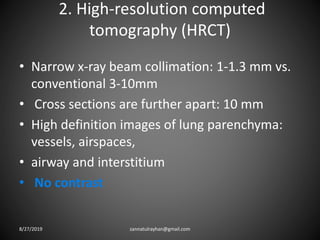
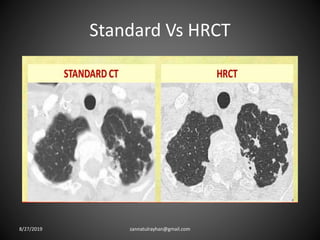
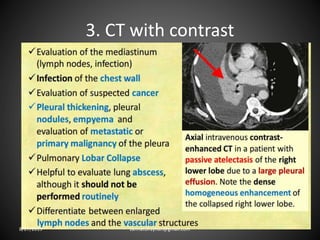
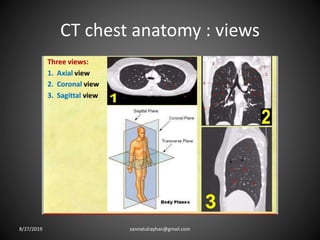
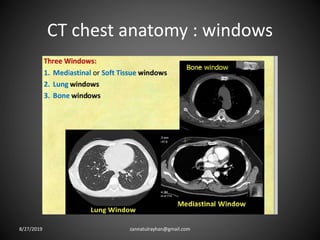
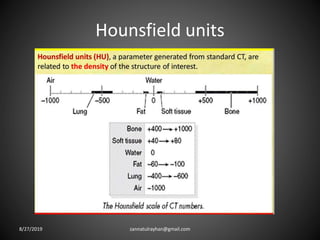
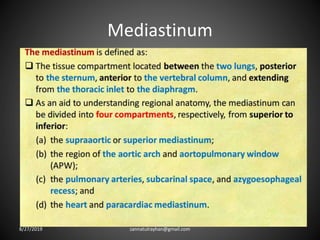
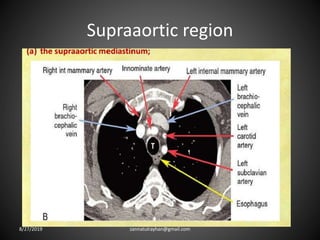
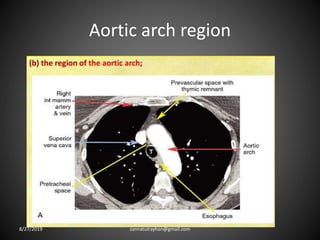
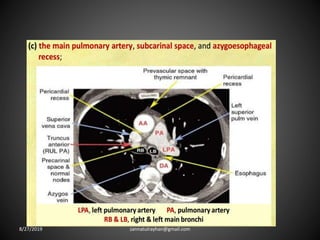
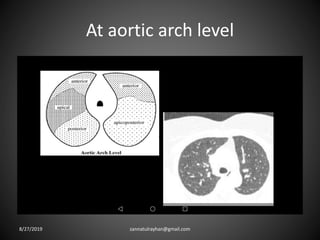
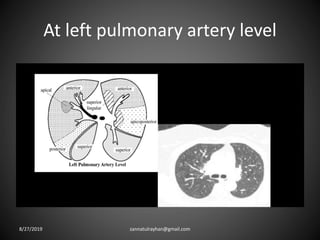
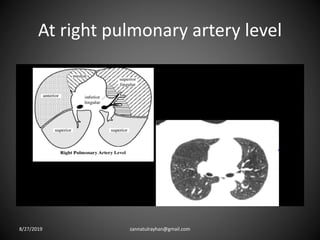
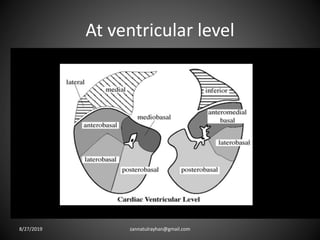
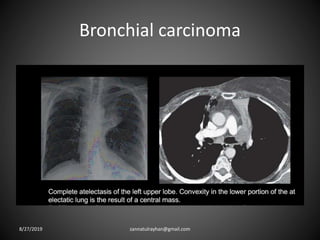
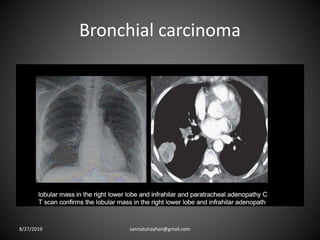
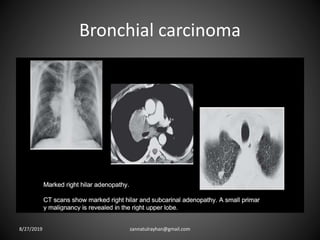
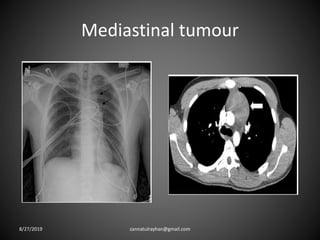
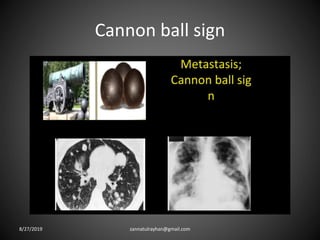
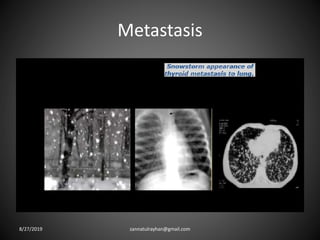
