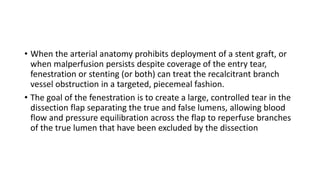
This document provides an overview of interventional radiology procedures in general surgery. It discusses:
1. The history of interventional radiology, including pioneers like Seldinger who developed catheterization techniques.
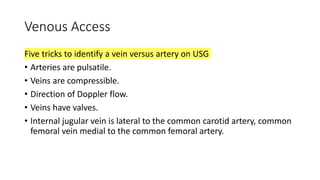
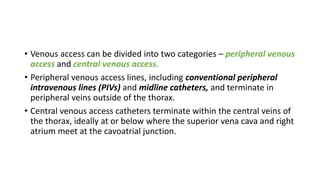
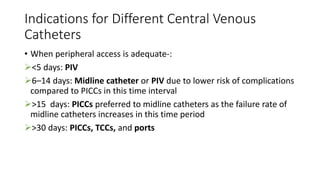
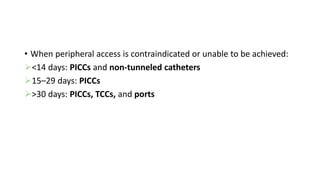
2. Methods for arterial and venous vascular access, such as the Seldinger technique for arteries and identifying veins via Doppler.
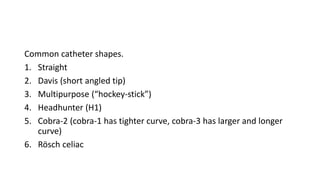
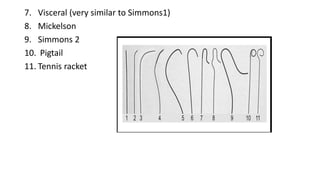
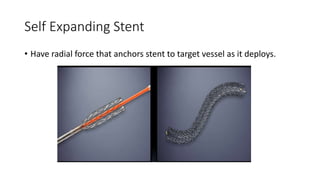
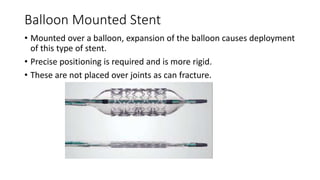
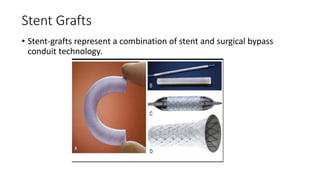
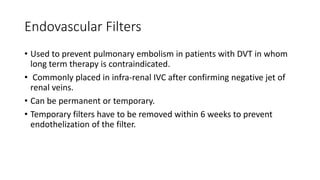
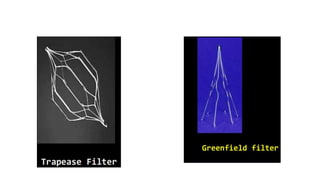
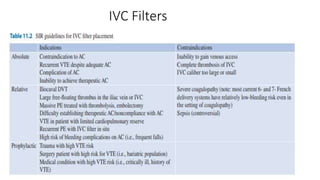
3. Common tools used like guidewires, catheters, stents, and filters.
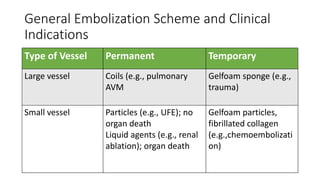
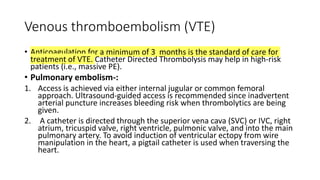
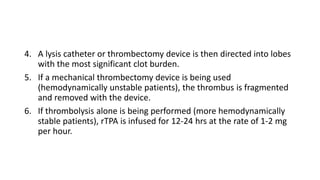
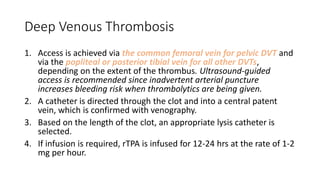
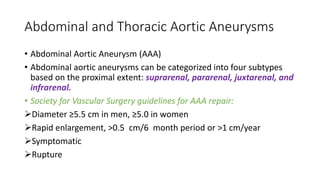
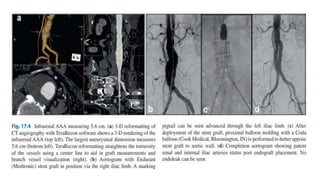
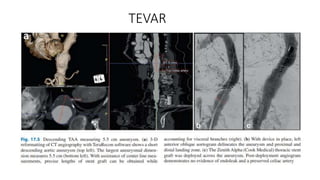
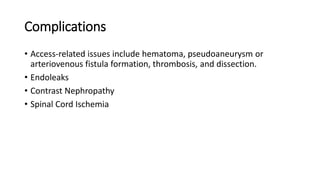
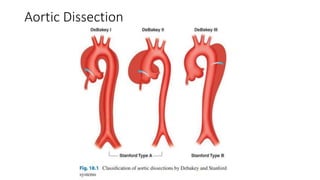
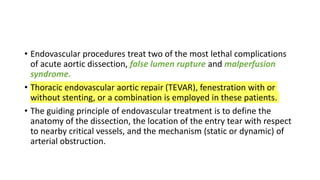
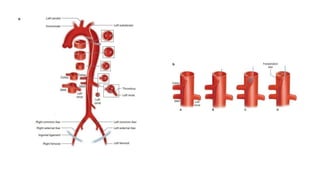
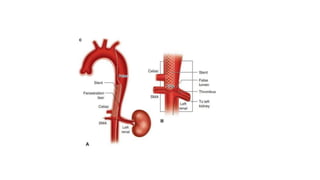
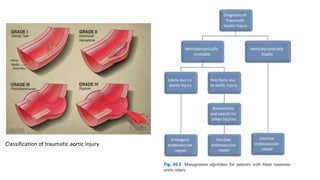
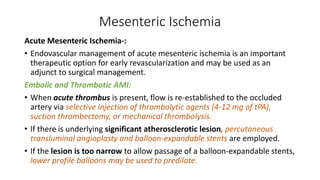
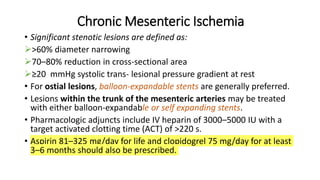
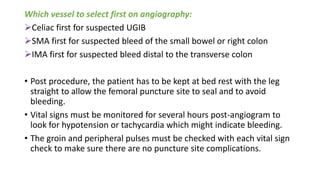
4. Clinical applications for procedures like thrombolysis, embolization, and stent placement to treat conditions like DVTs, aneurysms, and arterial blockages.