the temporalis muscle is incised, an oval or circular craniotomy is made over the posterior aspect of the sylvian fissure. (D) The completed anastomosis is shown
- 24. • After a linear incision is made over the parietal branch of the STA distally, the artery is identified on the superficial surface of the galea. The artery is exposed to the zygomatic arch, separated from the adjacent subcutaneous tissue with an adventitial cuff. • The craniotomy is centered 6 cm above the external auditory meatus (the Chater point), where several large MCA branches emerge from the distal sylvian fissure. • When there are two separate MCA branches that arise from the dome of an aneurysm, a single STA bypass may not be sufficient. In these cases, a doublebarrel STA bypass, using both the frontal and parietal branches, can be performed to bypass to two separate MCA branches.
- 25. • After the dura is opened and an appropriate recipient artery (≥1 mm diameter) is selected, the arachnoid over this vessel is opened, and a 10-mm length of the vessel is prepared. • The distal end of the STA is denuded, beveled, and spatulated for the bypass. The STA is occluded and the vessel is incised, matching the donor artery orifice for size (approximately 3–4 mm). • The anastomosis is completed with about four interrupted 10-0 monofilament nylon sutures on each of the front and back walls. • The distal MCA temporary clip is usually opened first, allowing backfilling of the anastomosis to inspect for major leaks, before opening the proximal MCA and STA clips.
- 26. Type IV Bypass: Direct Intracranial- Intracranial Arterial Anastomosis • Anastomosis between two adjacent cerebral artery segments. • Advantages over EC-IC bypass:- • obviate the need for harvesting extracranial grafts. • Useful for distant recipient locations, such as the interhemispheric fissure • Disadvantages – • Long-term patency rates for these bypasses are uncertain • more technically demanding • can only be applied where an appropriate donor artery is in close proximity to the recipient artery.
- 27. • can involve end-to-end primary reanastomosis after excision of an aneurysm, side-to-side anastomosis of two adjacent intracranial arteries, or an end-to- side anastomosis between two cerebral arteries. • Examples of side-to-side type IV bypasses include PICA-PICA, pericallosal-pericallosal, and MCA-MCA between adjacent MCA branches in the sylvian fissure.
- 28. Pericallosal artery–Pericallosal artery intracranial revascularization The arteries are exposed adjacent to the corpus callosum, and a side-to-side anastomosis is made completed pericallosal artery–pericallosal artery bypass for the treatment of a giant, wide-necked, partially thrombosed anterior communicating artery aneurysm (arrow)
- 29. Techniques for Occluding or Trapping an Aneurysm, After Bypass • Combined proximal and distal parent artery occlusion immediately after the bypass is completed. • Trapping is preferable because it isolates the aneurysm from the circulation, avoids the risk for rupture from retrograde filling. • Proximal parent artery occlusion alone, which alters the blood flow to the aneurysm, tends to be adequate to induce aneurysmal thrombosis, while allowing for collateral circulation and revascularization to maintain the patency of critical branches along the artery.
- 30. • Direct surgical occlusion of the proximal parent artery in the neck, or just proximal to the aneurysm (hunterian ligation) is typically performed immediately after construction of the bypass. • In some cases, the parent artery proximal to a giant aneurysm cannot be exposed easily during the same procedure used for the bypass. In such cases, coil occlusion of the parent artery immediately following bypass can be performed.
- 31. OUTCOMES 1. most serious acute complication is that of early graft occlusion. • patency of arterial and venous grafts can be ensured by • gentle and meticulous surgical technique; • Careful avoidance of twisting, kinking, stretching, or tension of the graft; • avoidance of graft spasm by adventitial papaverine irrigation; and • administration of perioperative antiplatelet therapy. A. Complications
- 32. • If there is any question intraoperatively about the patency of the bypass, as determined visually using ICG video angiography and Doppler ultrasound, intraoperative angiography should be performed. • If the graft is found to be severely stenotic or occluded, the bypass vessel or anastomosis should be revised. Sometimes, simply repositioning the bypass vessel is adequate. 2. Aneurysmal rupture associated with the hemodynamic changes that accompany arterial reconstruction with a bypass. These complications emphasize the need to isolate the aneurysm completely from the circulation by trapping whenever possible.
- 33. 3. Ischemic neurological deficits may be evident postoperatively. Cerebral protection with moderate hypothermia, induced arterial hypertension, and barbiturate administration ordinarily minimizes this risk. • subdural or epidural hematomas postoperatively.
- 34. b. Long-Term Graft Patency • depends on several factors, with the choice of conduit used chief among them • Superficial temporal artery grafts tend to have the greatest patency rates. • The Carotid Occlusion Surgery Study showed a 96% patency rate at a mean of 605 days’ follow-up. • The International Cooperative EC/IC Bypass Study of 1985 found that the postoperative patency rate of 663 STA-MCA bypasses was 96% at an average follow-up of 55.8 months.
- 35. • Long-term bypass graft failure appears to be rare for aneurysms, estimated at 5.3%. • Young patients in particular may benefit from the addition of revascularization, as ICA occlusion appears to confer an increased lifetime risk of stroke and secondary intracranial aneurysm formation. • Occlusion of vein grafts increases over time. Ten years after surgery, thrombosis occurs in about 40% of aortocoronary grafts and in more than 50% of femoropopliteal bypasses. • In a study by Regli and coworkers, Long saphenous vein grafts for cerebral revascularization, the early patency rate was 88%, and at 13 years it was 73%.
- 36. C. Results of Bypass for Complex Intracranial Aneurysms • Using saphenous vein graft bypasses for giant aneurysms, Sundt and associates reported an acute graft patency rate of 94%. “Excellent” or “good” outcomes were achieved in 80% of anterior circulation aneurysms and in 44% of posterior circulation aneurysms. • Lawton and colleagues reported that 93% of 61 patients had good outcomes after revascularization for intracranial aneurysms. • Sen and Sekhar reported results in 30 patients who underwent vein grafting with carotid occlusion or resection (primarily for tumors). Their rate of graft patency was 86% at 18 months; 4 patients sustained ischemic injury related to the bypass procedure.
- 37. CONCLUSION • Several types of EC-IC and IC-IC bypass procedures can provide revascularization, if the treatment of unclippable aneurysms or skull base tumors requires major artery occlusion or sacrifice. • The selection of the type of revascularization procedure depends on the demand for blood flow through the bypass and the anatomy of the vessels. • Parent artery occlusion or trapping by surgical or endovascular techniques, combined with EC-IC bypass to maintain tissue perfusion, is an effective strategy for treating such complex aneurysms.
- 38. Careful attention to technique can yield a high rate of bypass patency and good clinical outcomes in those patients not ideal for flow diversion or clip reconstruction.
- 39. References 1. Youmann’s and Winn Neurological Surgery 8th Ed 2. Zhao Y, et al. Direct Bypass Surgery vs. Combined Bypass Surgery for Hemorrhagic Moyamoya Disease: A Comparison of Angiographic Outcomes. 2018. Front. Neurol. 9:1121. 3. Basil E. et al. Trends in Literature on Cerebral Bypass Surgery: A Systematic Review. Cerebrovasc Dis 1 February 2022; 51 (1): 102–113. 4. https://mayfieldclinic.com/pe-erebralbypass.htm
- 40. Thank you