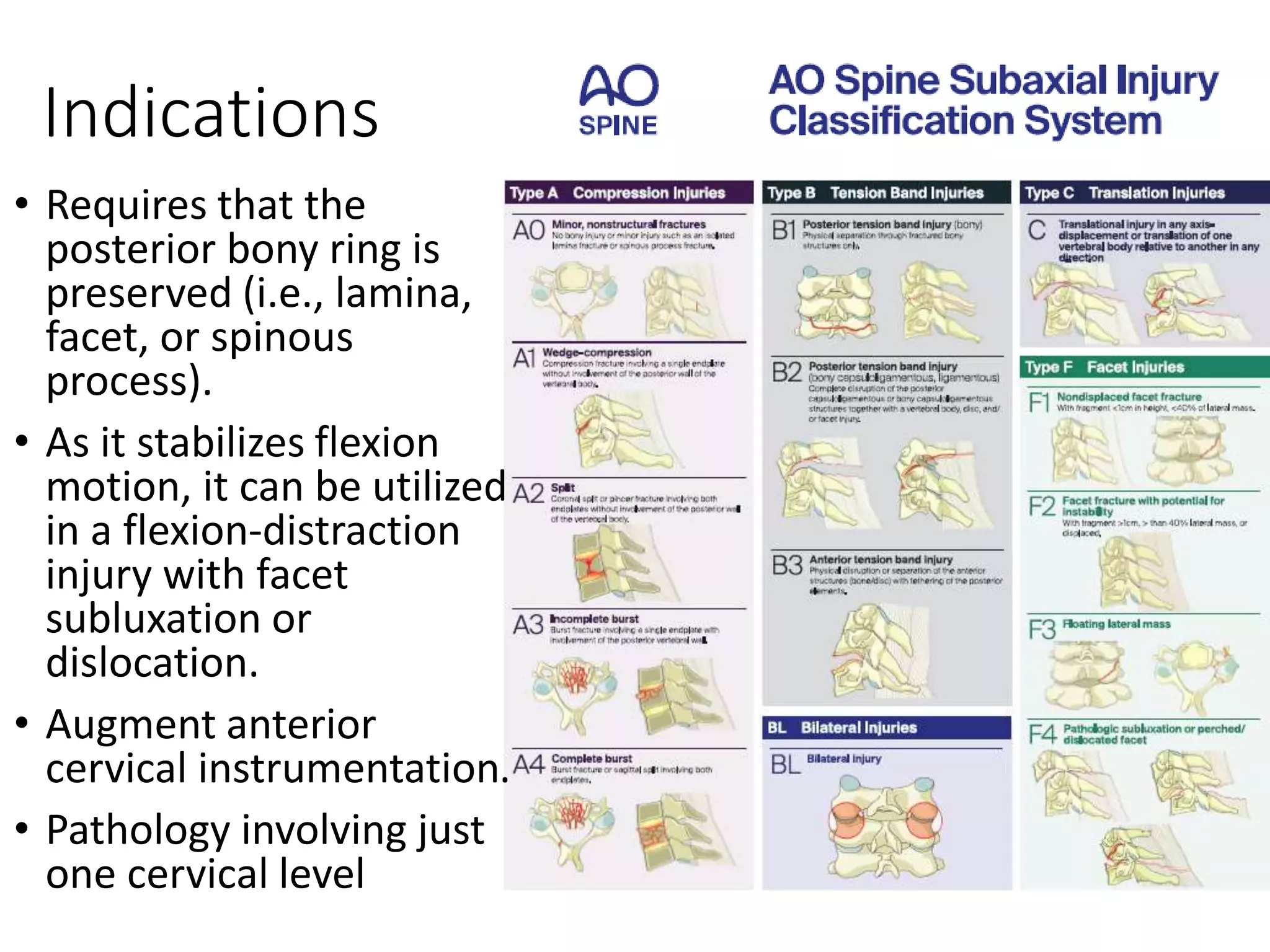
The document presents an overview of fusion techniques in the subaxial cervical spine, detailing anatomy, surgical planning, indications, and both anterior and posterior approaches to surgery. Key concepts include the principles of decompression, alignment restoration, and the considerations for fusion materials and techniques. Innovations in surgical methods, including anterior controllable antedisplacement fusion and skip corpectomy, highlight advancements that improve outcomes for complex cervical spine conditions.