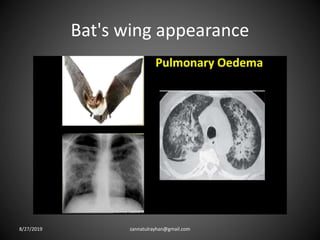
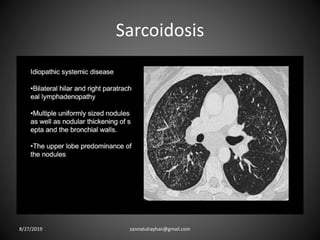
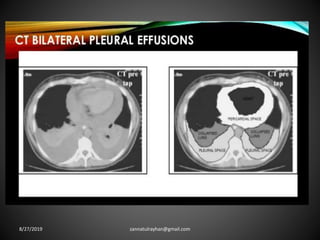
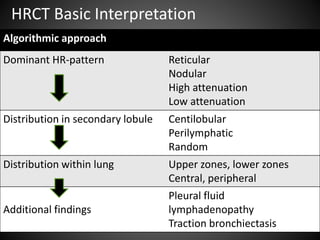
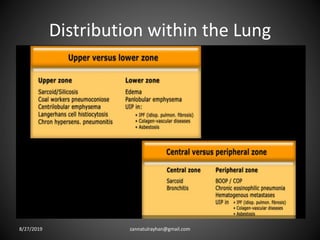
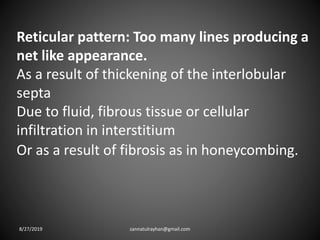
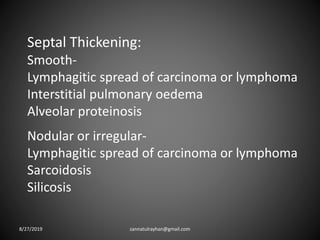
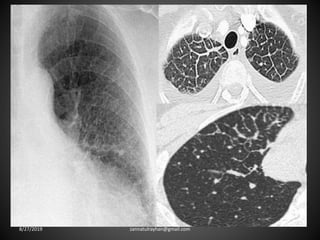
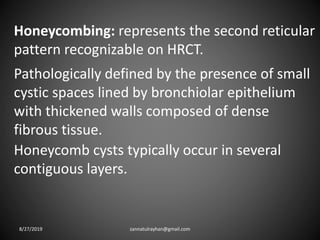
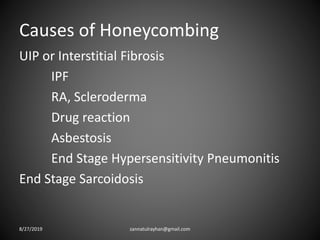
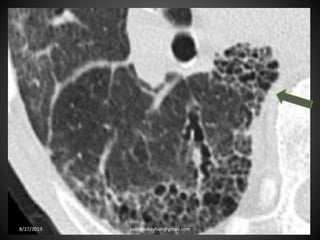
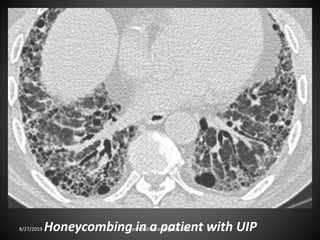
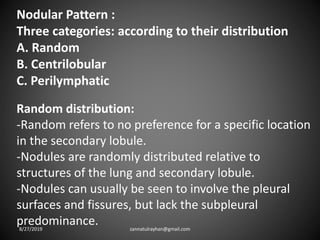
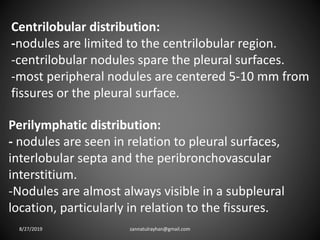
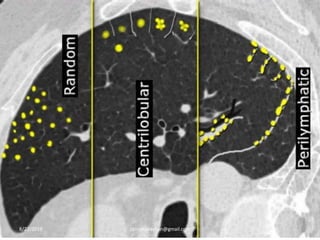
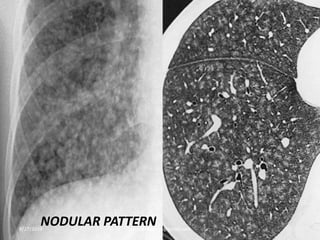
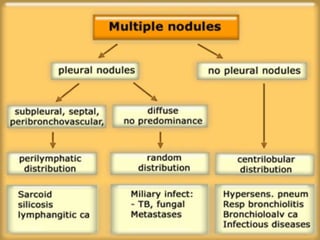
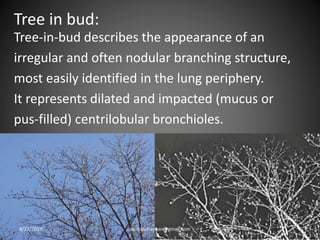
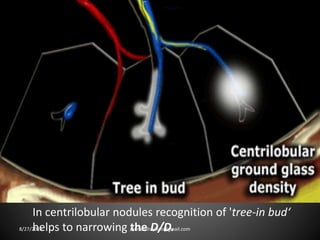
