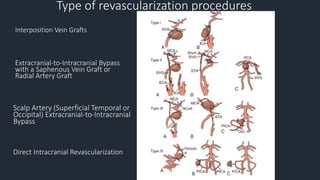
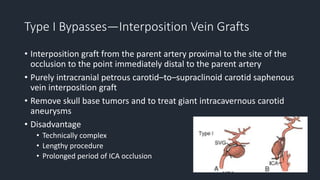
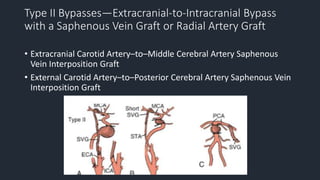
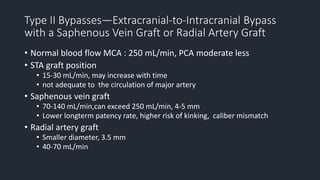
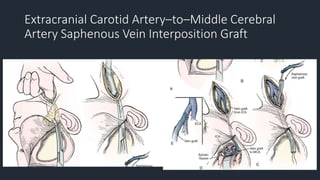
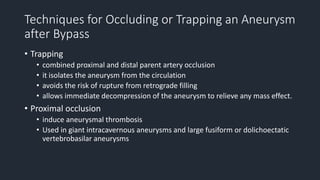
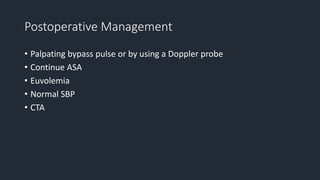
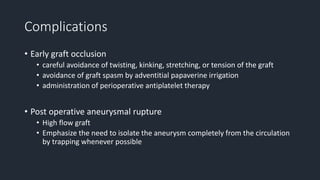
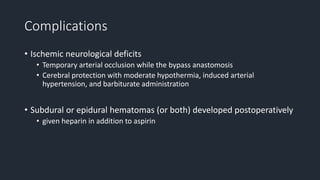
This document discusses revascularization techniques for complex aneurysms and skull base tumors. It covers when bypass is necessary due to inadequate collateral circulation, planning for bypass procedures, types of procedures including interposition grafts and direct arteriotomy, management during and after surgery, and complications. Revascularization techniques are used to treat complex aneurysms when coiling or clipping is not possible or to sacrifice arteries during tumor removal when normal blood flow must be restored. Careful planning and patient management are required due to risks of graft occlusion, hemorrhage, and ischemia.