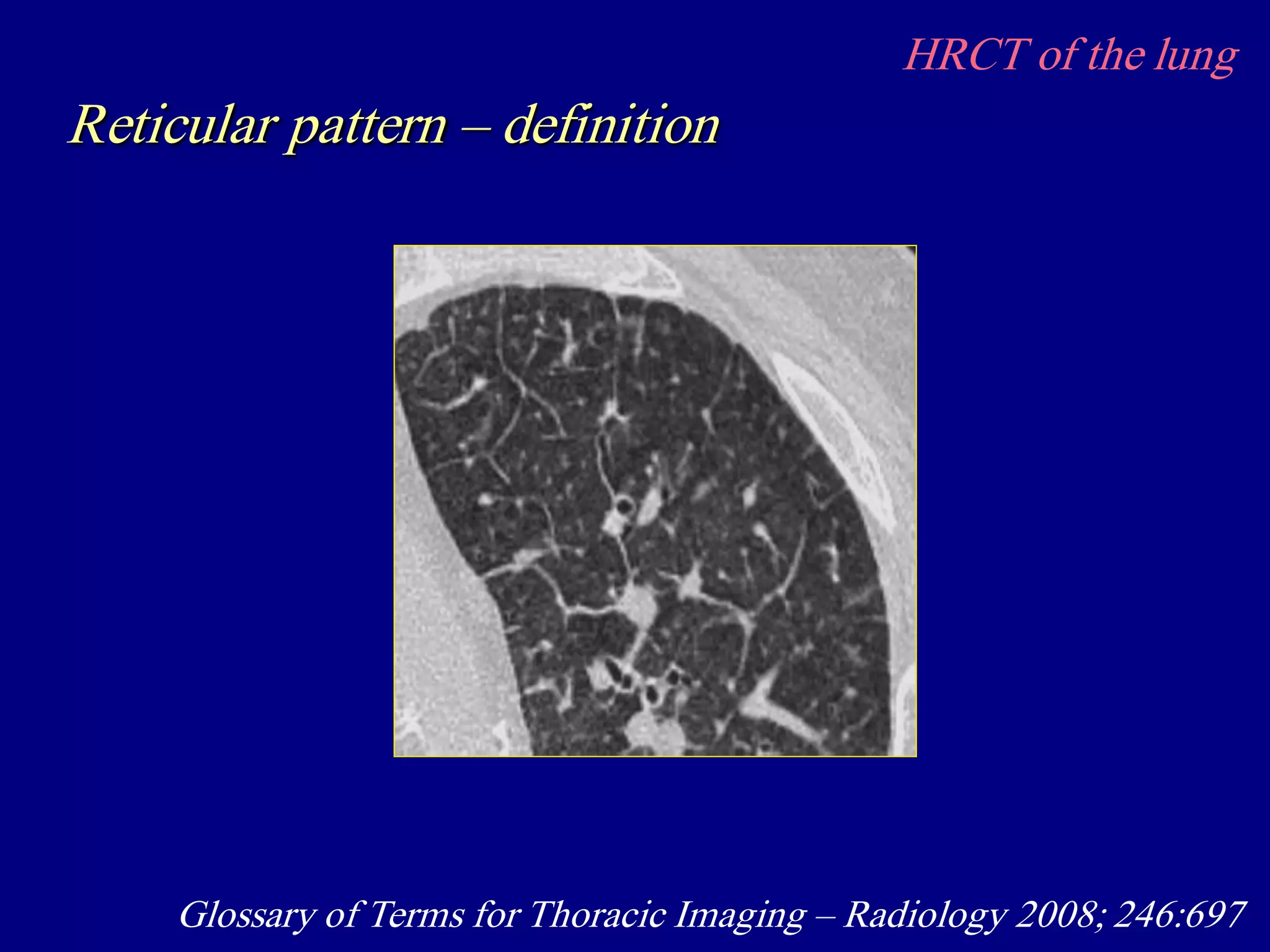
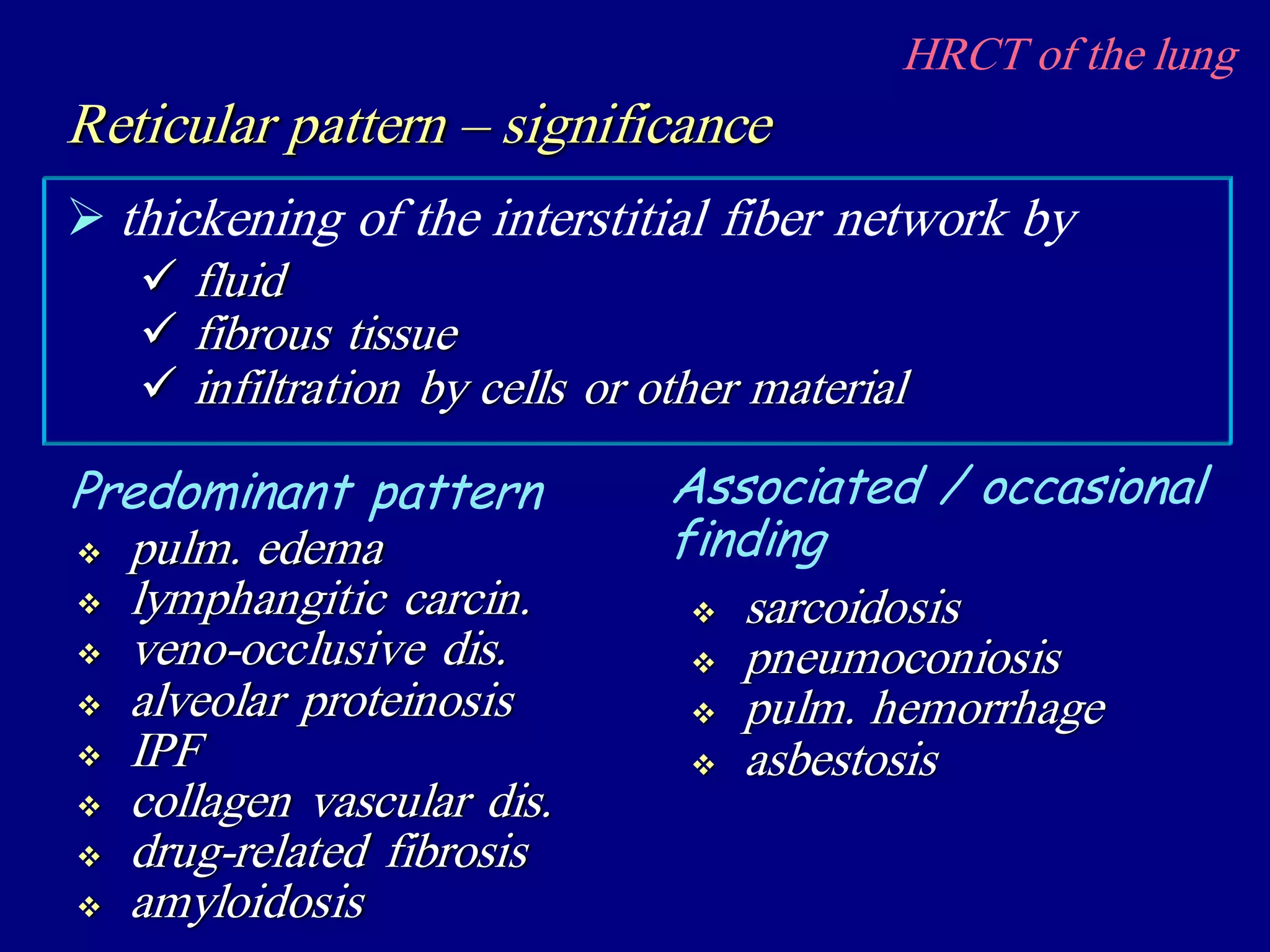
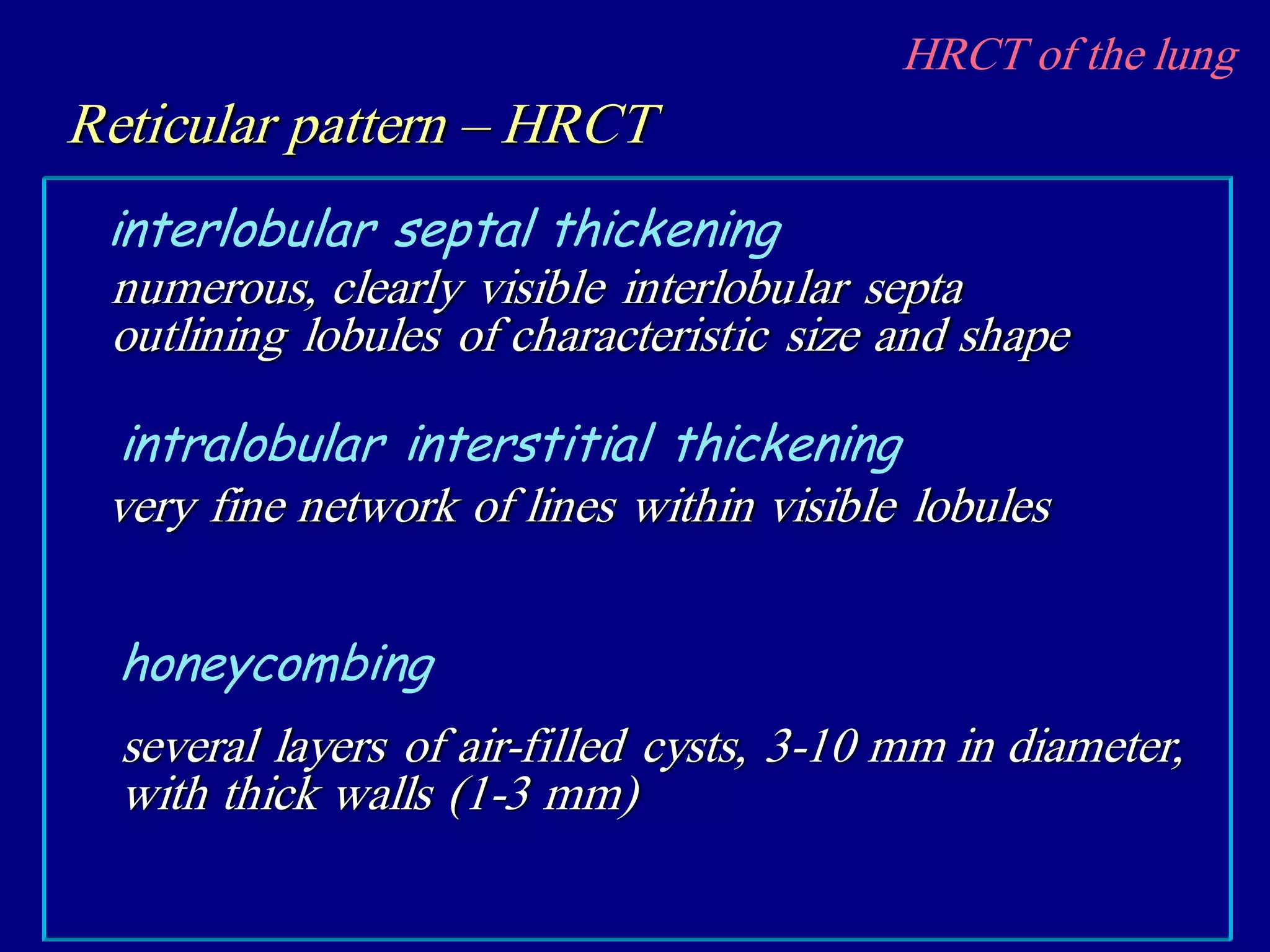
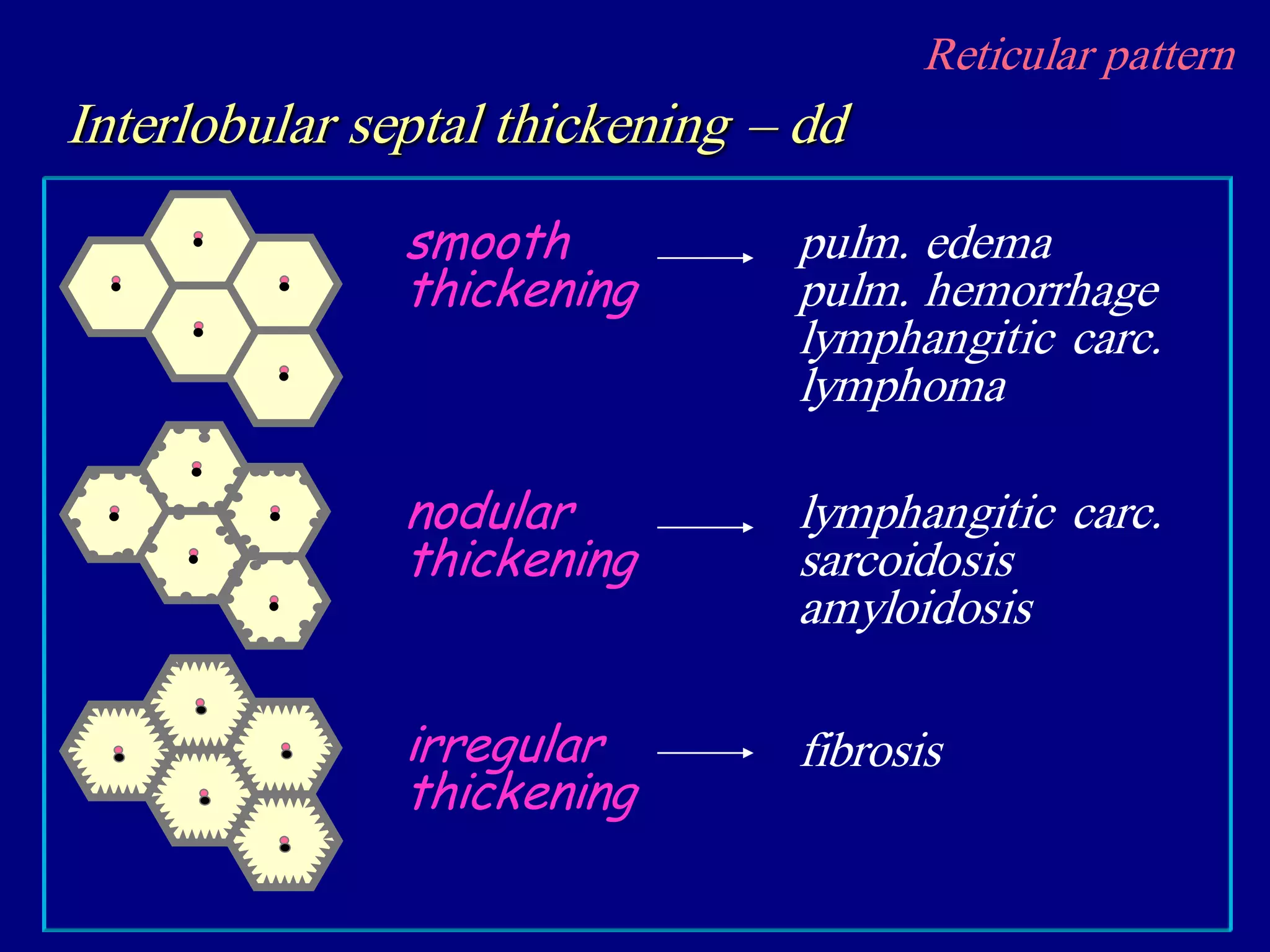
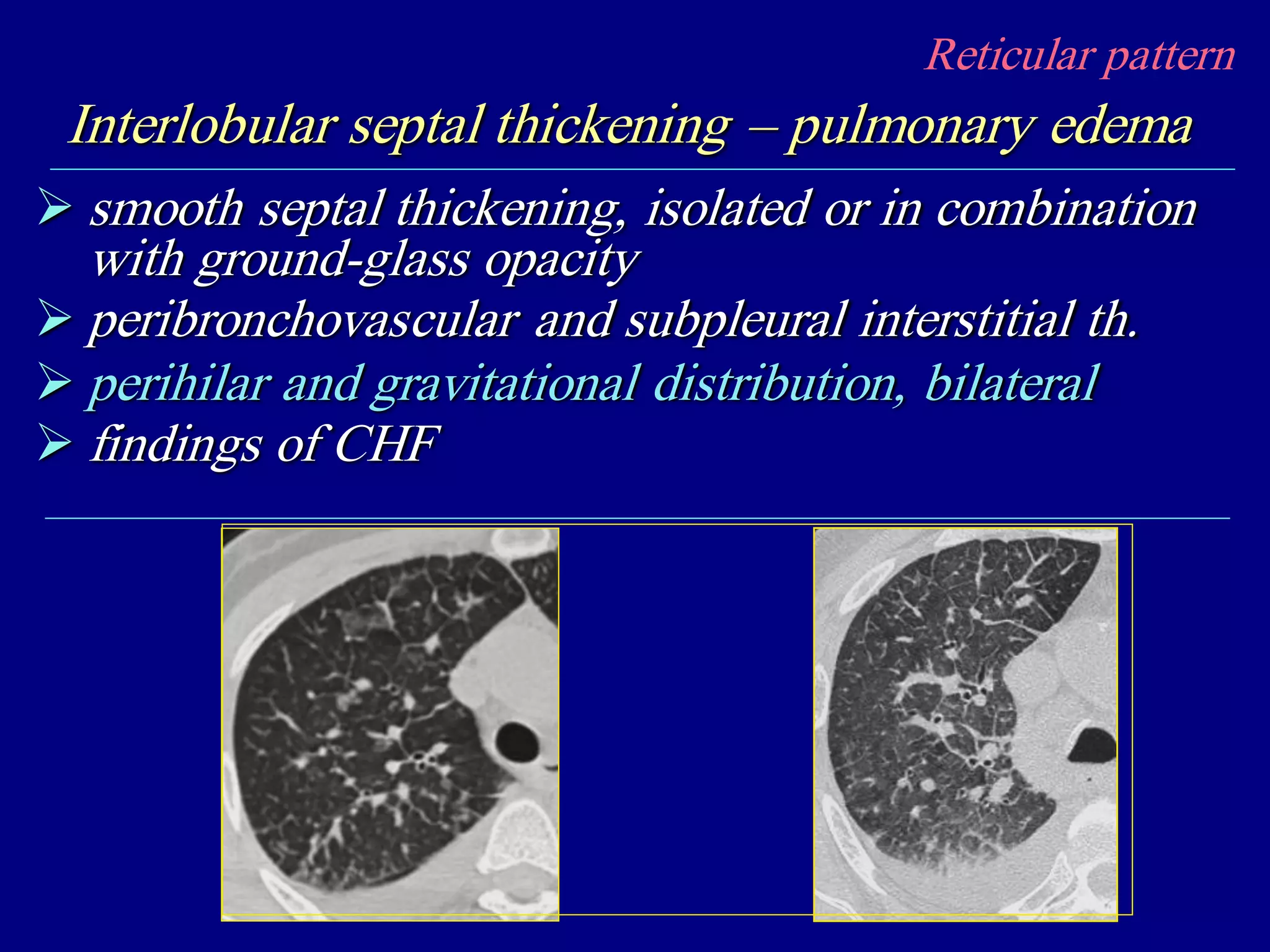
