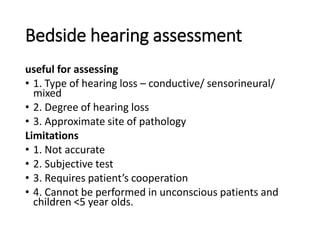
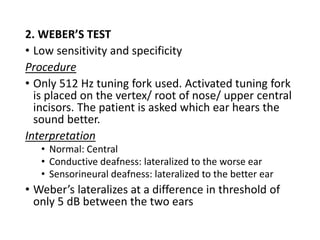
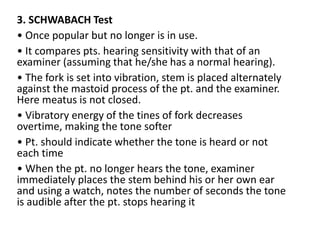
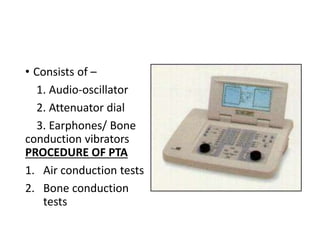
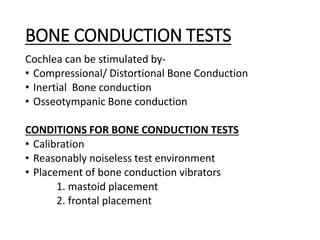
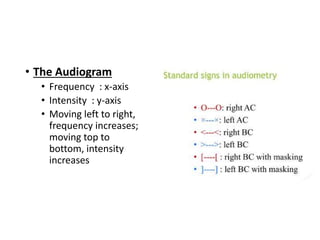
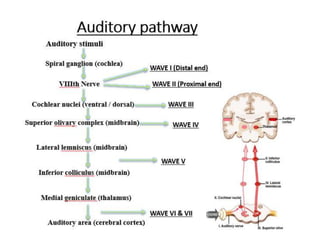
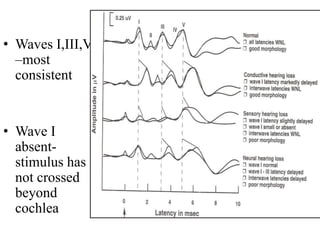
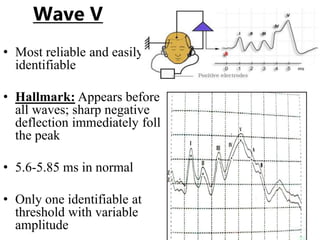
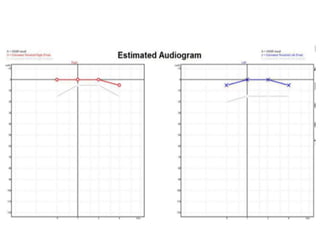
The document presents an overview of audiological assessment techniques, focusing on methods to evaluate hearing loss, including bedside hearing assessments and various tuning fork tests. It details auditory assessments such as pure tone audiometry and impedance audiometry to differentiate types of hearing loss, along with brainstem evoked response audiometry and otoacoustic emissions, which provide insights into the integrity of the auditory pathway. The document outlines the procedures, applications, and limitations of these tests, emphasizing their role in developing individualized treatment plans for patients.