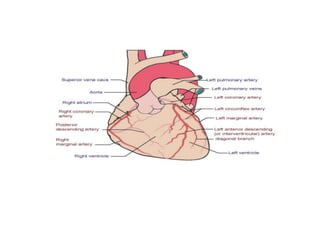
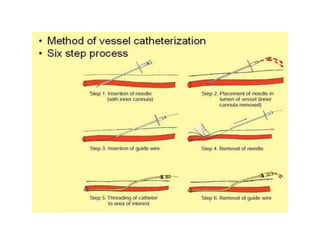
The document discusses coronary angiography, which is used to visualize the coronary arteries and detect blockages. It remains the gold standard for diagnosing coronary artery disease. The procedure involves inserting a catheter into an artery and using contrast dye and x-rays to view the arteries. It can be used for diagnostic purposes or to guide interventional procedures like angioplasty and stenting to open blocked arteries. The goals, indications, contraindications, and basic procedure steps are outlined.