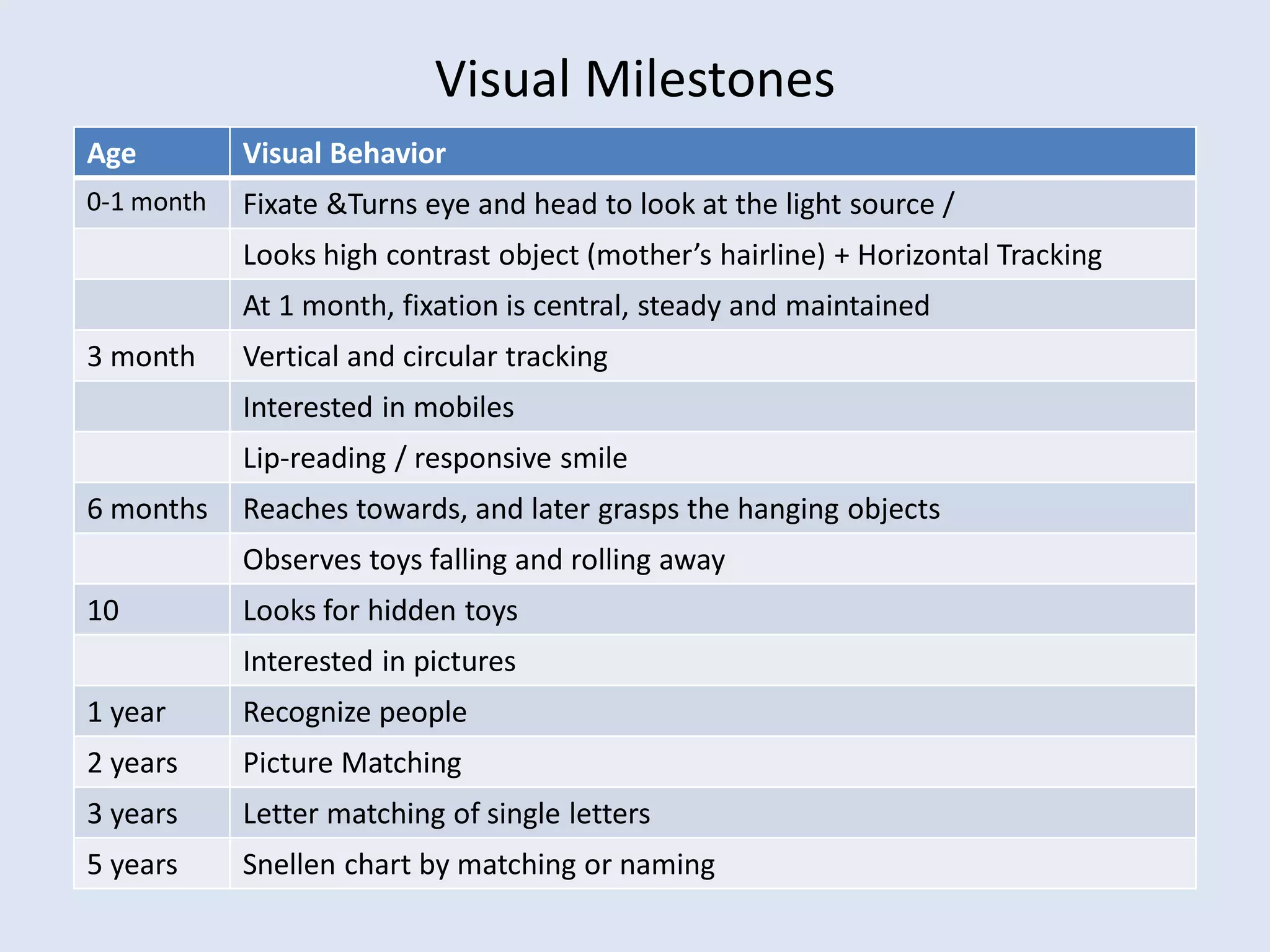
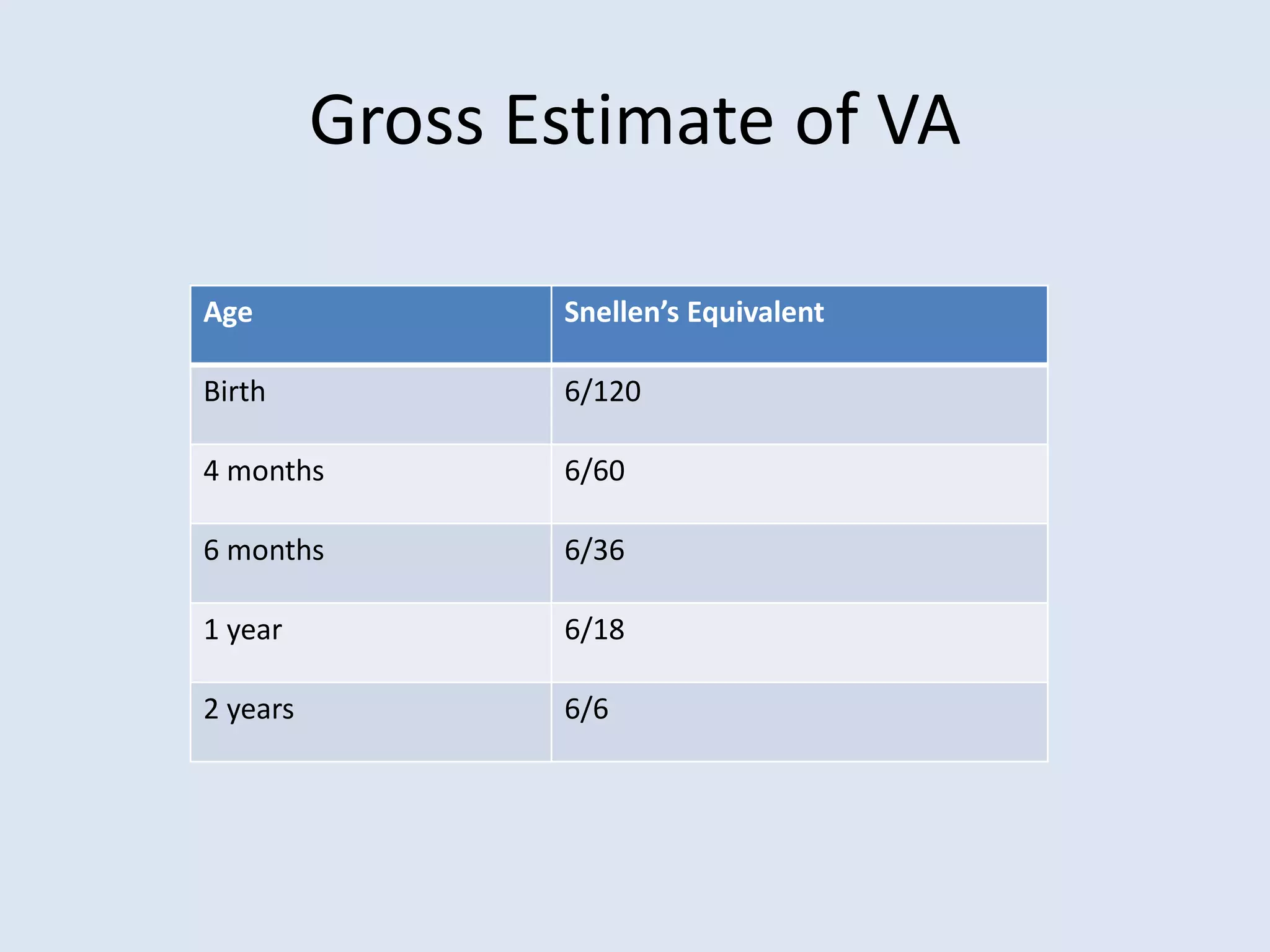
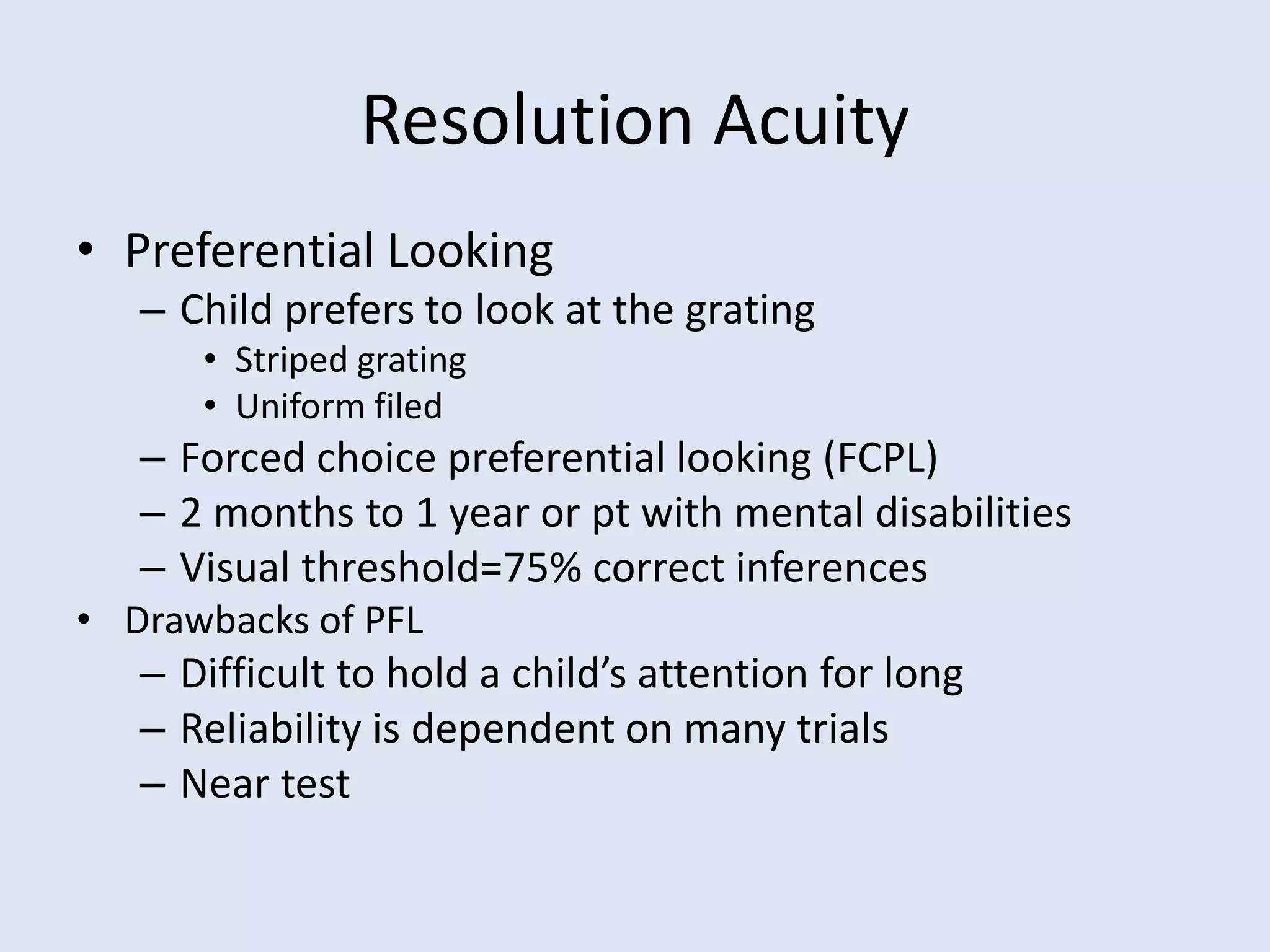
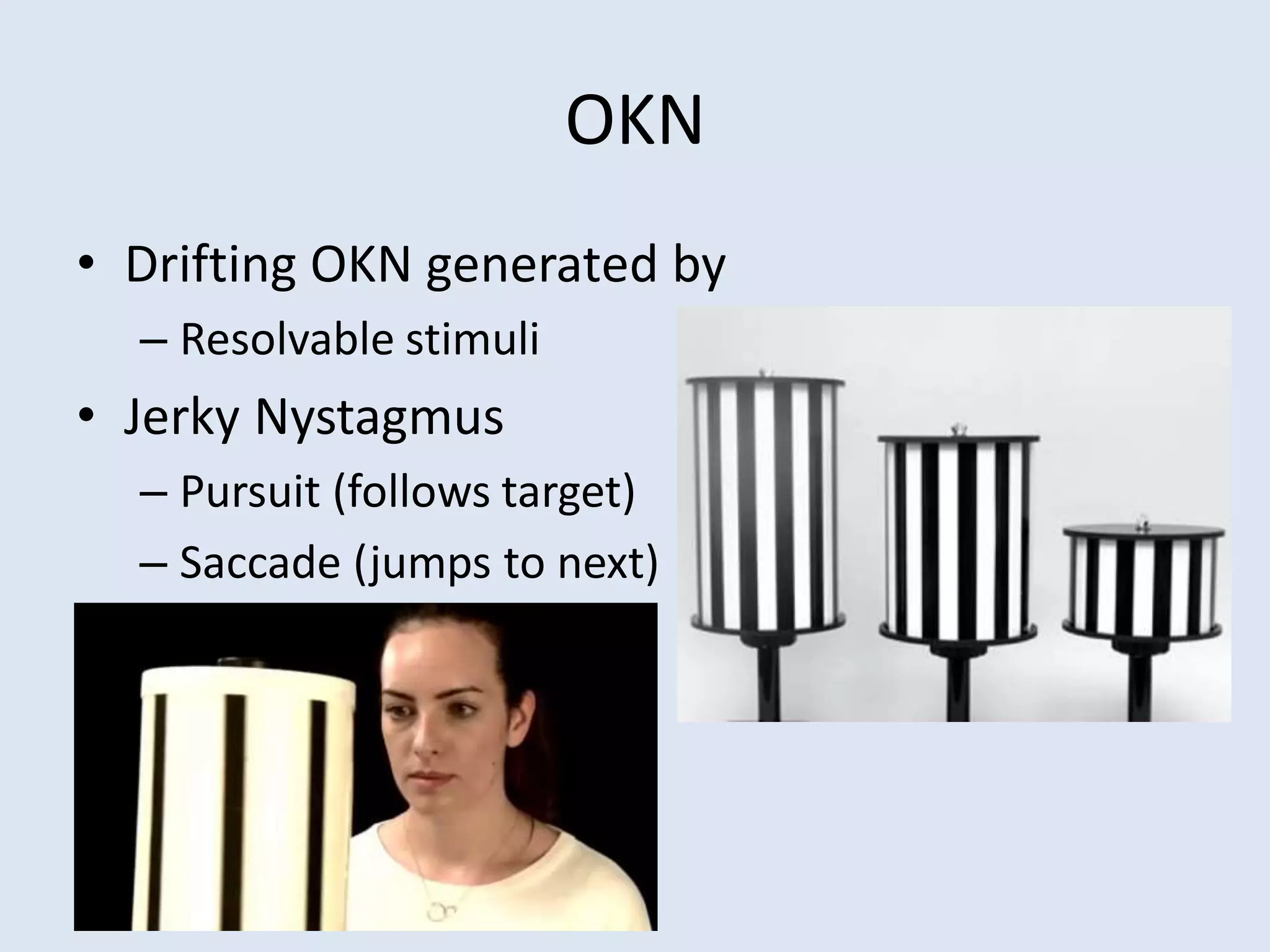