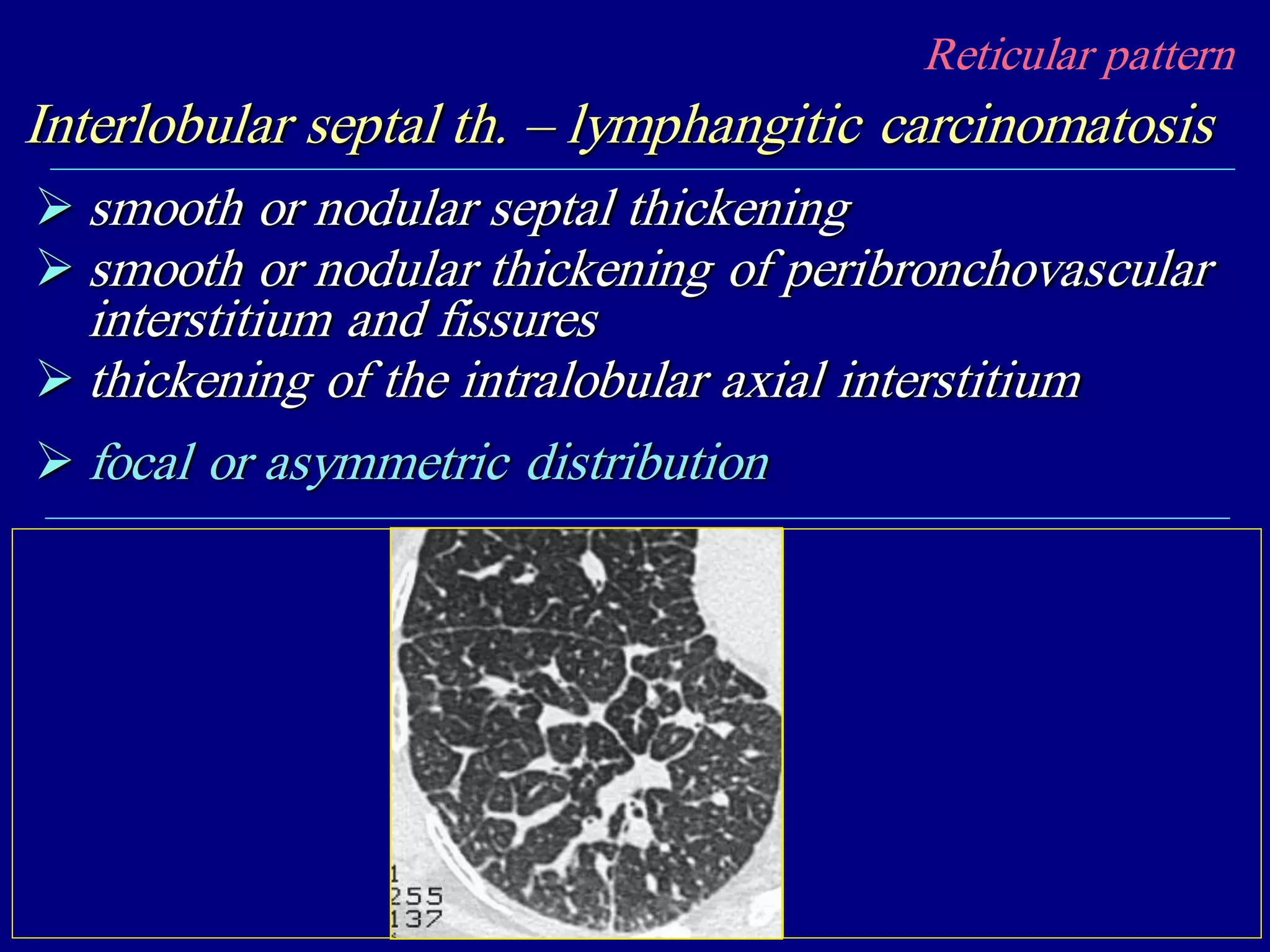
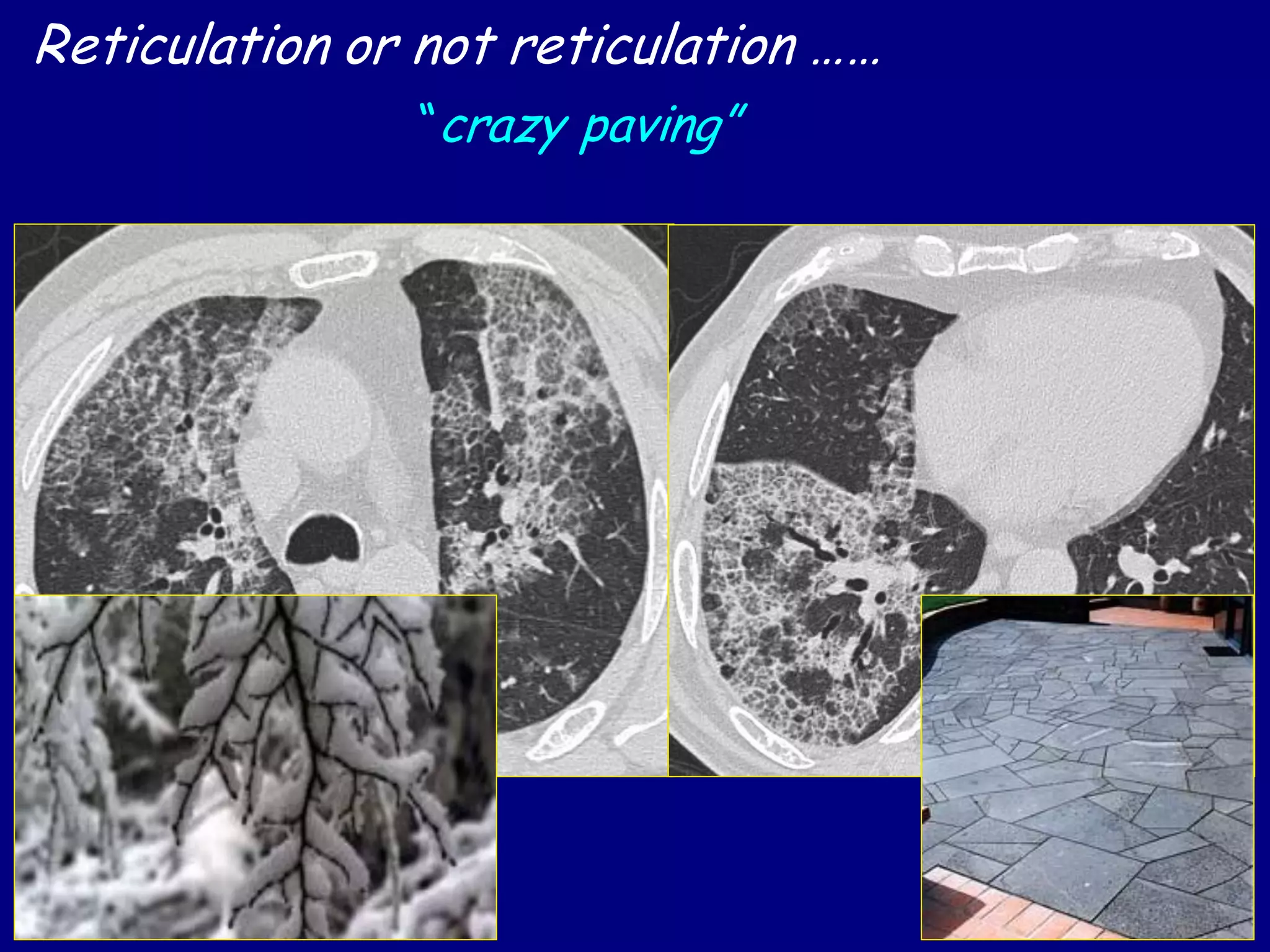
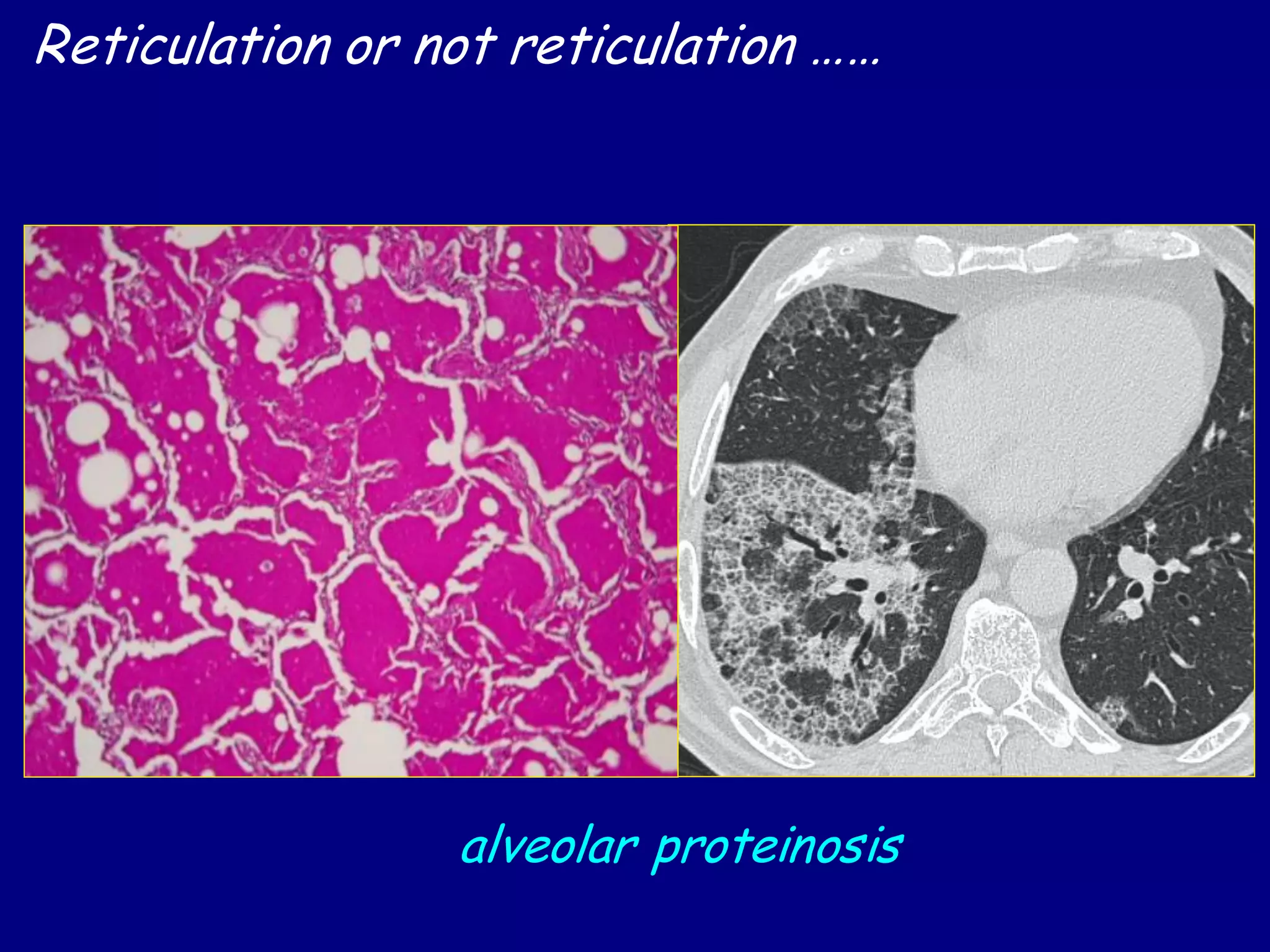
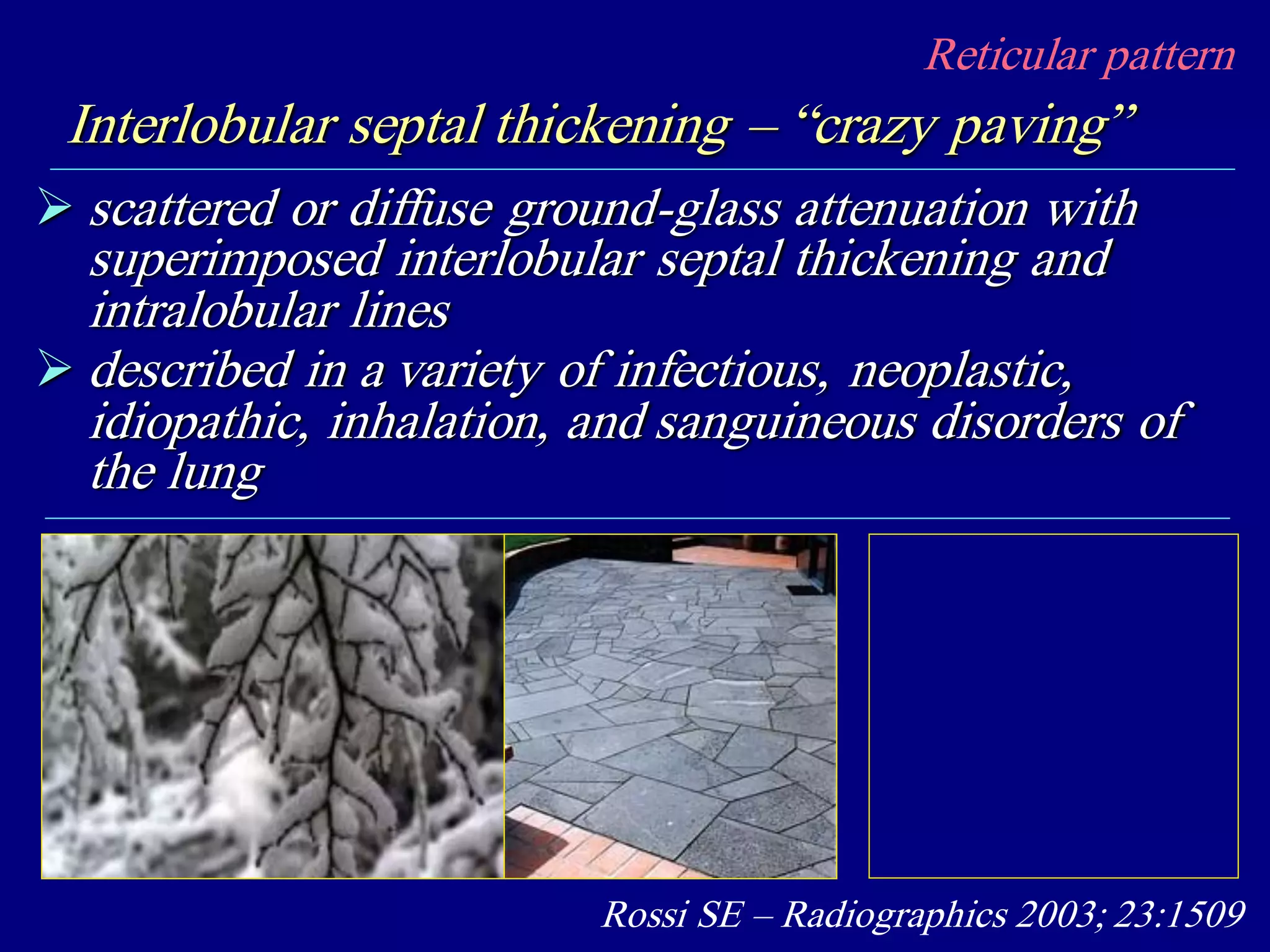
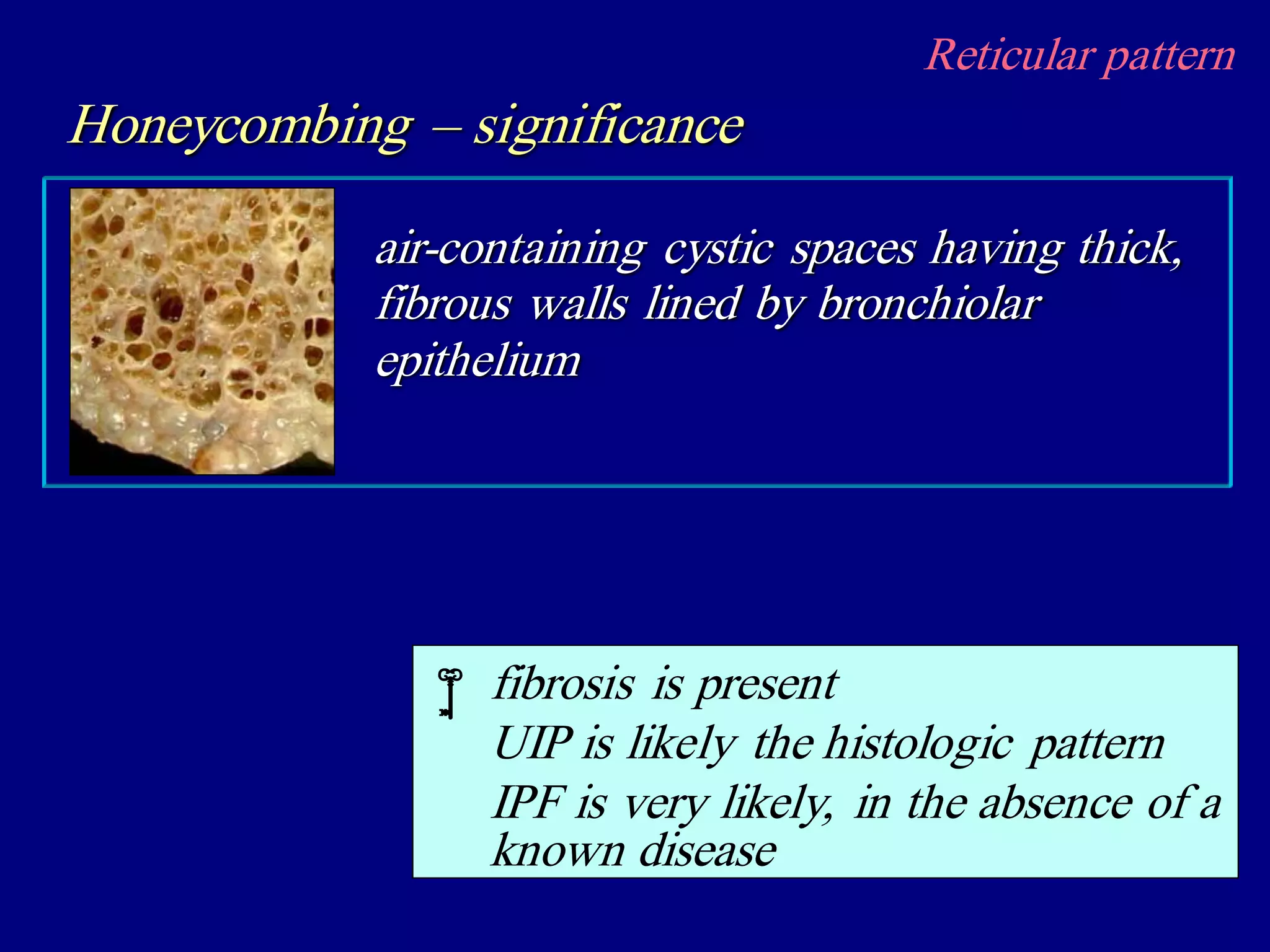
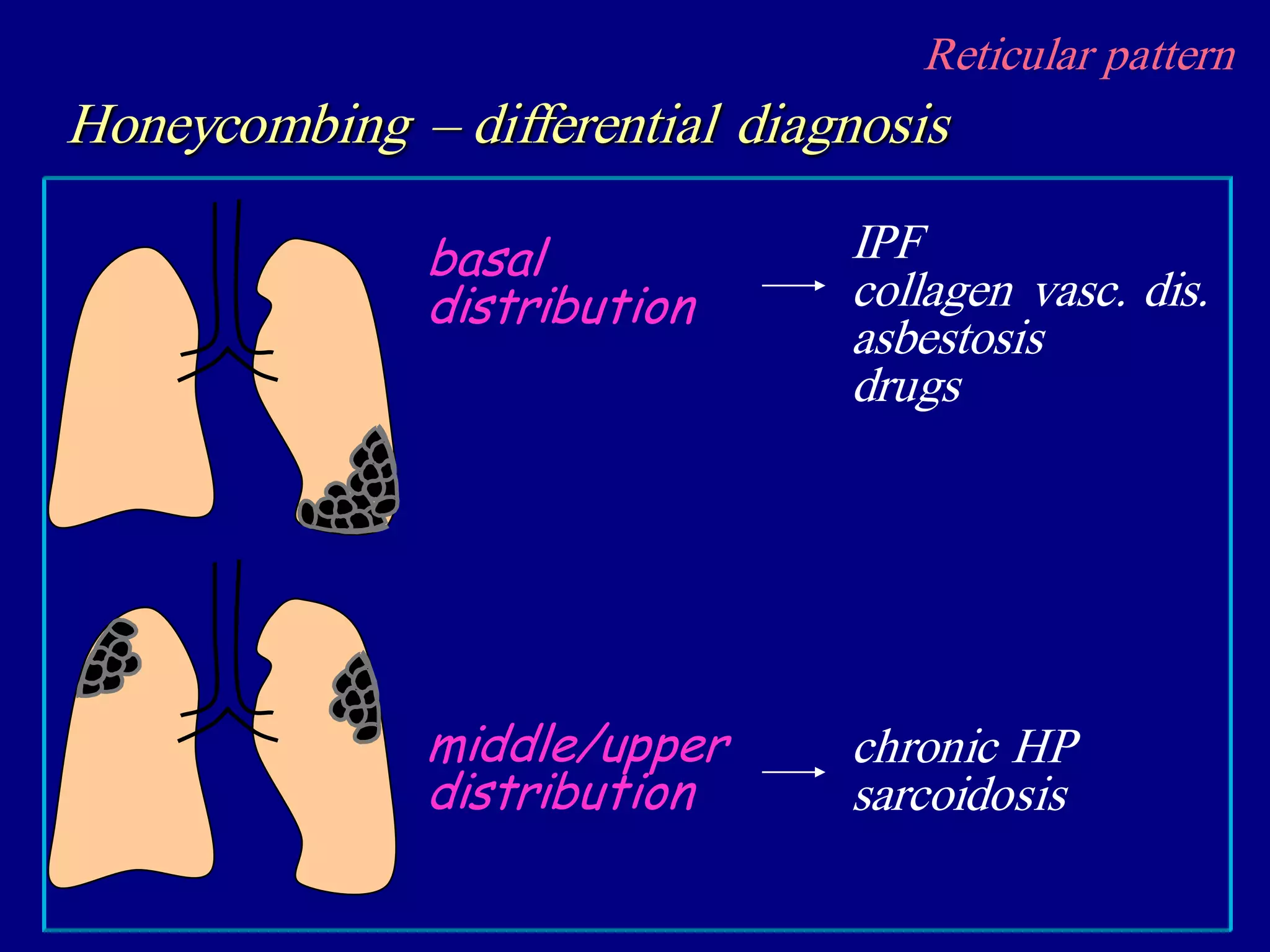