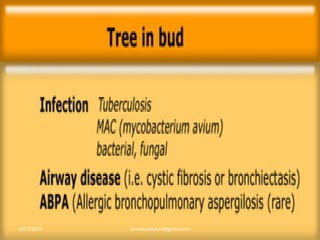
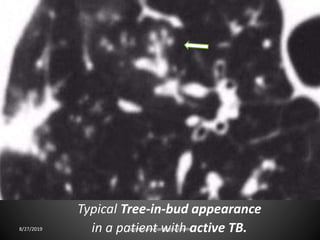
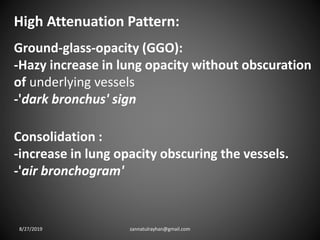
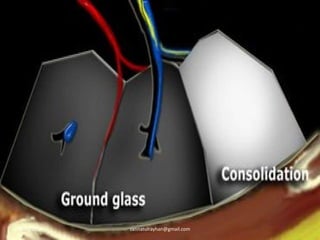
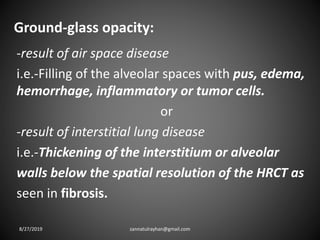
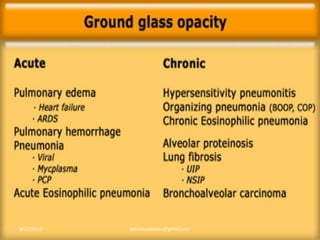
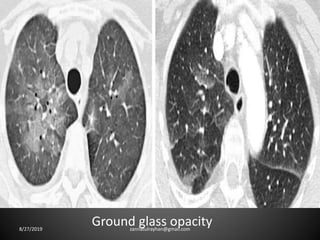
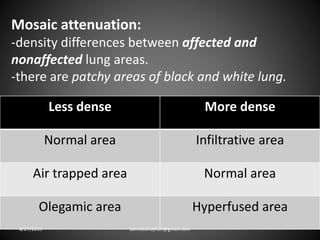
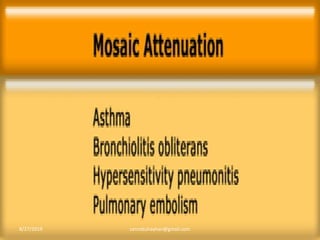
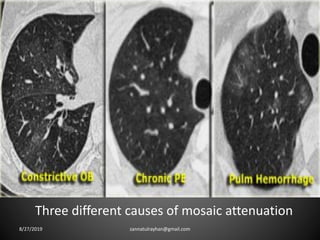
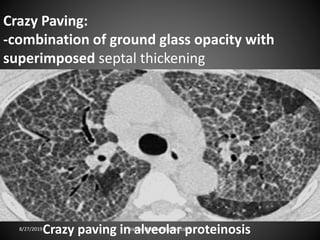
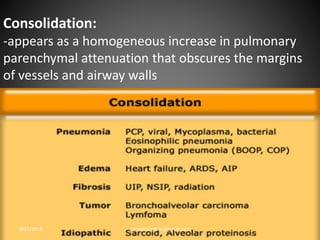
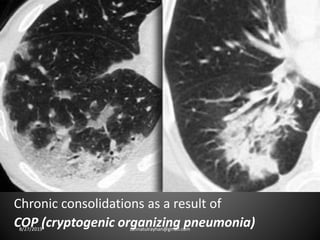
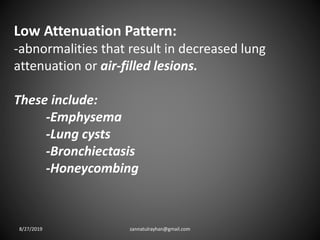
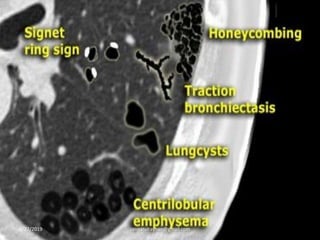
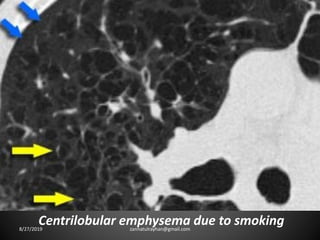
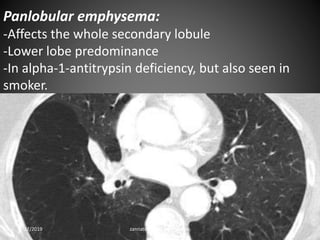
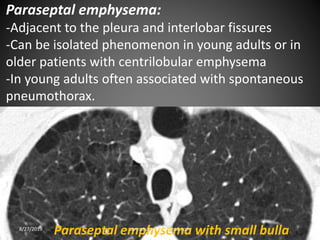
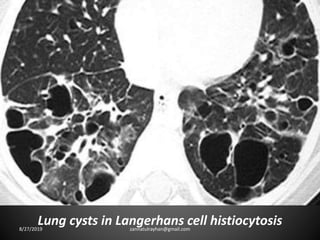
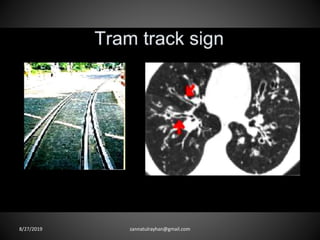