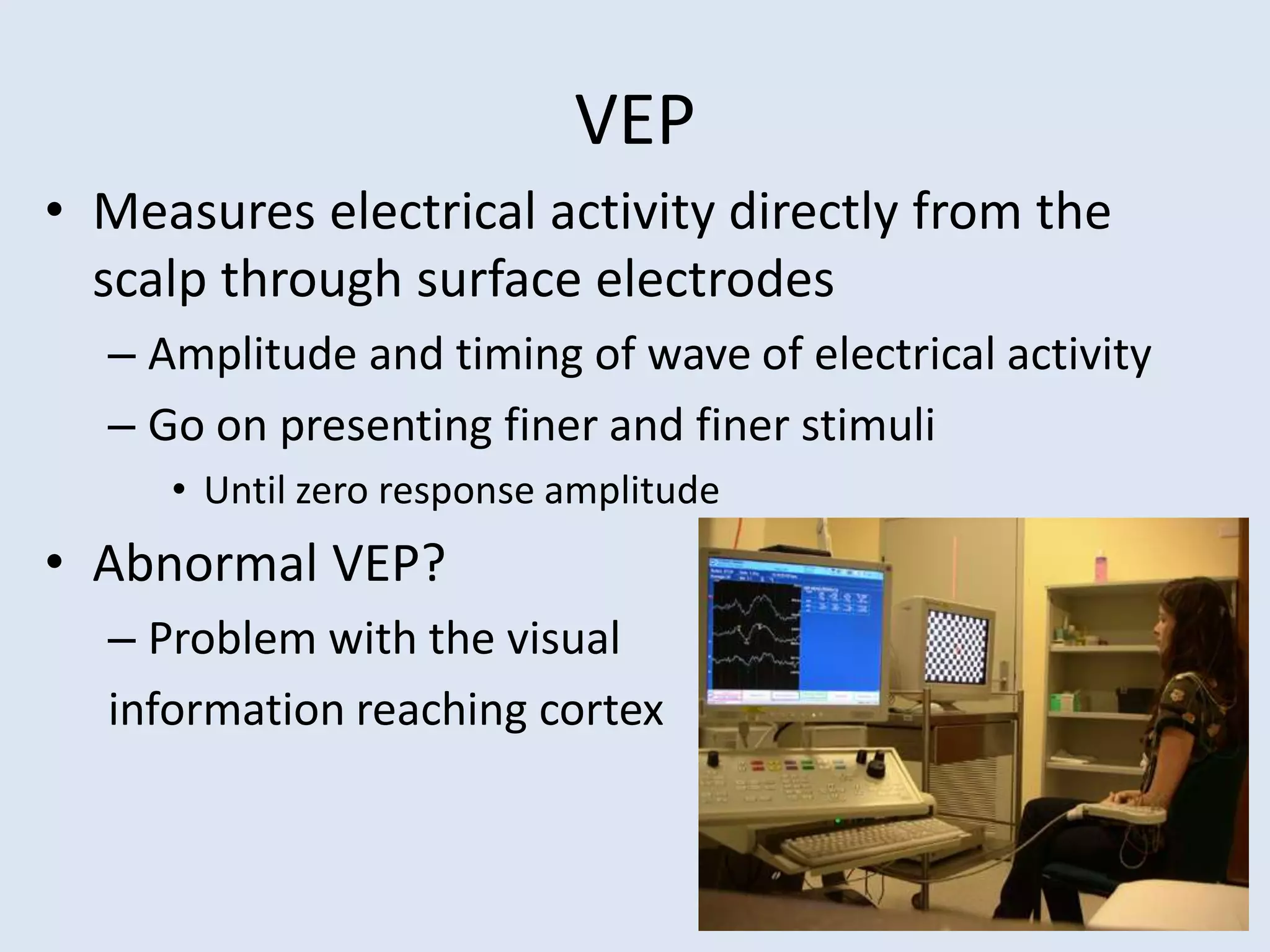
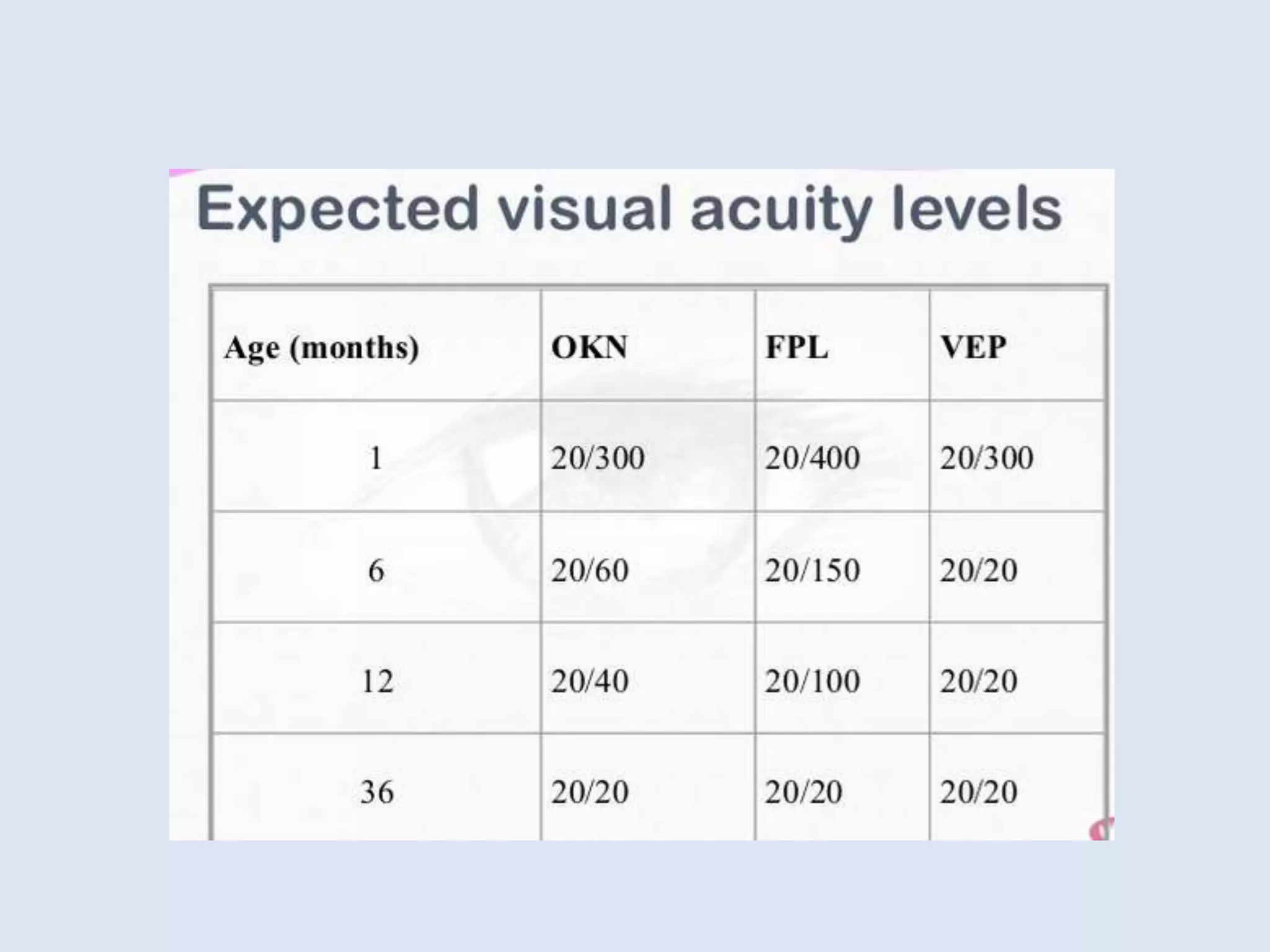
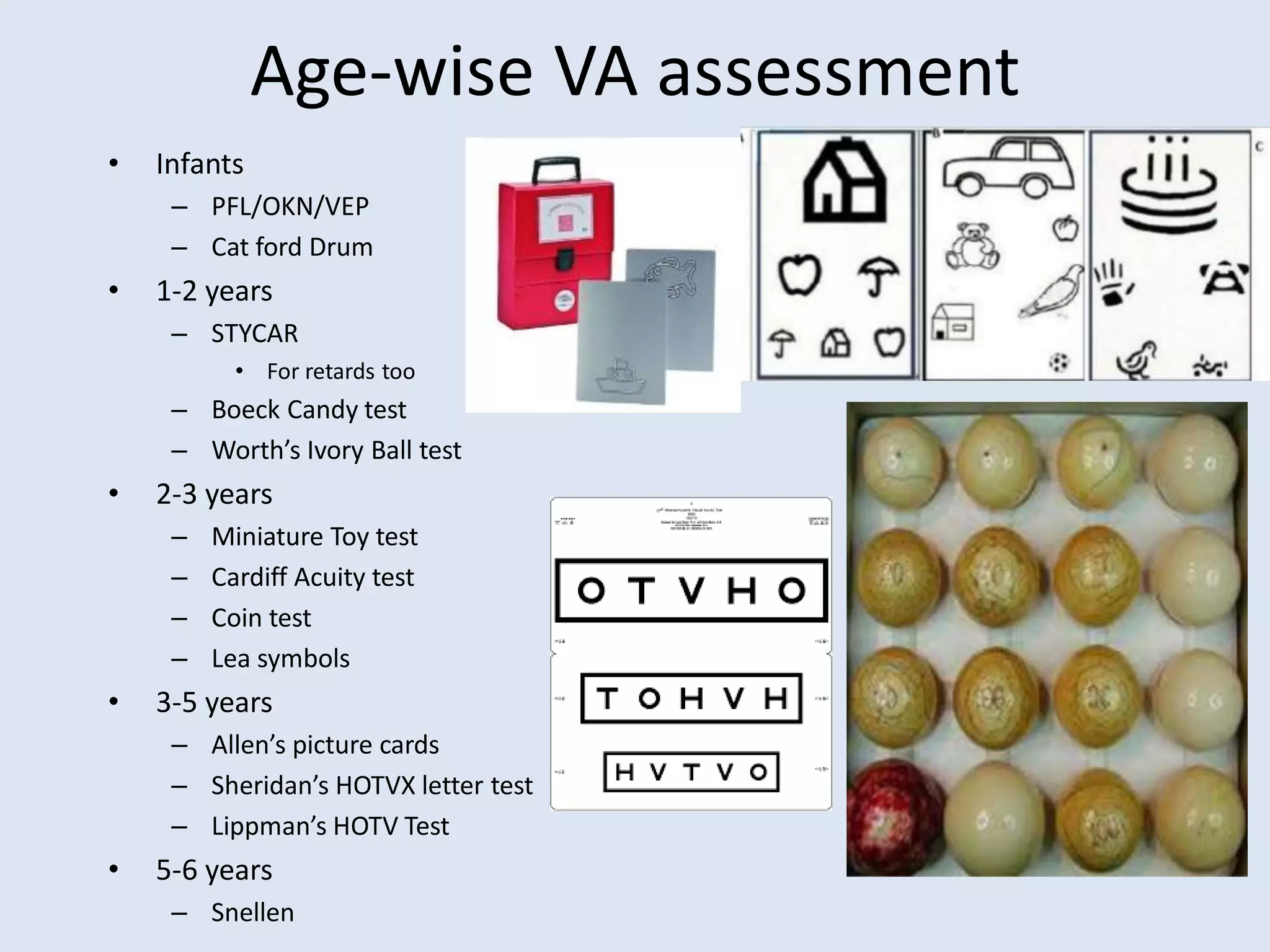
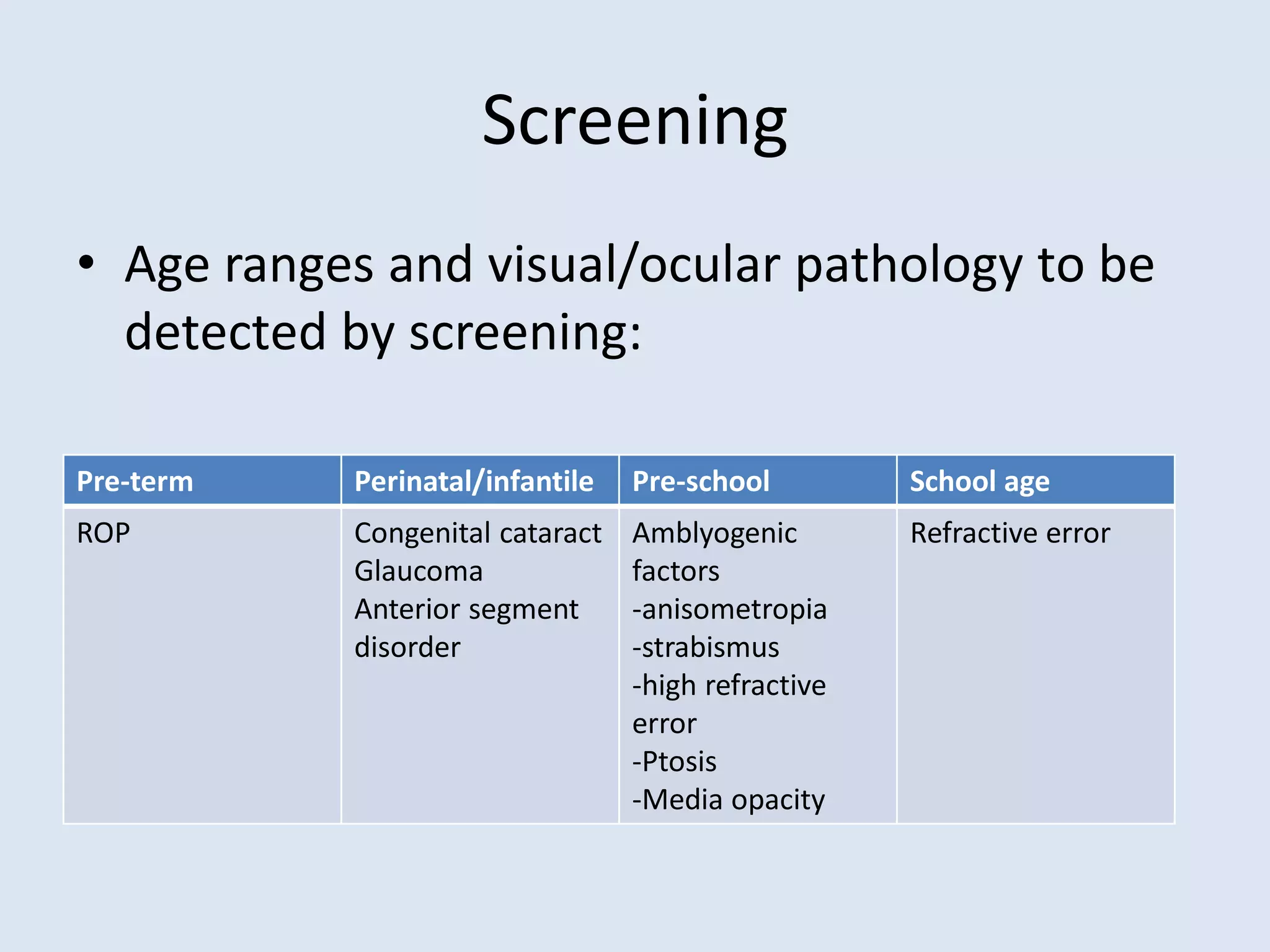