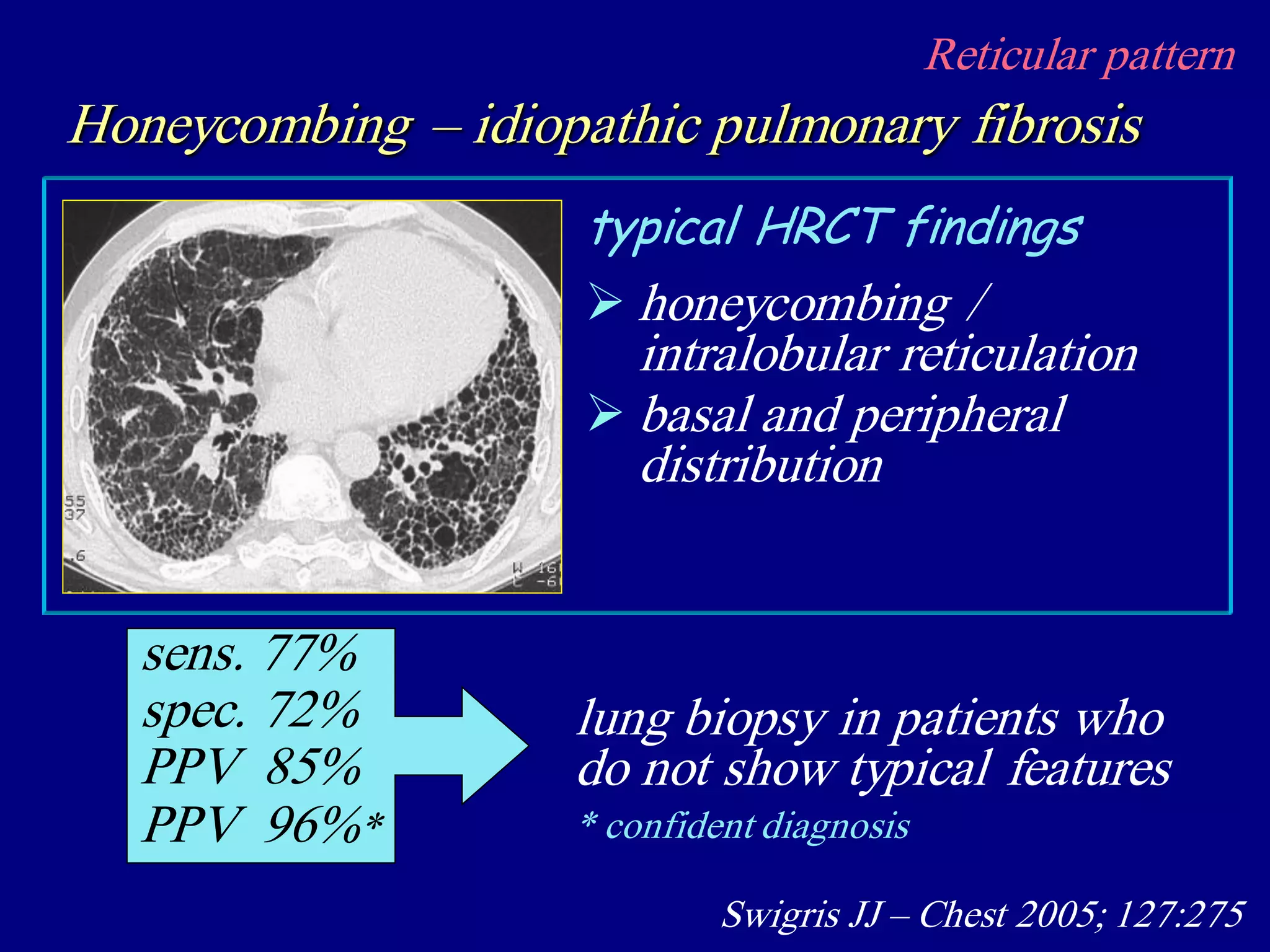
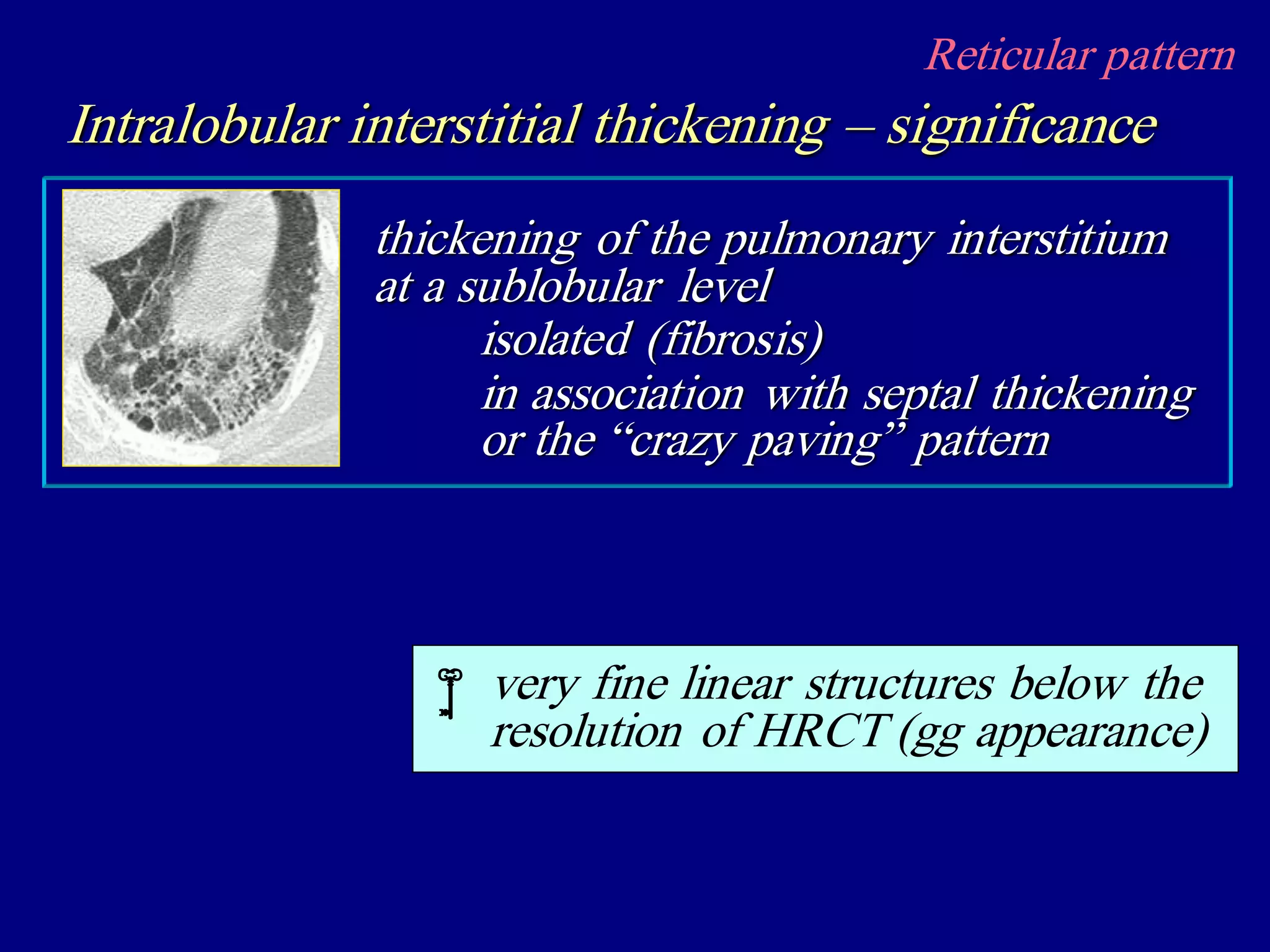
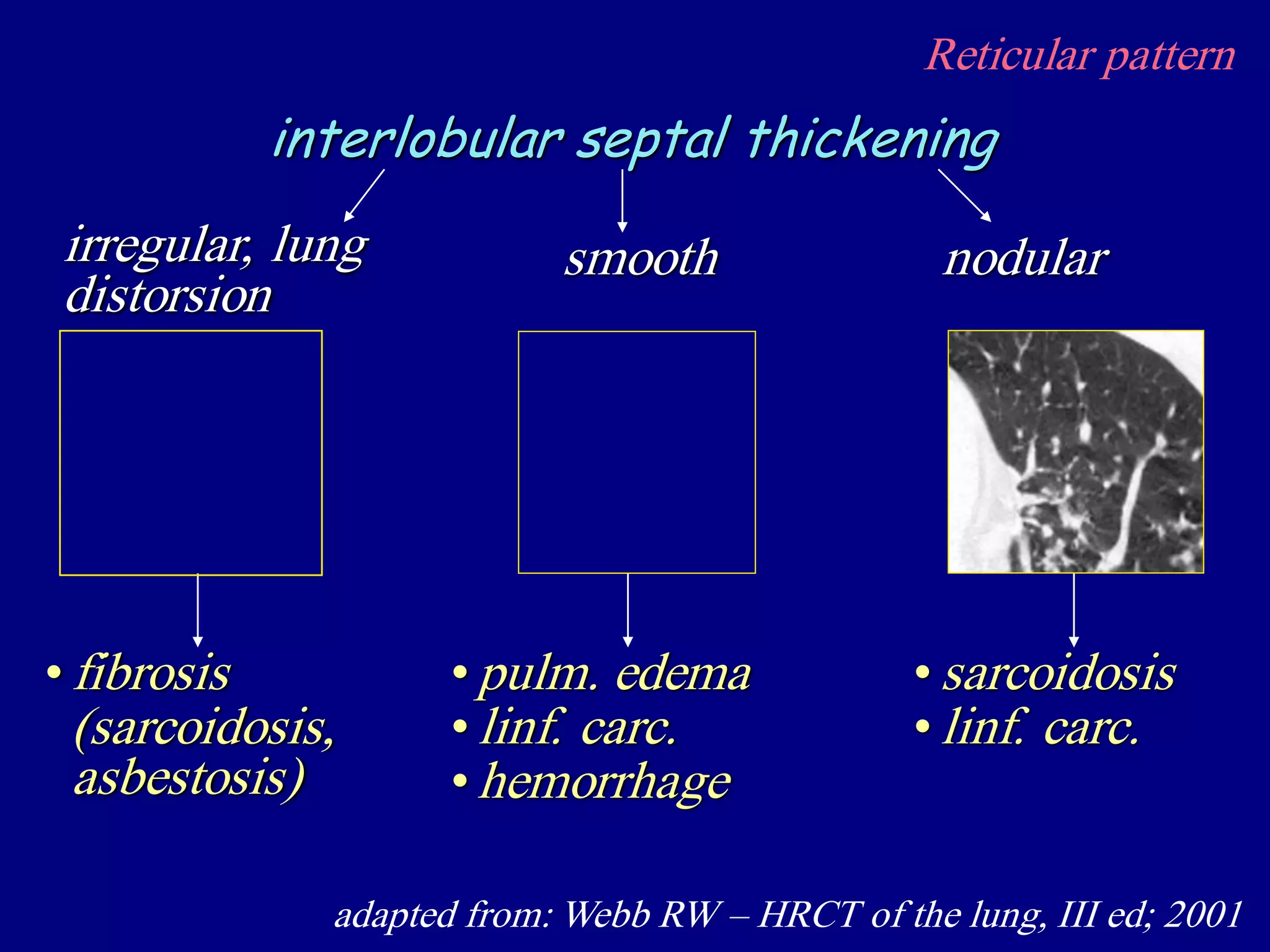
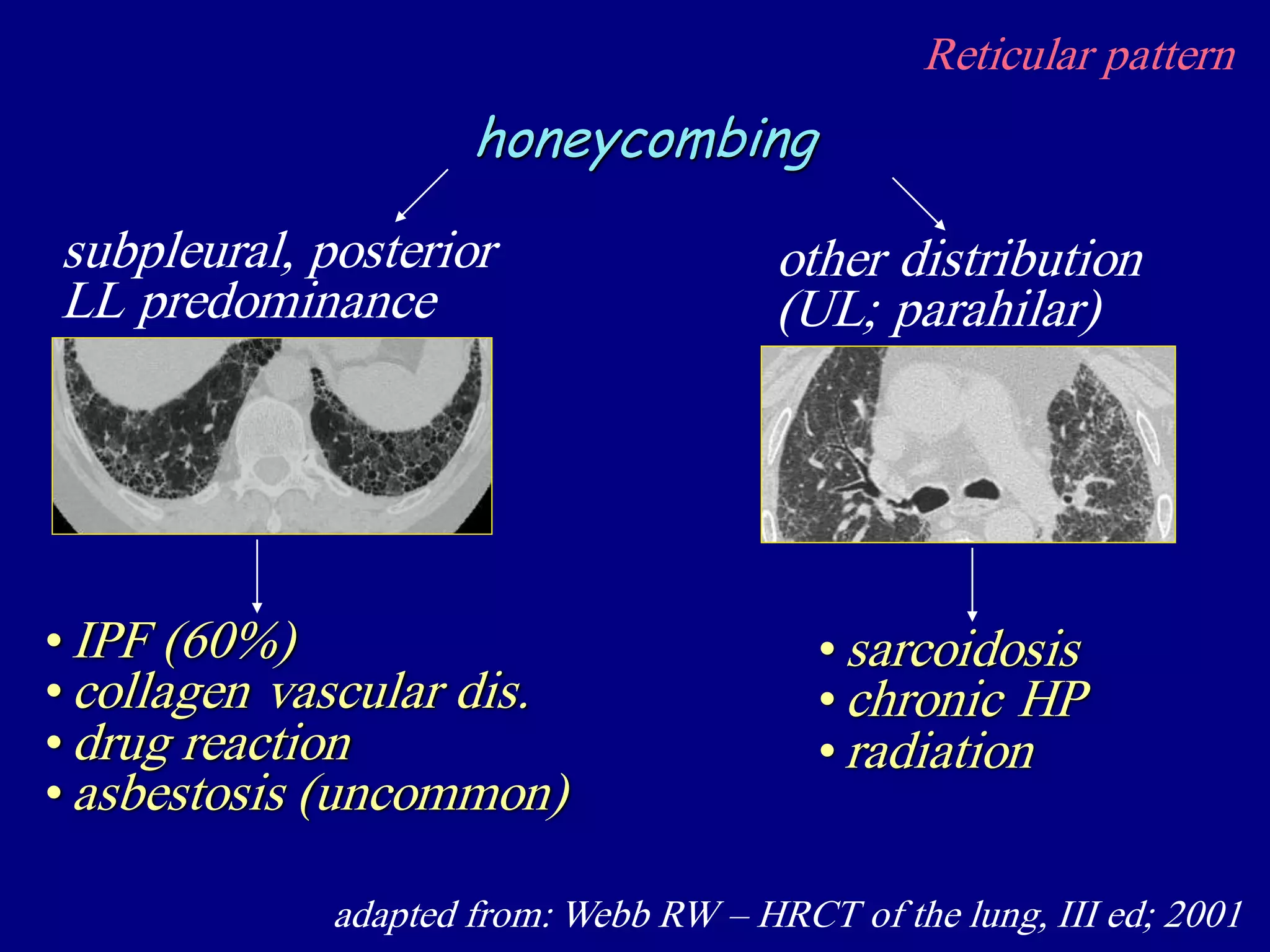
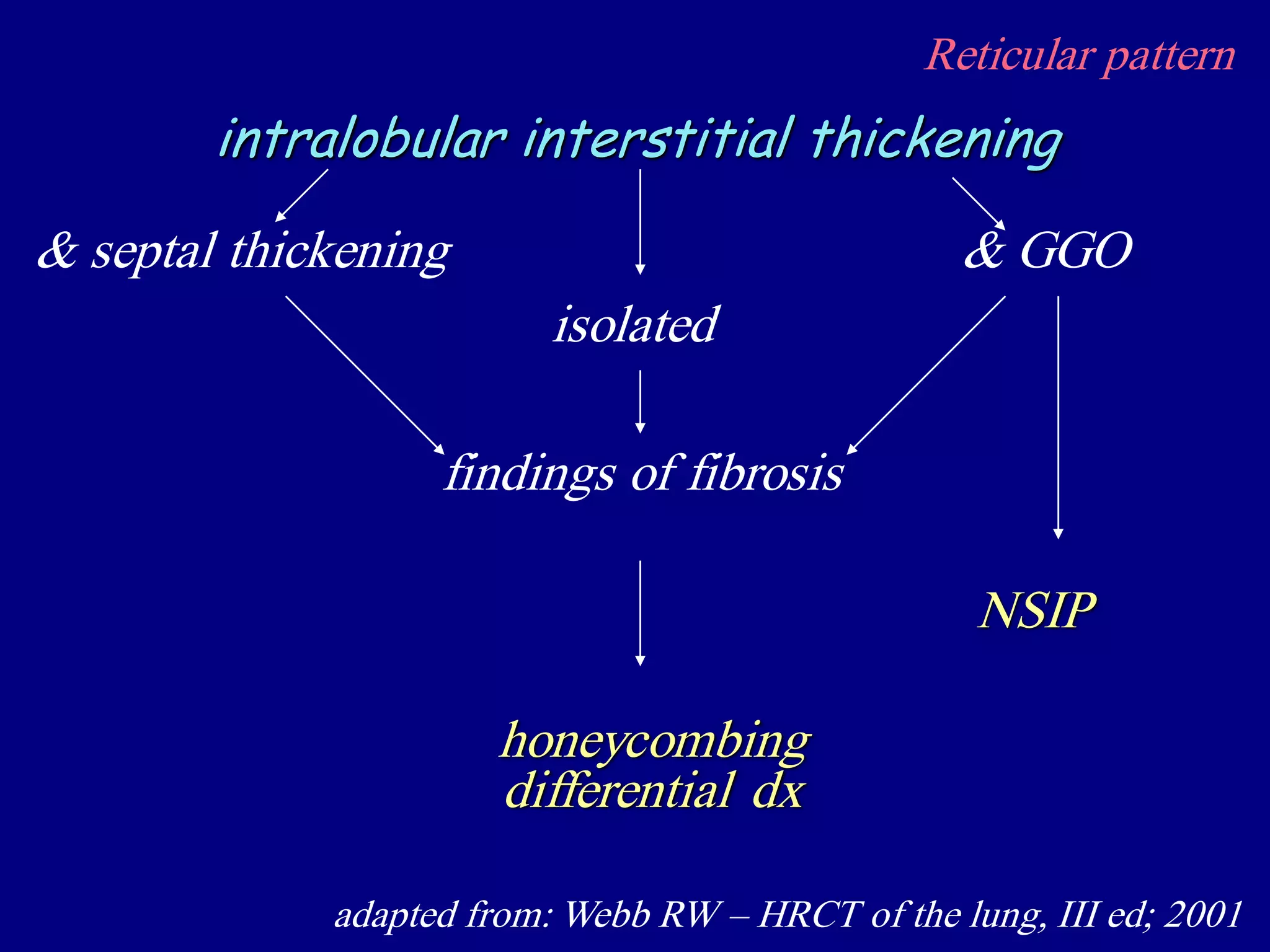