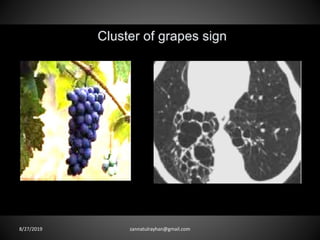
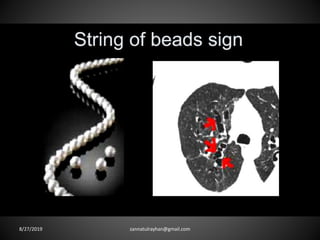
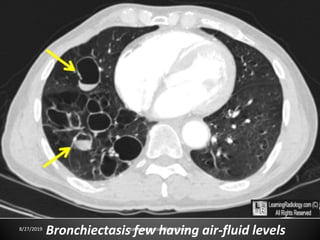
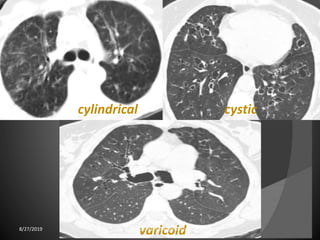
This document provides an overview of CT chest imaging, including standard CT, high-resolution CT, and their indications. It discusses CT chest anatomy and windows. Common lung pathologies seen on standard CT like bronchial carcinoma, collapse, and metastasis are described. Interpretation of high-resolution CT focuses on patterns such as reticular, nodular, ground glass opacity, and consolidation. Specific findings including honeycombing, tree-in-bud, mosaic attenuation, and crazy paving are explained. The document concludes with a discussion of low attenuation patterns including emphysema, lung cysts, and bronchiectasis.