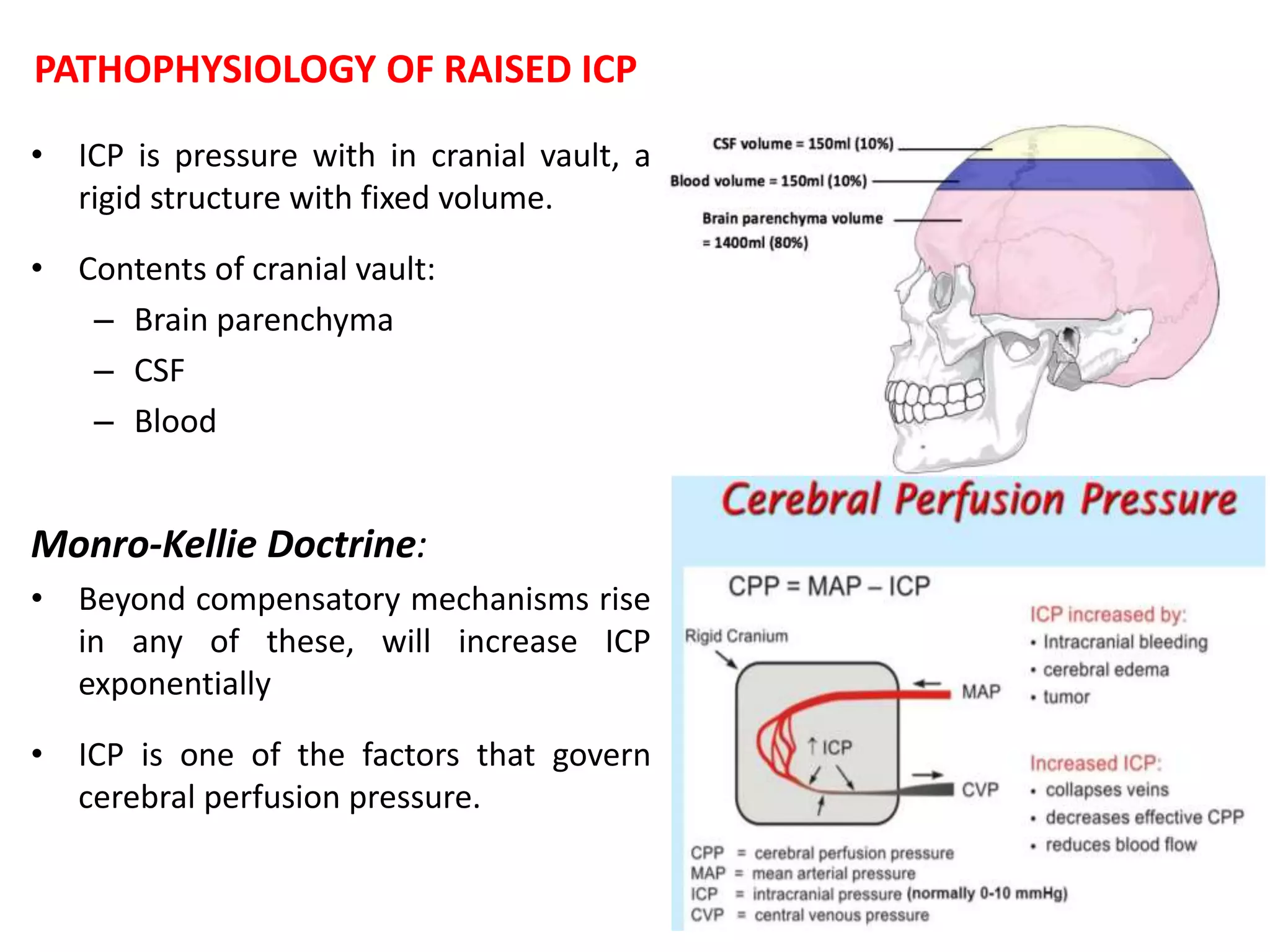
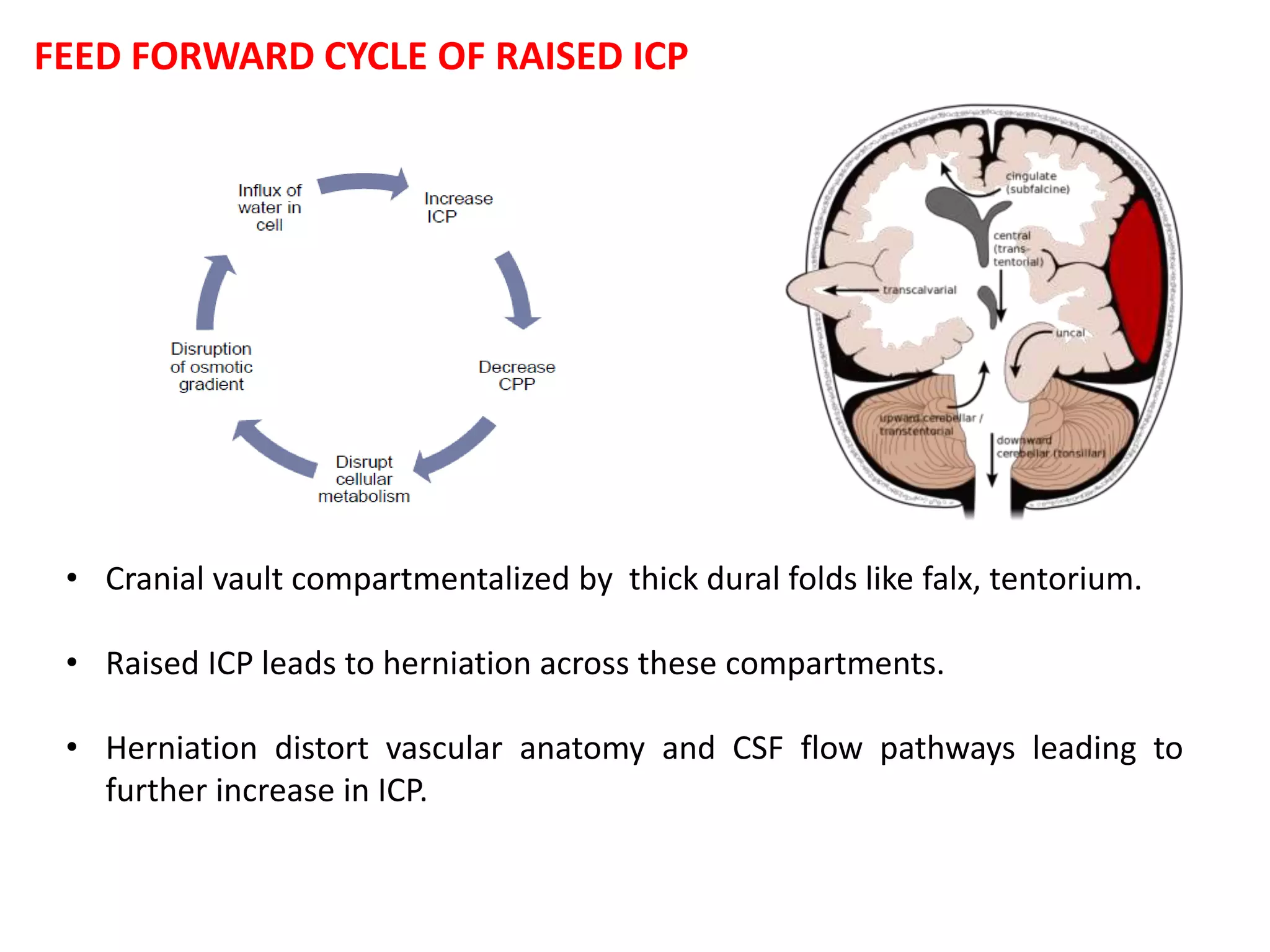
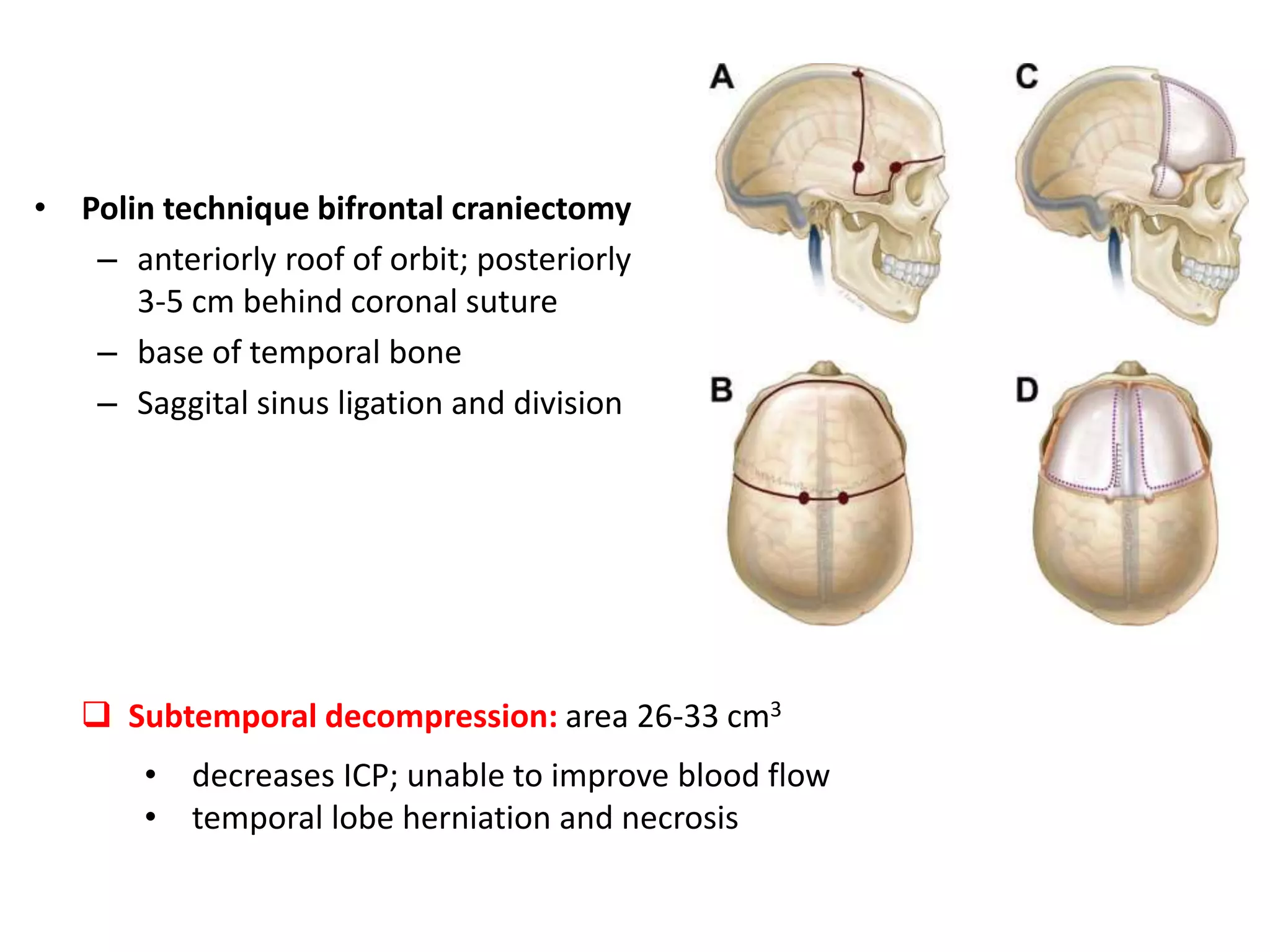
Decompressive craniectomy (DC) is a surgical procedure aimed at managing refractory intracranial hypertension and reducing mortality from traumatic brain injury. The technique, first described in the late 19th century, has evolved to include specific indications based on imaging and clinical criteria, particularly in patients with diffuse cerebral swelling. Recent studies have highlighted the benefits of early DC in reducing intracranial pressure but noted its controversial role in adult populations regarding long-term outcomes.