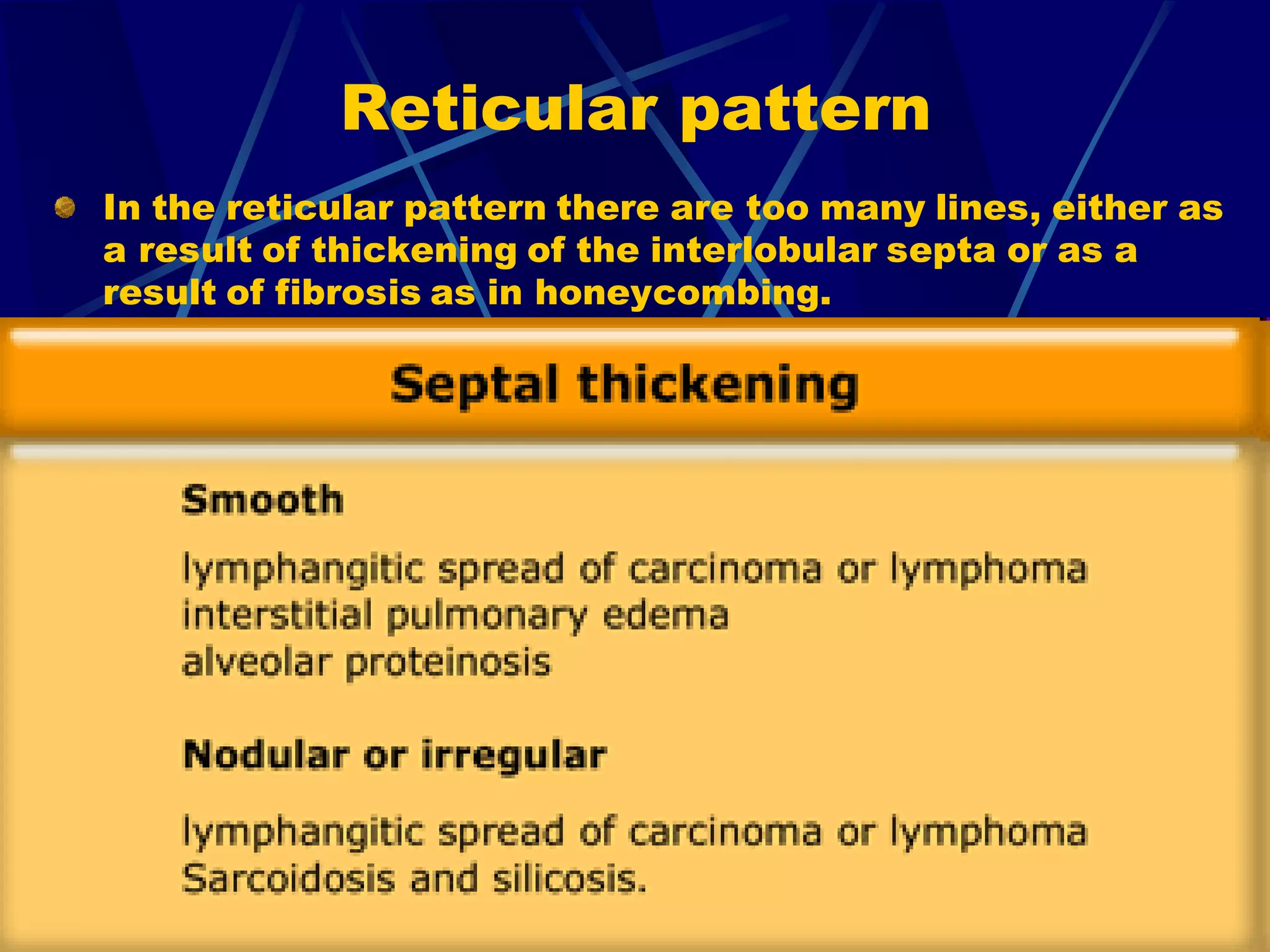
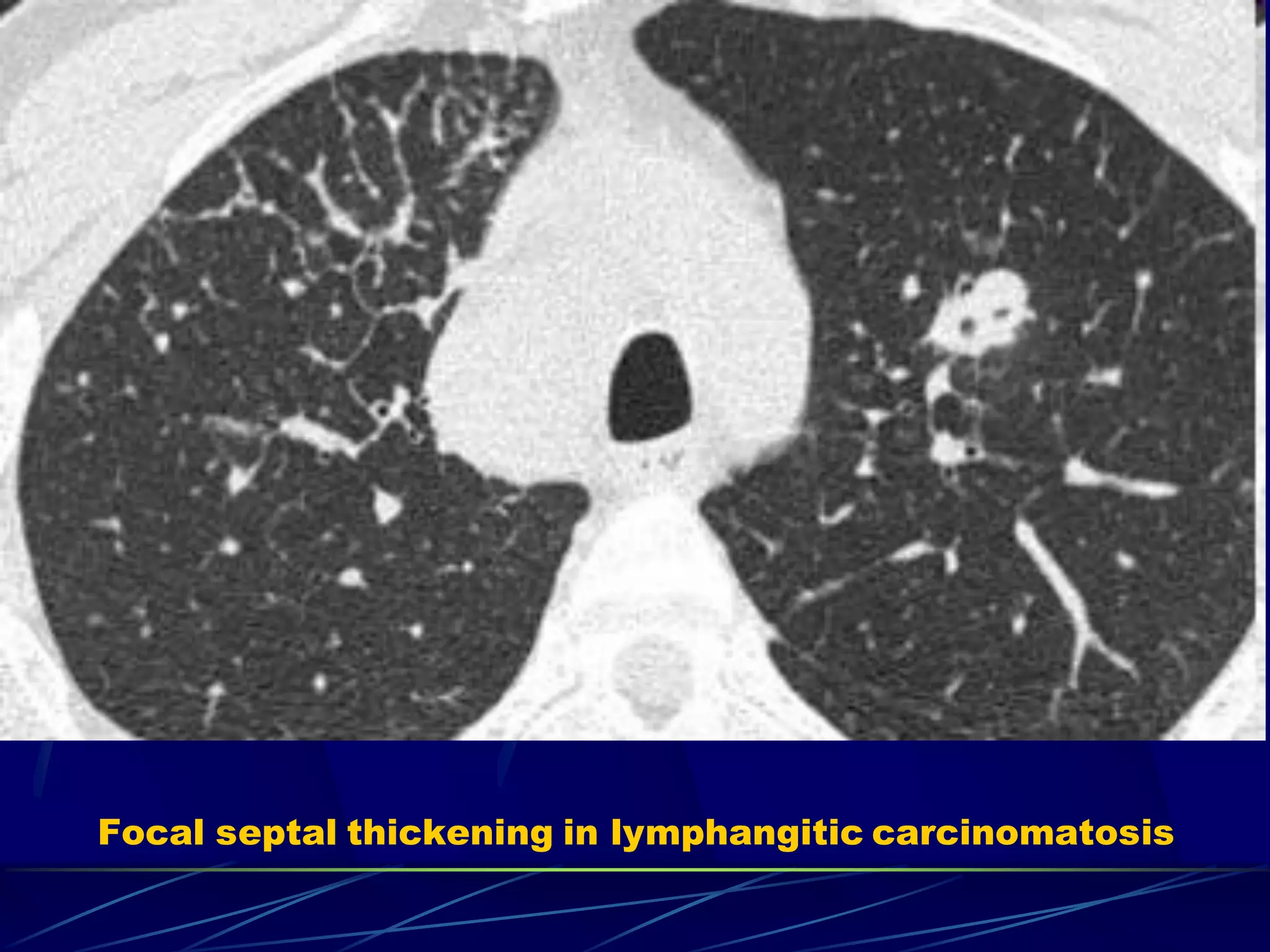
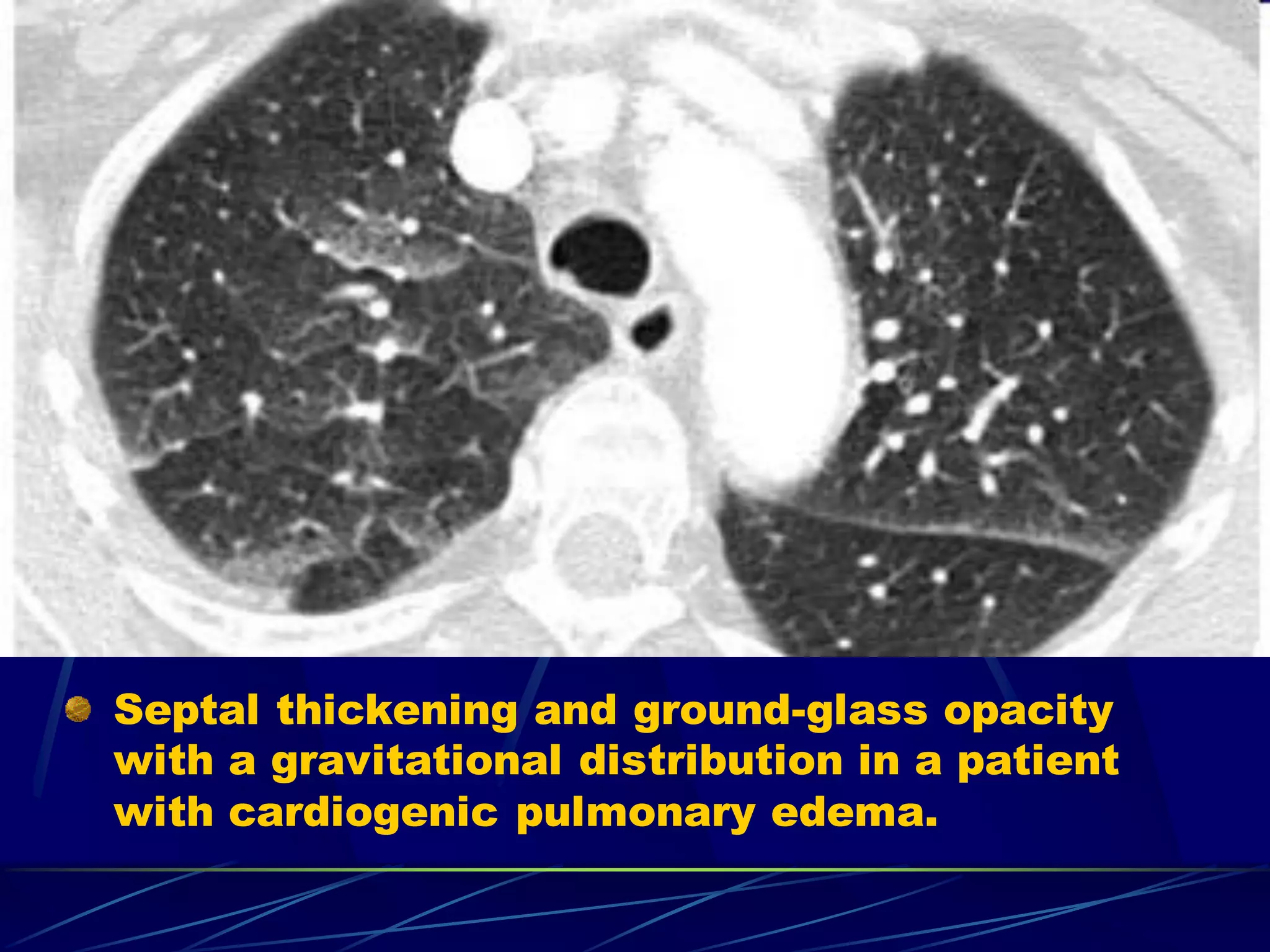
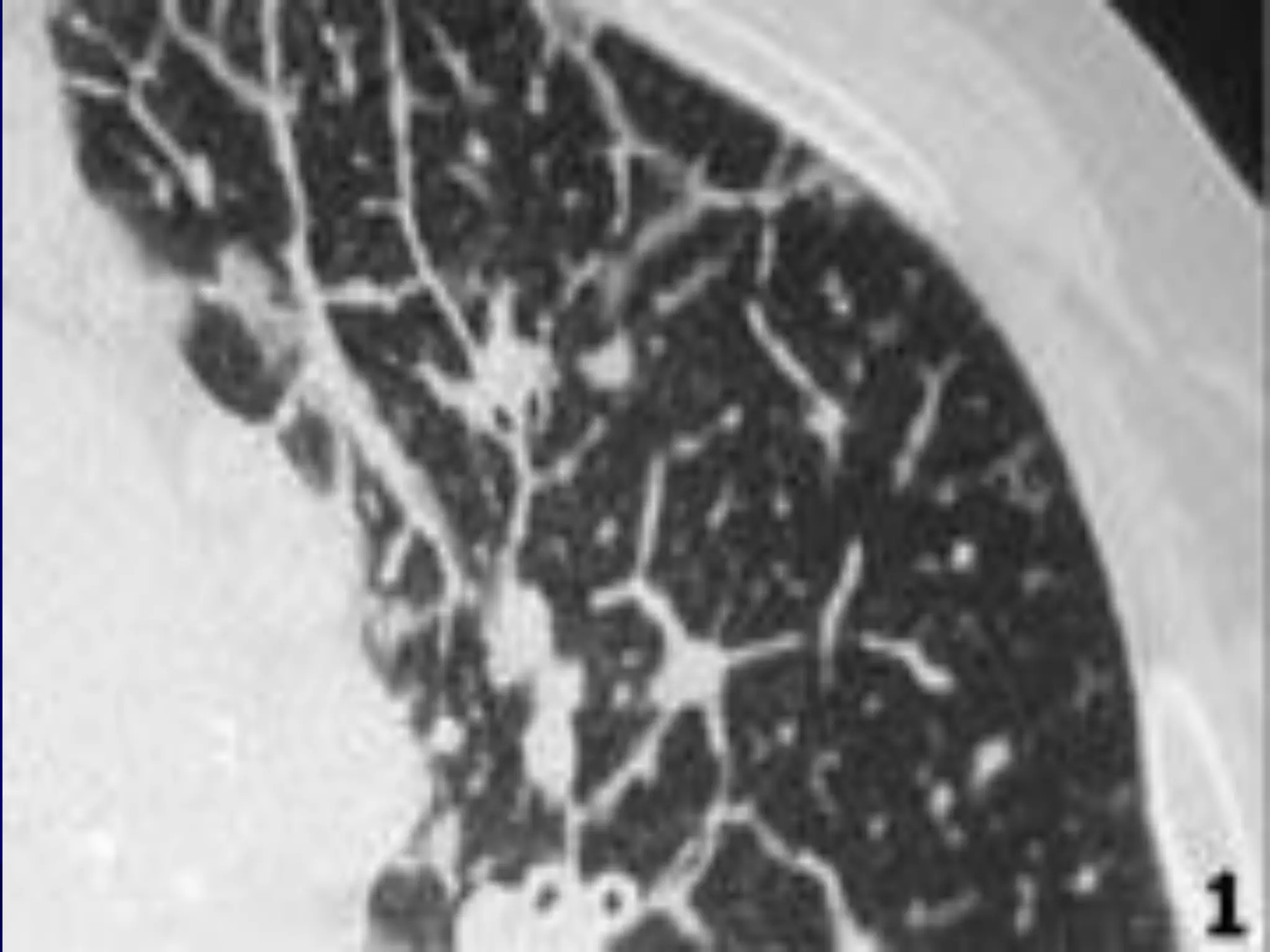
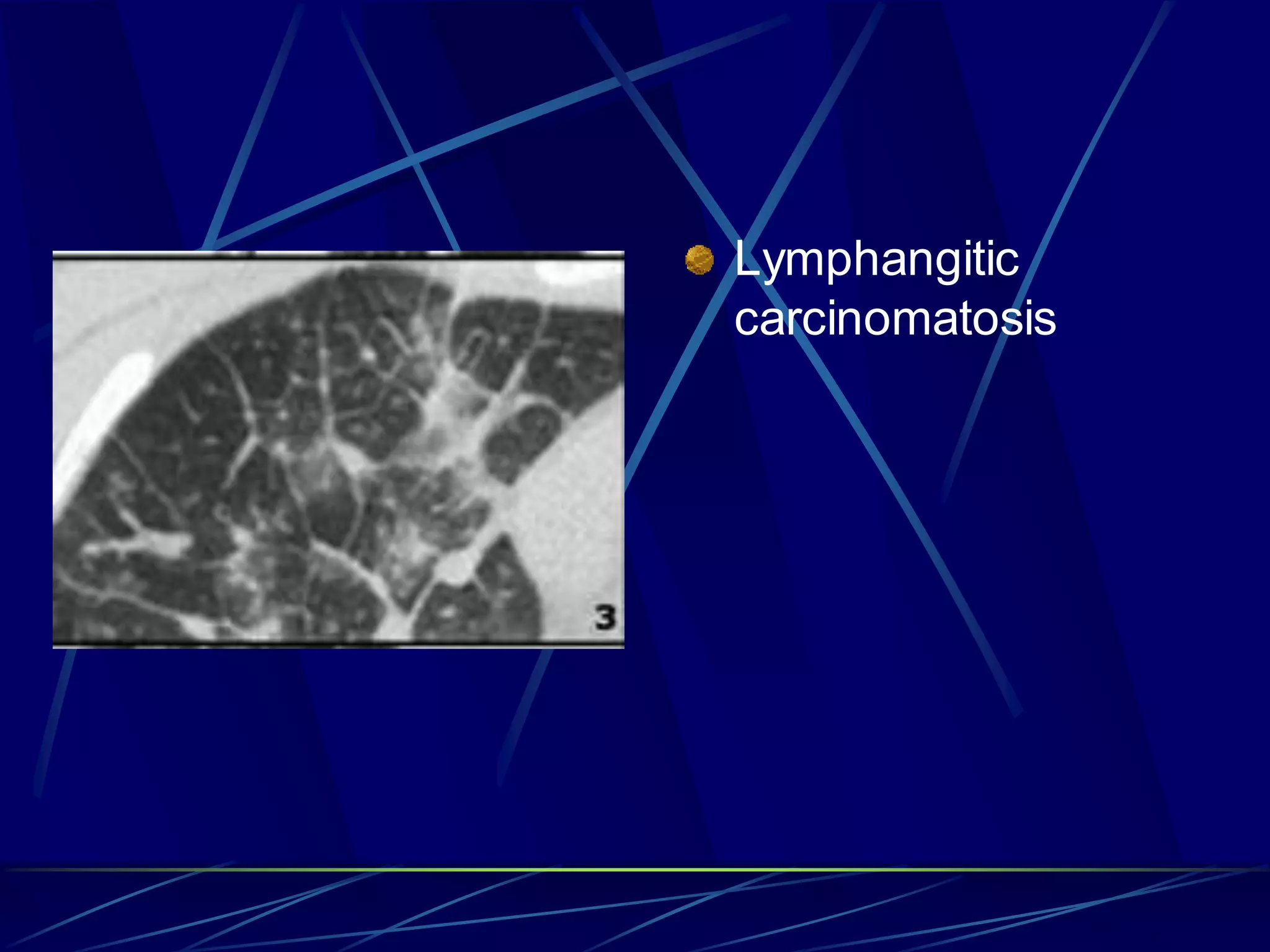