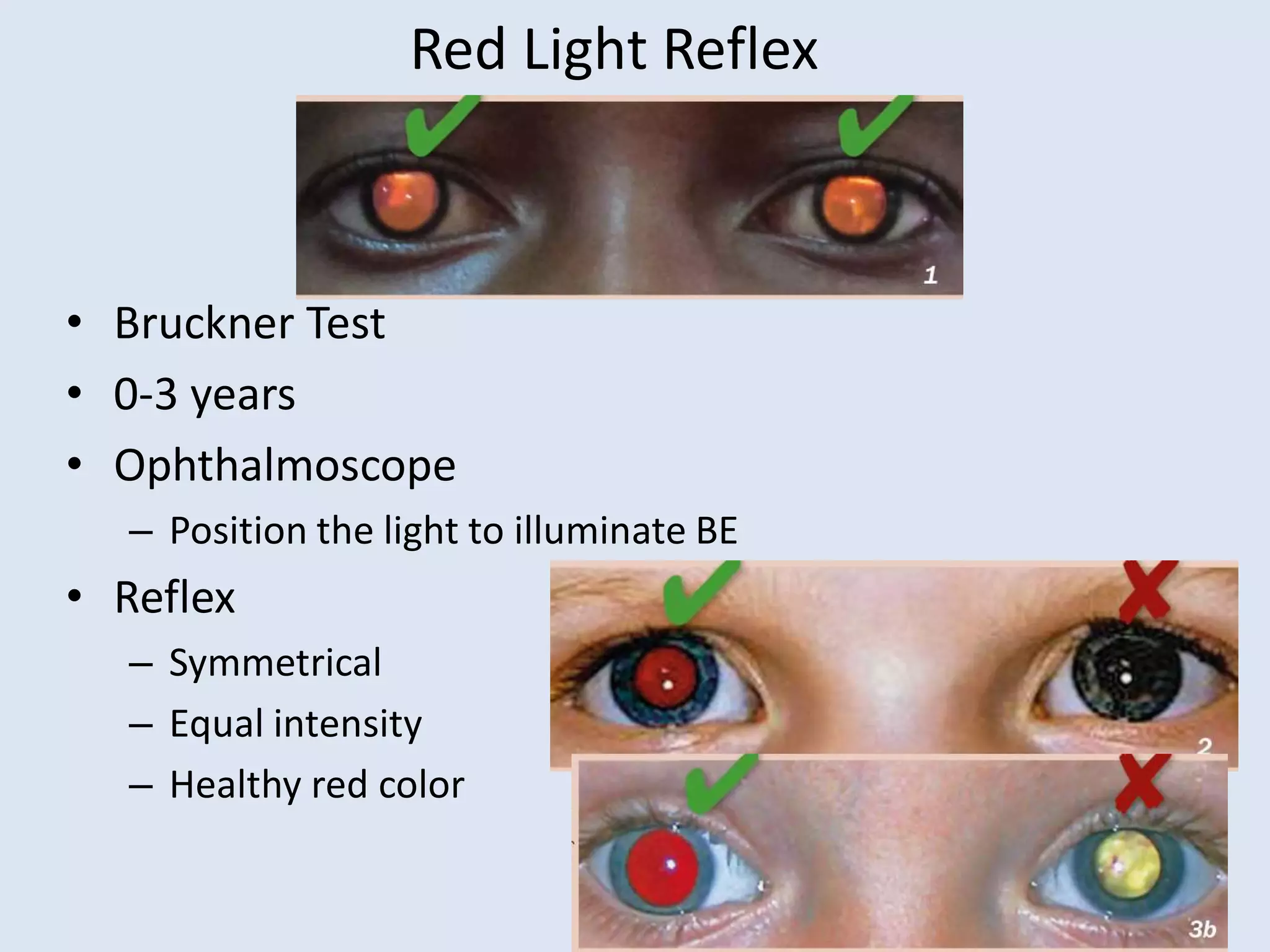
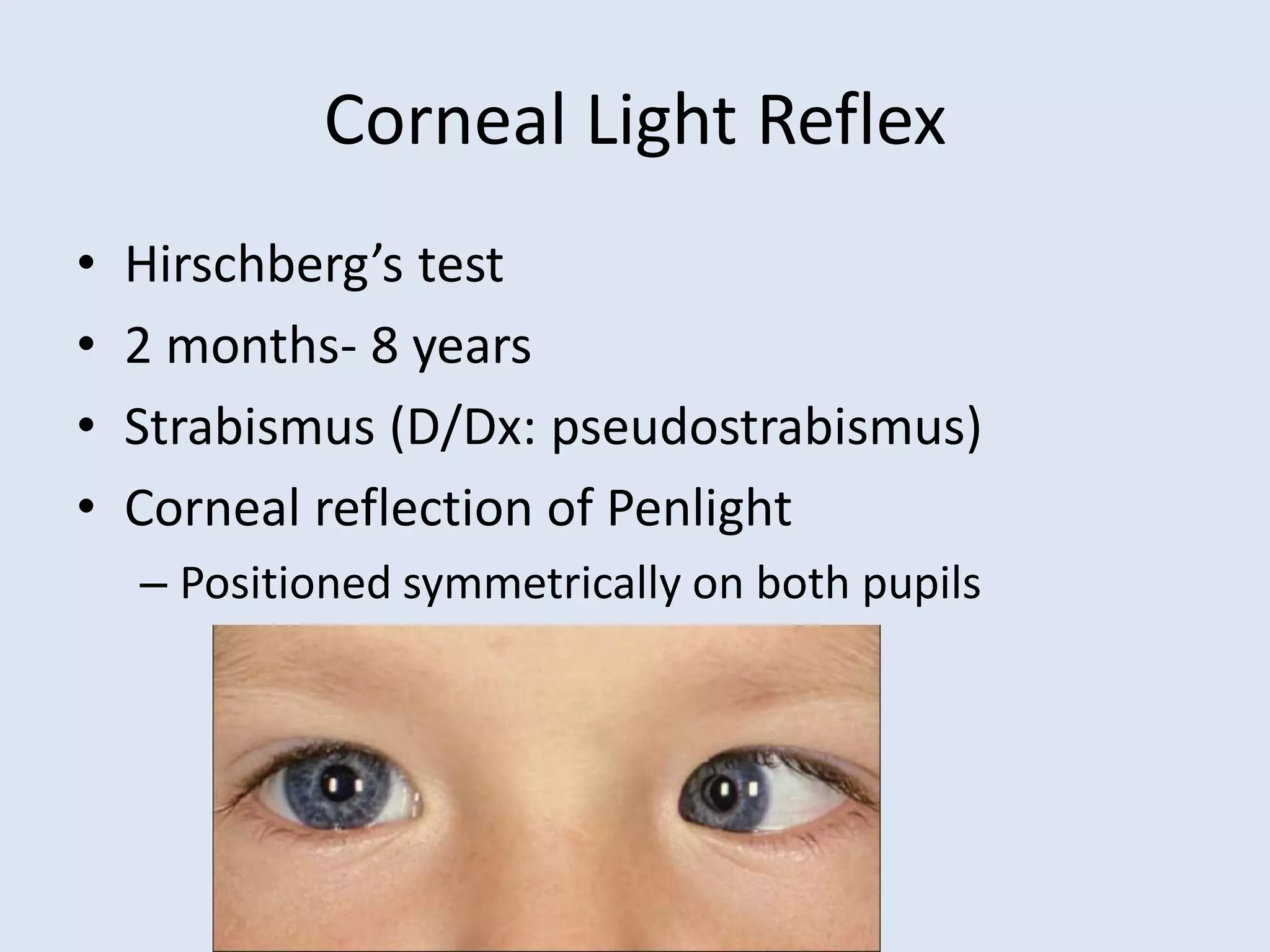
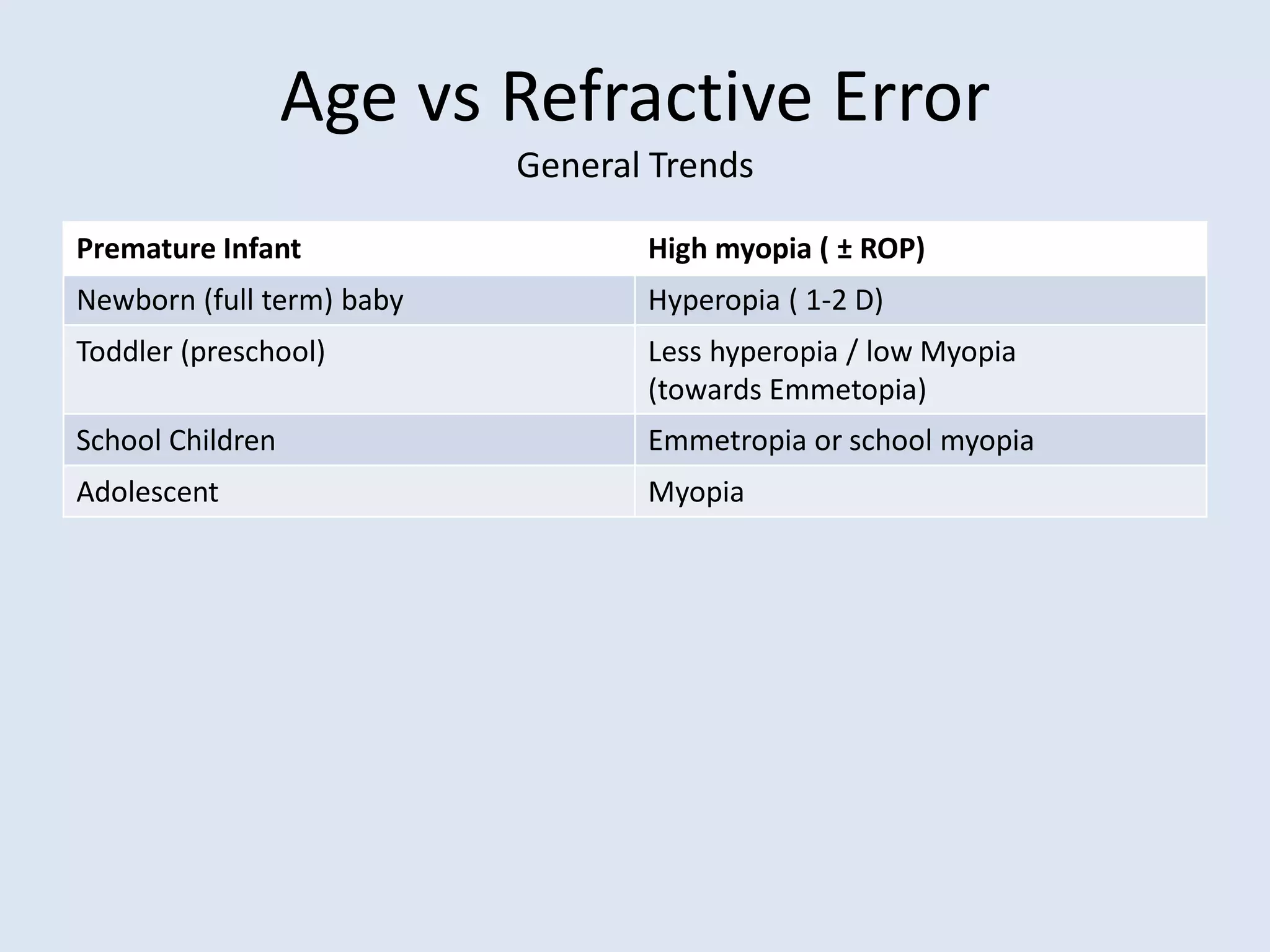
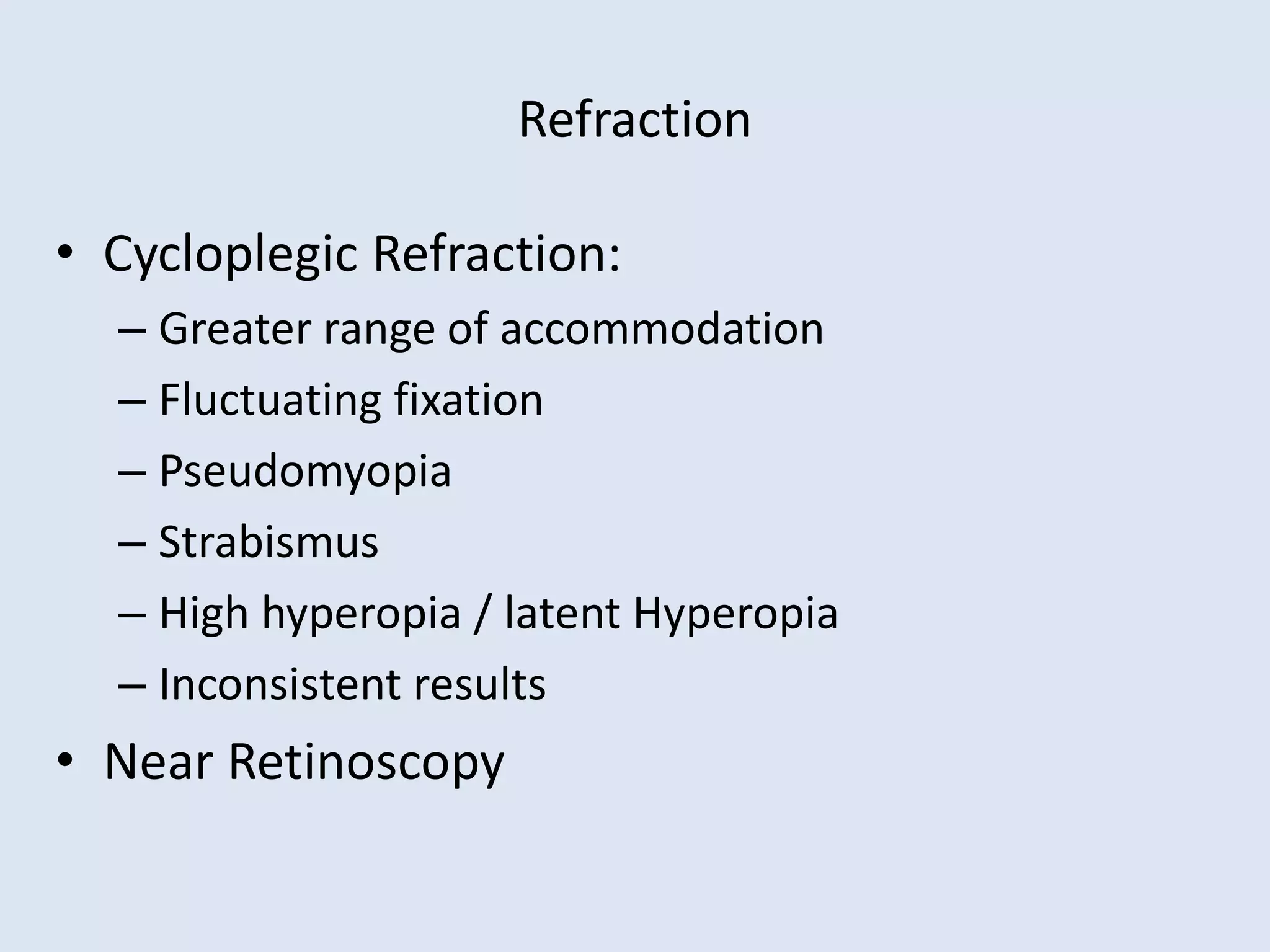
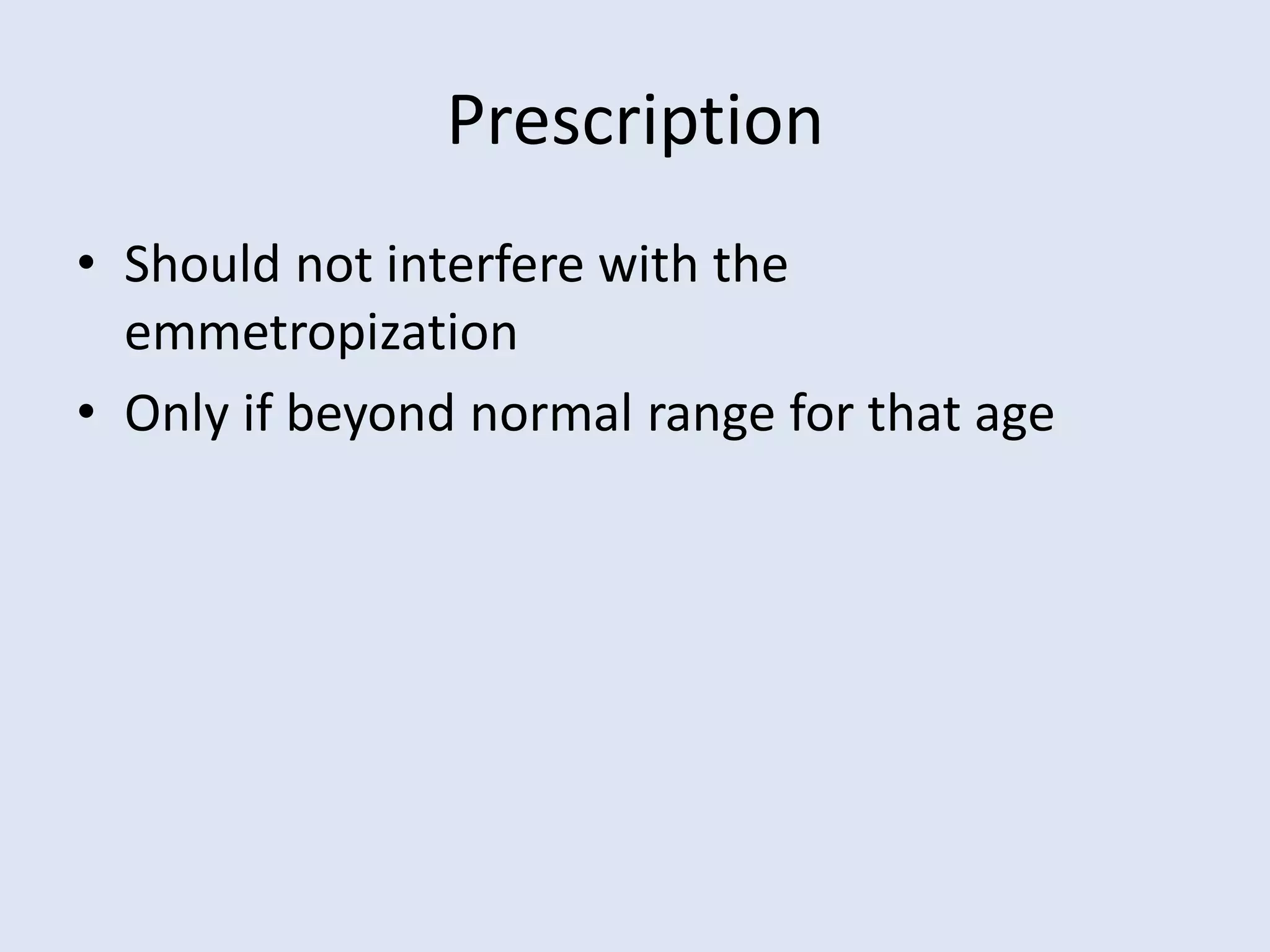
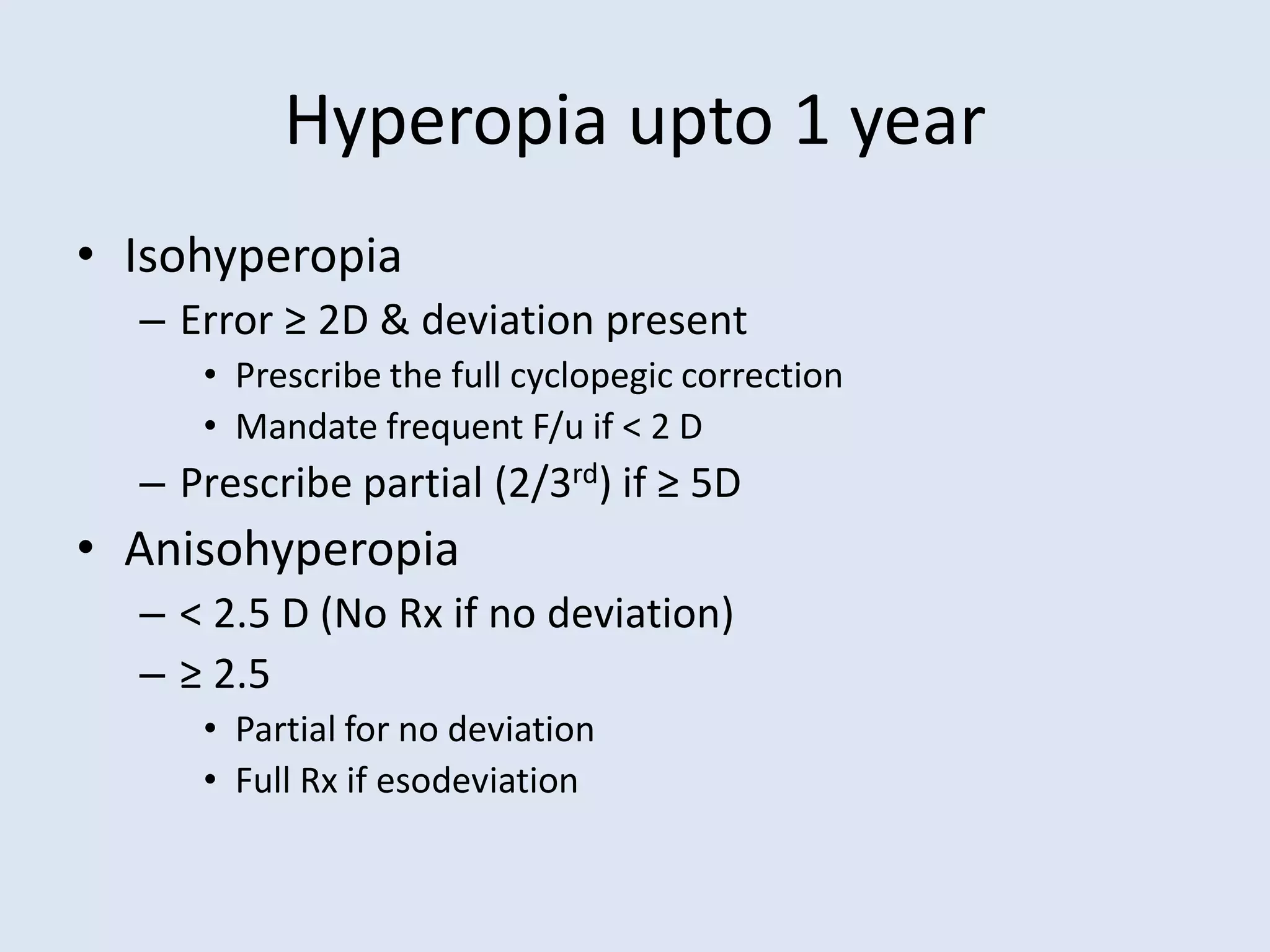
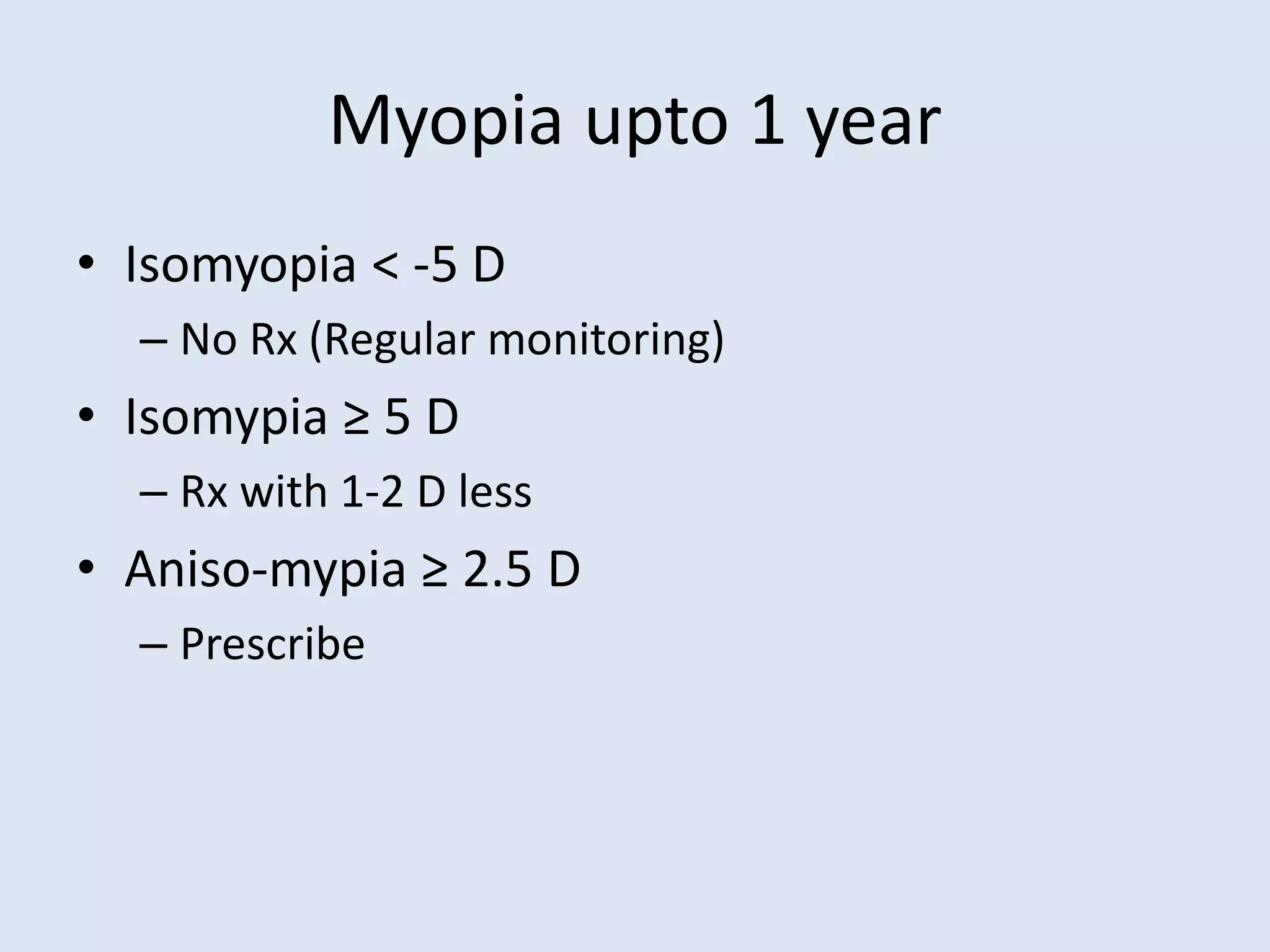
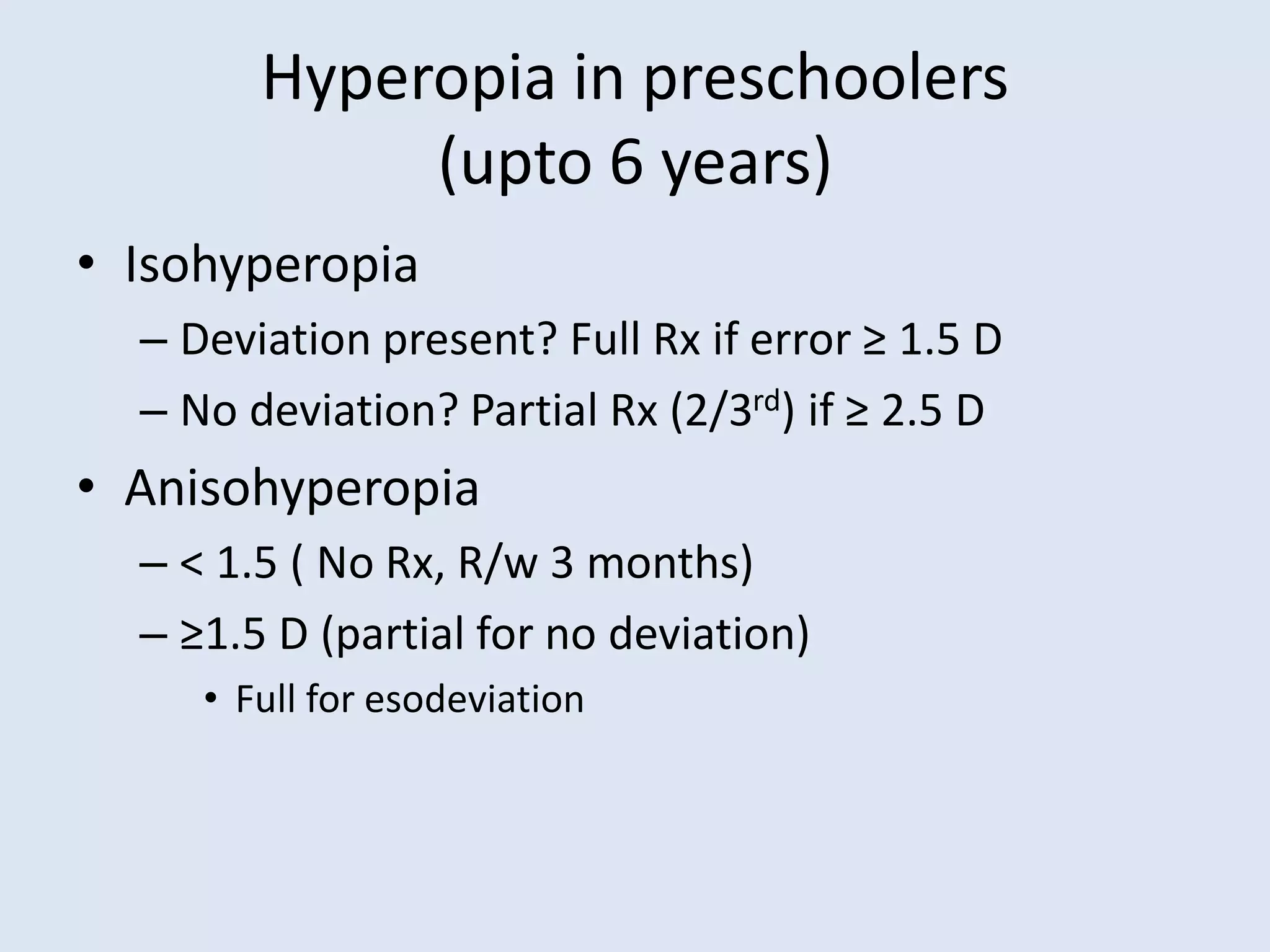
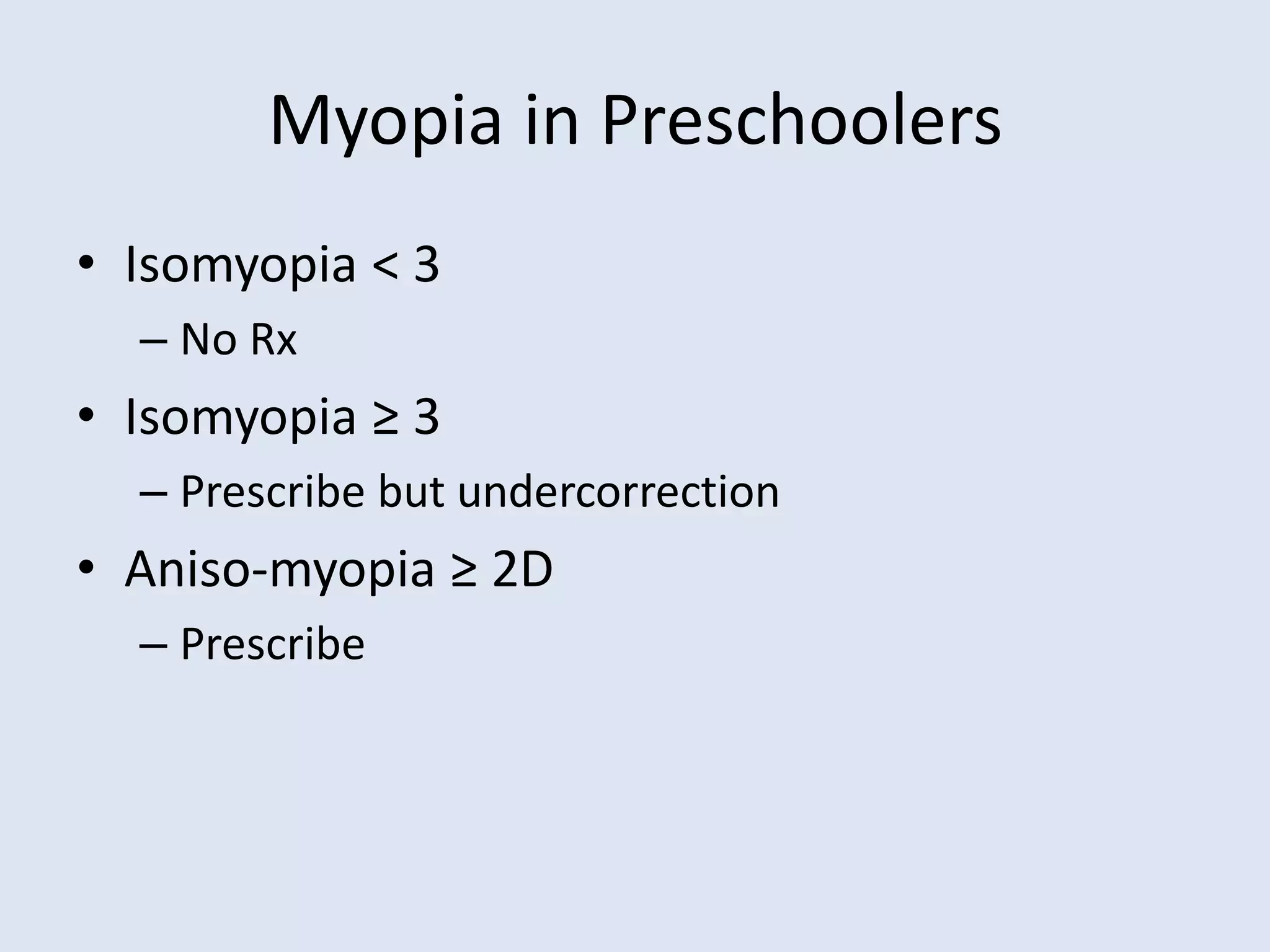