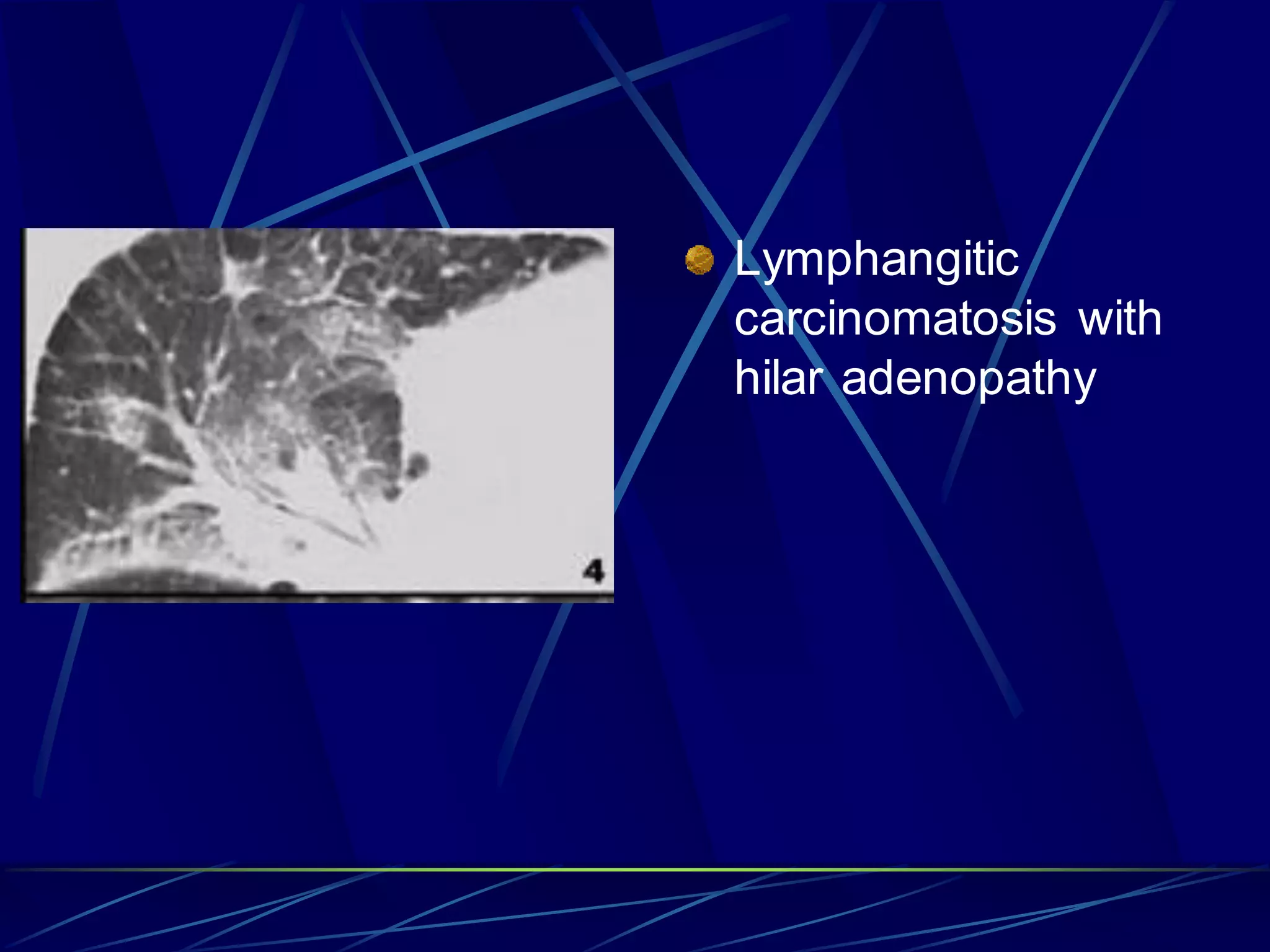
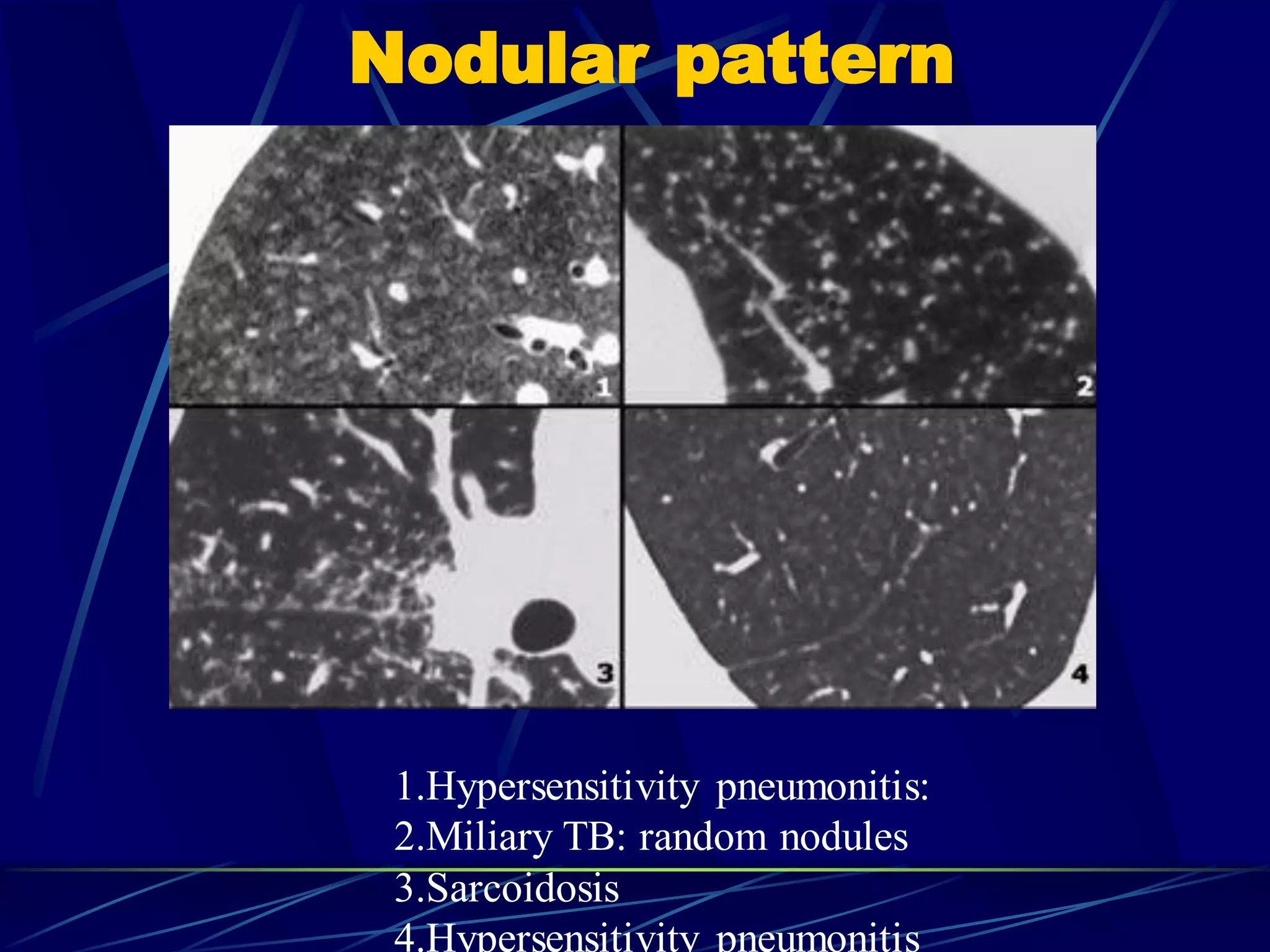
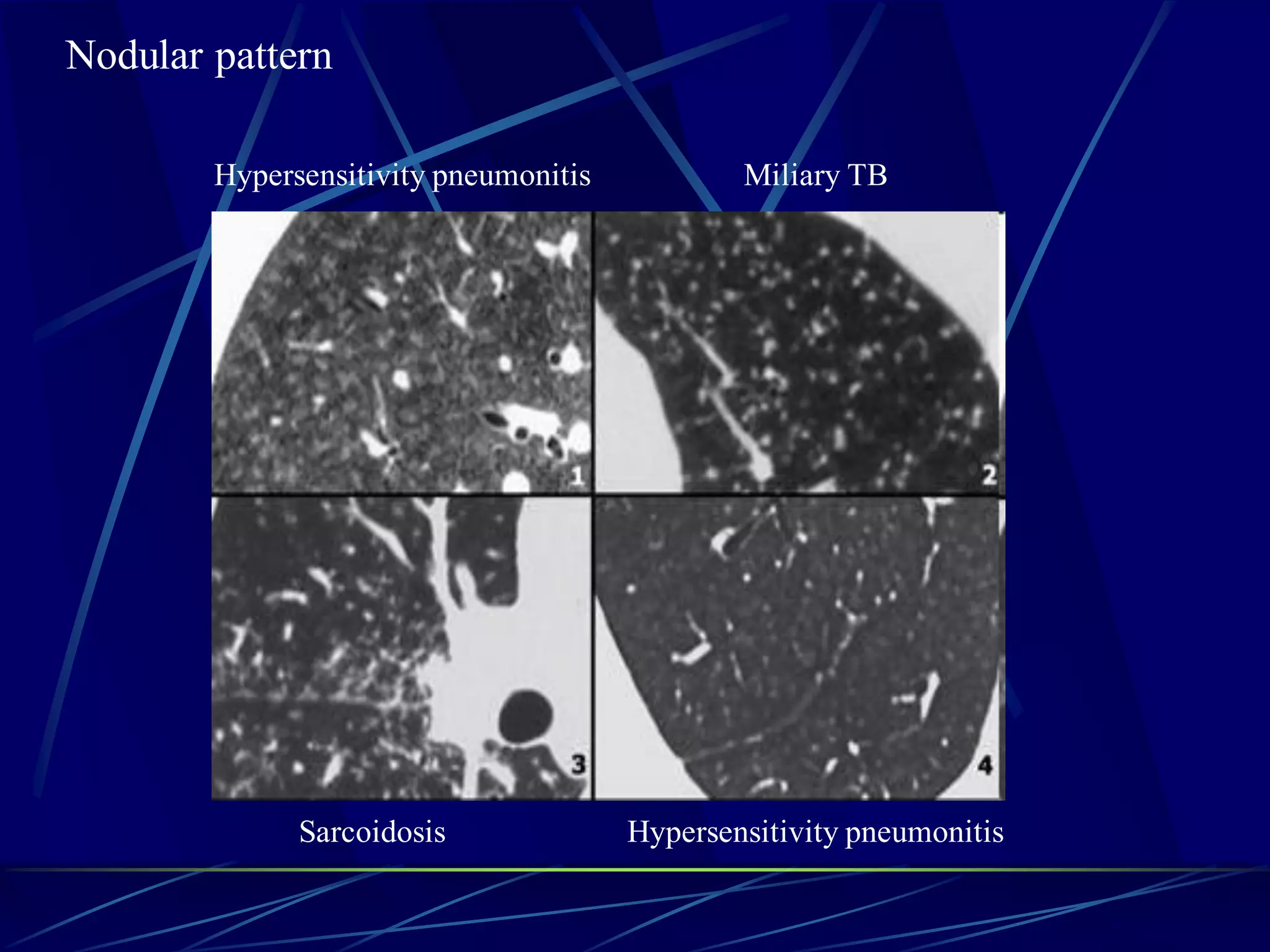
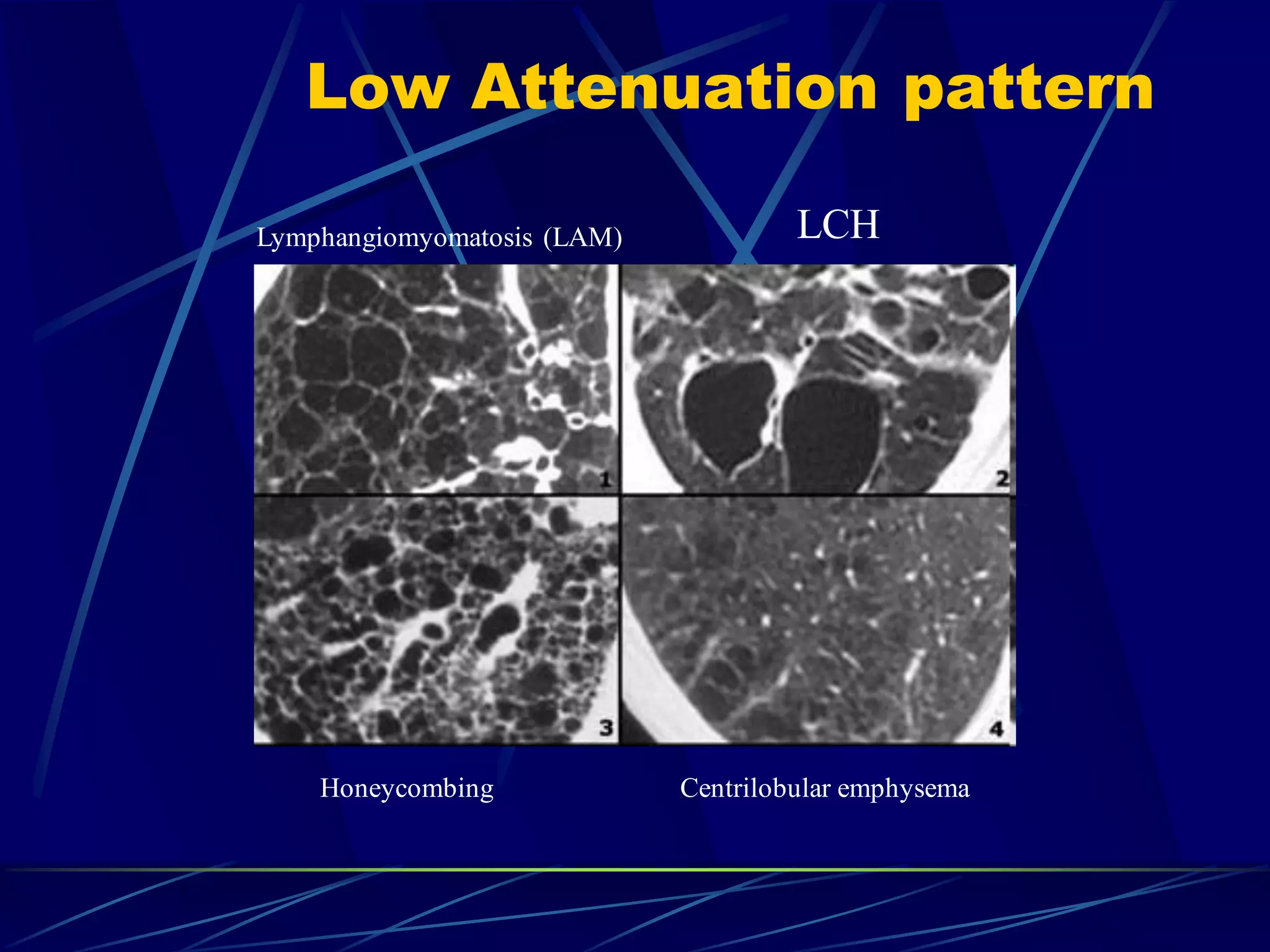
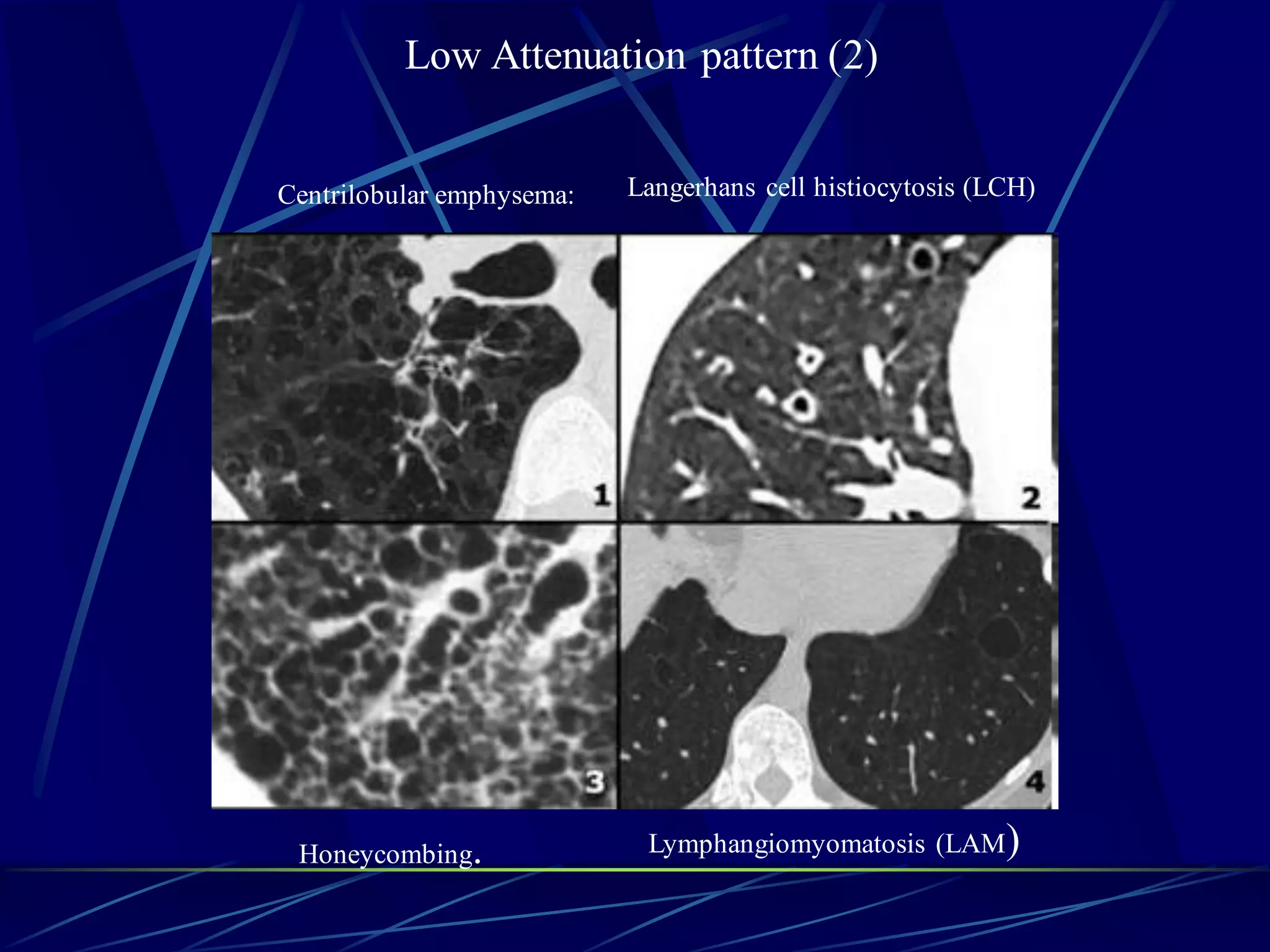
The document discusses the reticular pattern seen on CT scans of the lung. A reticular pattern results from the superimposition of irregular linear opacities, forming a mesh-like or network appearance. Reticular opacities can be fine, medium, or coarse depending on the width of the opacities. A classic reticular pattern is seen in pulmonary fibrosis where curvilinear opacities form small cystic honeycomb spaces along the pleural margins and bases. Potential causes of interlobular septal thickening seen on CT include pulmonary edema, lymphangitic carcinomatosis, fibrosis, and sarcoidosis. Honeycombing signifies the presence of fibrosis and is seen commonly in idiopathic