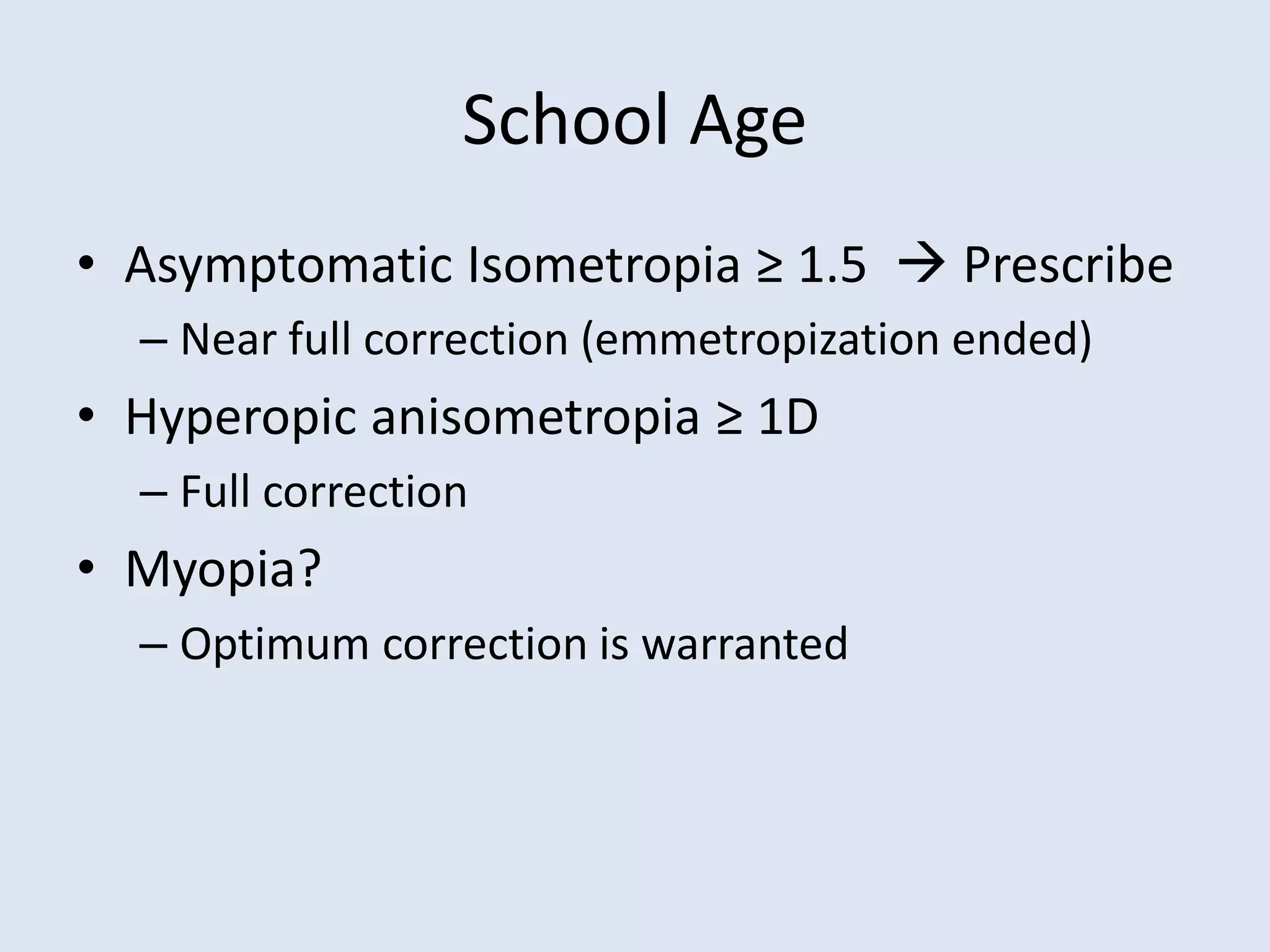
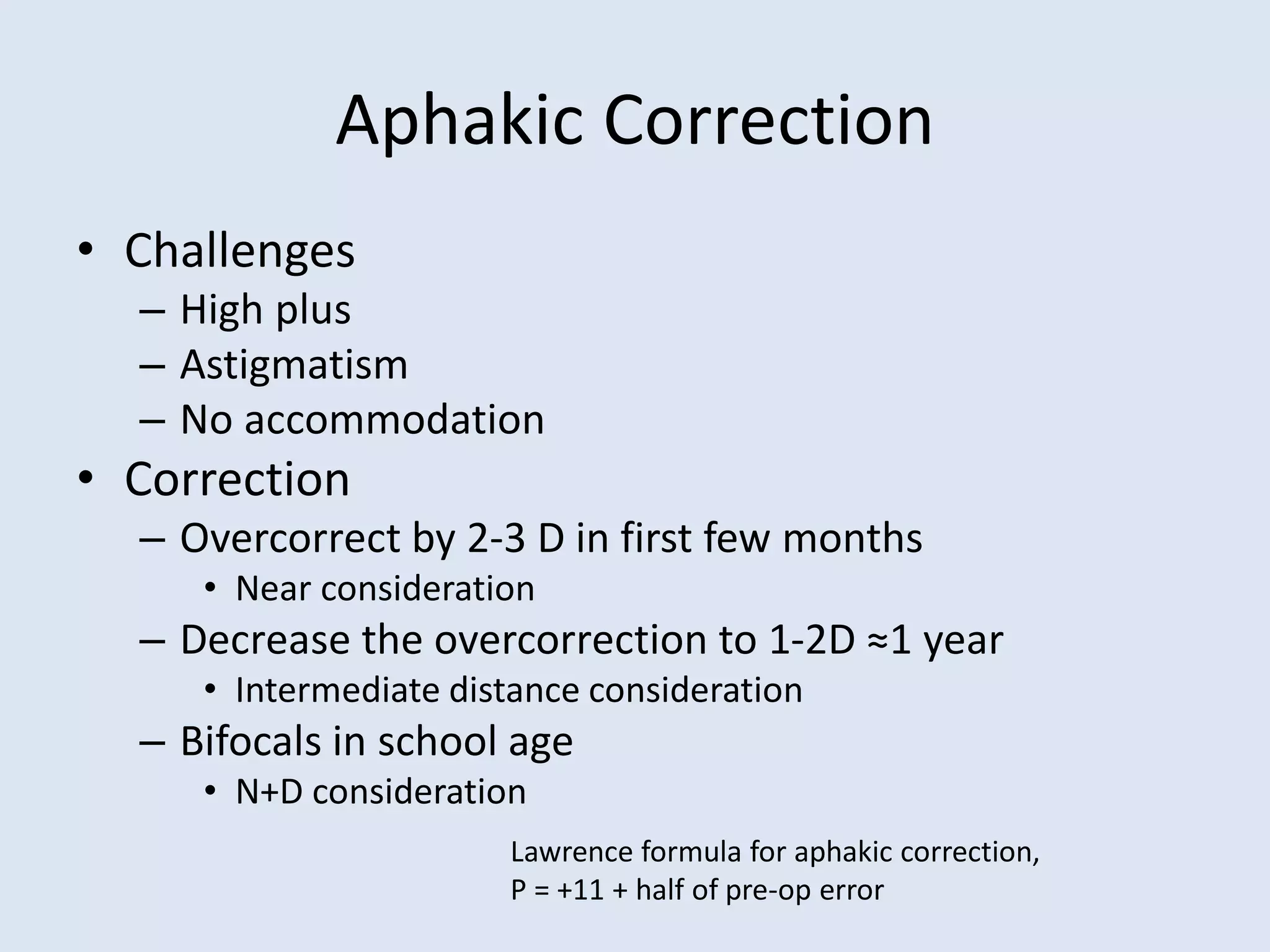
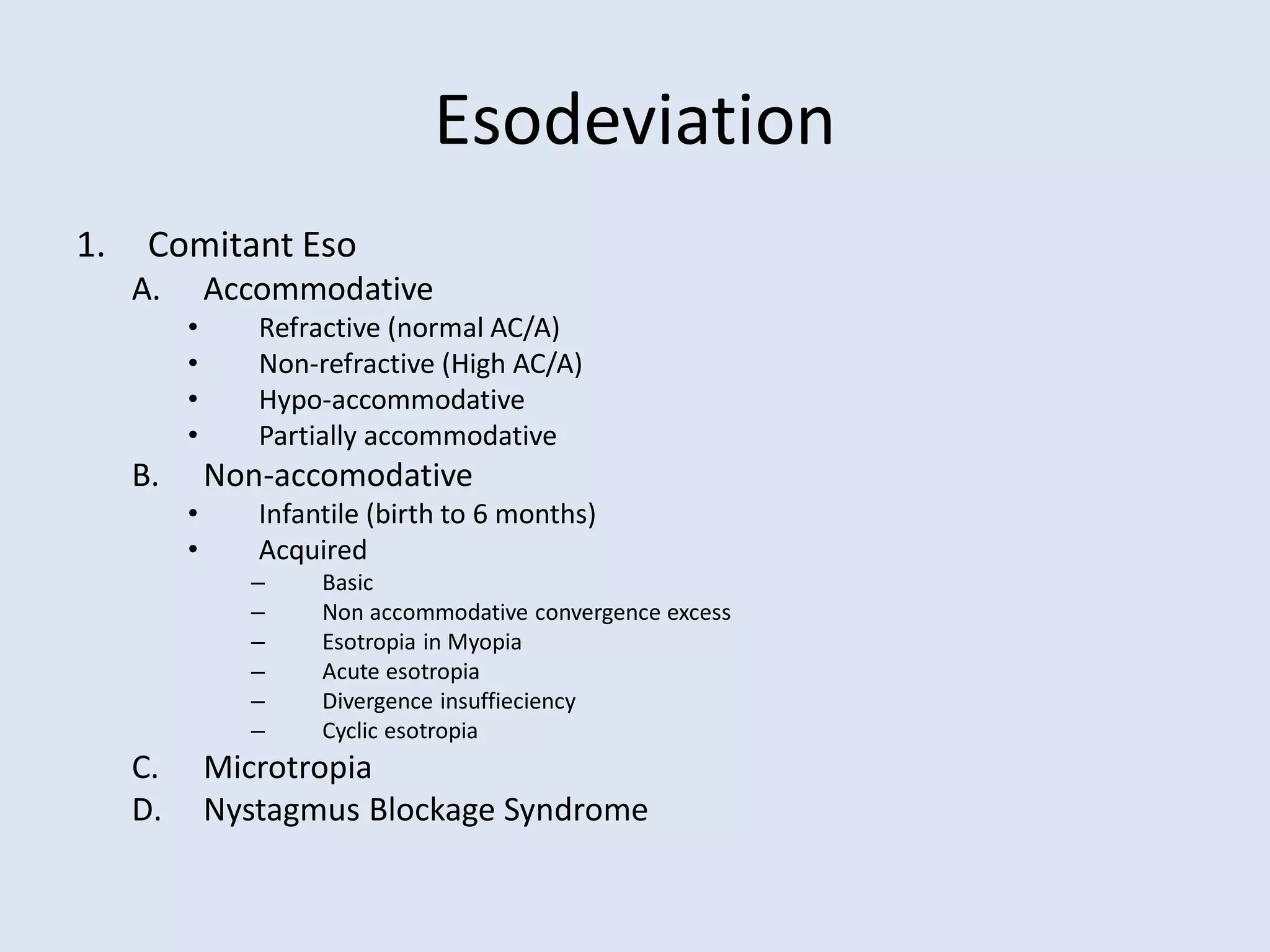
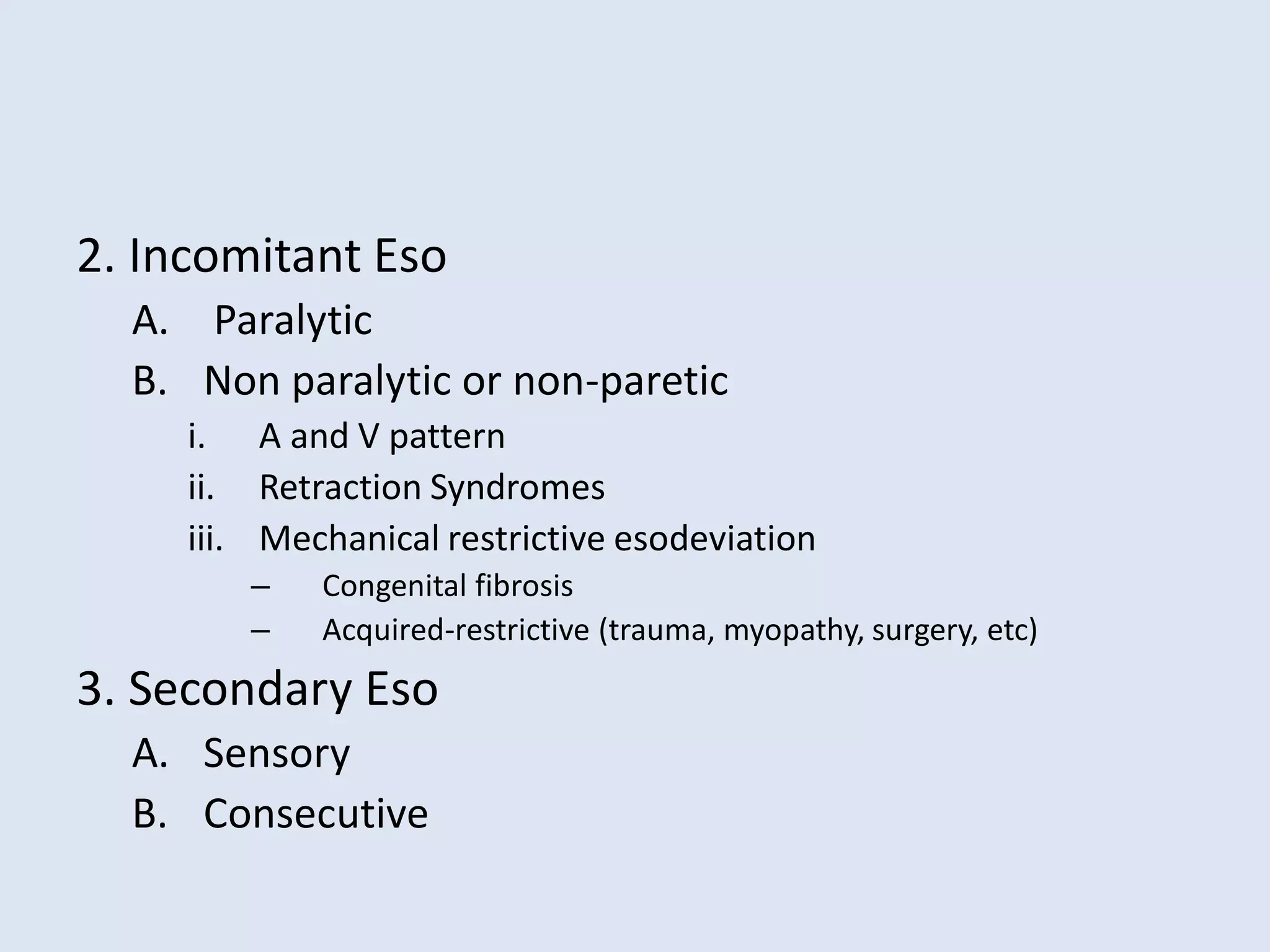
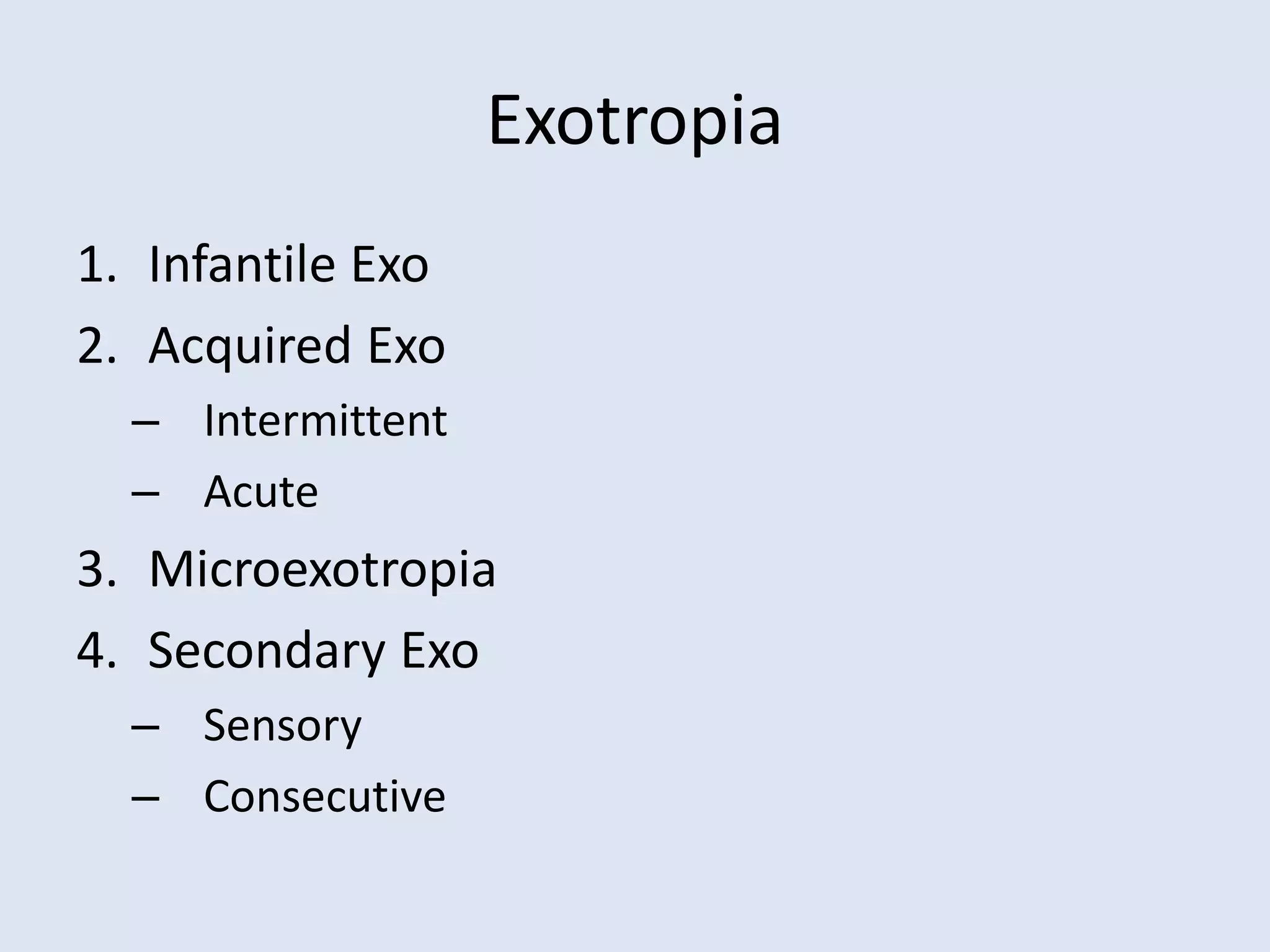
This document provides a comprehensive overview of vision assessment and screening in children, detailing various visual conditions such as refractive errors, amblyopia, strabismus, and nystagmus. It outlines age-specific visual milestones, assessment techniques, and corrective measures for different visual impairments. Additionally, it discusses the implications of these conditions on pediatric eye care and the importance of prompt diagnosis and treatment.