This document provides information on various anesthetic agents used in ophthalmic procedures, including general anesthetics (GA), regional anesthetics (RA), local anesthetics (LA), and topical anesthetics. It describes the types, mechanisms of action, common drugs, dosages, administration routes, indications, and side effects of different anesthetic classes. Key anesthetic agents discussed include nitrous oxide, halothane, ketamine, propofol, lidocaine, bupivacaine, and tetracaine.


![Common General Anesthetics [GAs]
• Nitrous Oxide
– Commonly called laughing gas with a formula N2O
– Colorless, non-inflammable, slightly sweet odor and
taste in room temperature
– Most used gaseous anesthetic in the world
– Other uses: food additive as propellant, fuel additive
for higher combustion, respiratory inhalant for
euphoric pleasures, refrigerant
– Due to its weaker anesthetic and muscle relaxant
properties, it is always supplemented with other
agents to increase the potency](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-5-2048.jpg)
![• Indication of Nitrous Oxide
– Surgical anesthesia, analgesia, pain
• Renal excretion accounts for >70%
• Side effects:
– Nausea, vomitting
– Paresthesia, lack of concentration
– Peripheral neuropathy, atonia
– Hypoxia [in overdose]](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-7-2048.jpg)




![RA
• Analgesic effect in specific body parts, eg. Legs,
hands [where procedures are targeted] like
epidural anesthesia
– Reduced risks comparative to GA
– Applicable for resource limited set up
– Pt consciousness retained greater cooperation
• Drug:
– Percutaneous lidocaine
– Bupivacaine
– Livobupivacaine
– Ropivacaine](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-16-2048.jpg)
![LA
• Local anesthetics are a group of structurally
related compounds which share as principal
mechanism of action the blockade of voltage-
gated sodium channel, resulting in reversible
interruption of nerve signal transduction.
– Used both topically or as injection form
• When used with epinephrine [adrenaline] LA has
– prolonged duration of action
– Reduced systemic absorption
[epinephrine has vasoconstriction effect on alpha
receptors of blood vessels]](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-17-2048.jpg)
![Chemical structure
• All local anesthetic [except cocaine] contains 3
basic structural components:
Aromatic
Ring
• Usually
substituted
Connecting
Group
• Ester
[novocaine]
• Or, amide
[lidocaine]
Ionizable
amino
Group](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-18-2048.jpg)



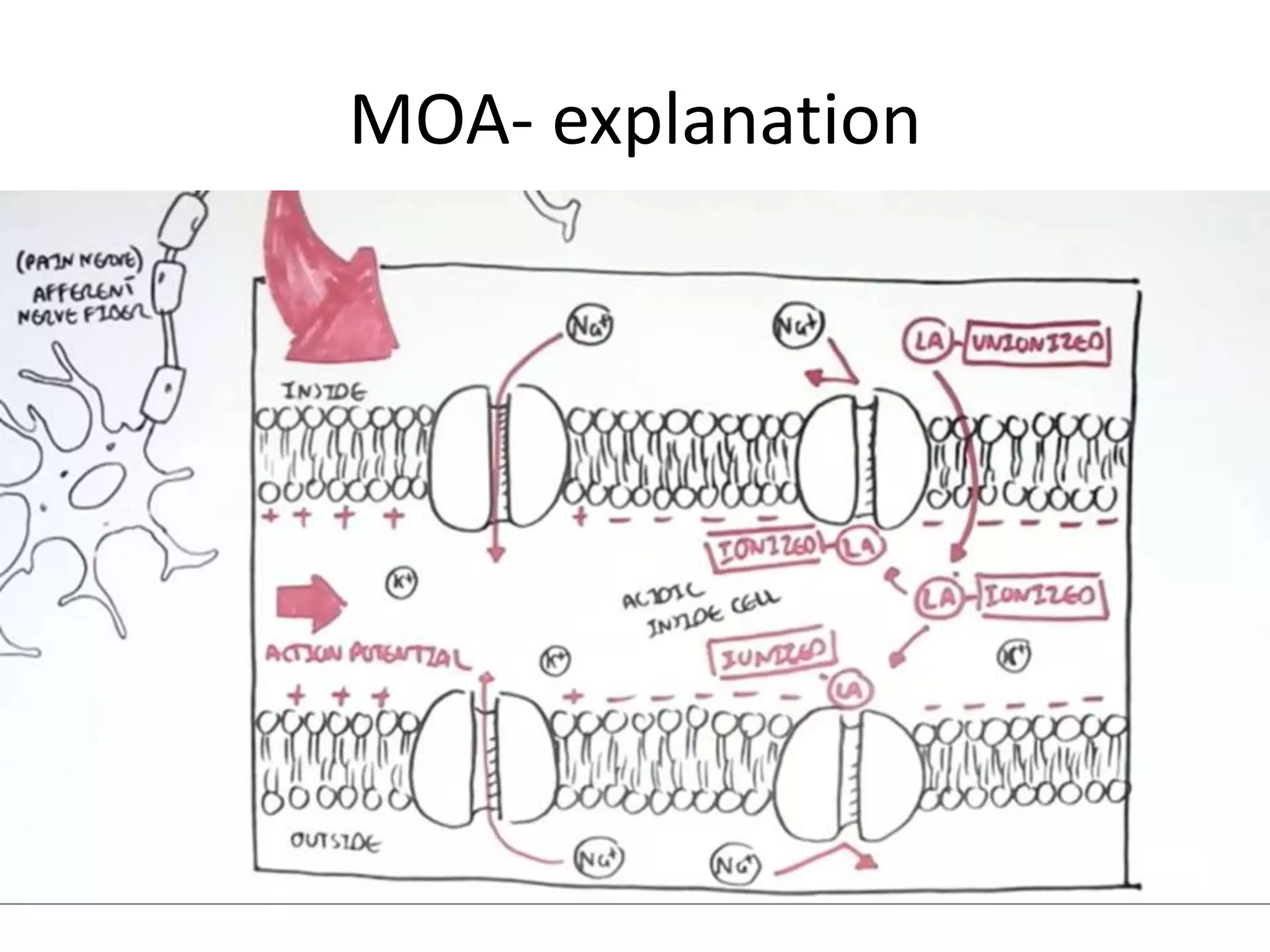


![• Next to sodium channel blockade LA also act upon
– Calcium and potassium channels
– G protein coupled receptors this gives the anti-
inflammatory effect
• Different additives may be used with LA for better
and prolonged effect:
– Buprenorphine [↑ed nausea and vomitting]
– Dexmeditomidine & Clonidine [dose dependent
systemic side effect eg. Bradycardia, hypotension]
– Dexamethasone [least systemic side effect and longest
nerve block duration]](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-25-2048.jpg)

![Common Ophthalmic anesthetics
• Lidocaine
• Proparacaine
• Tetracaine
• Proxymetacaine
[all in hydrochloride form]](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-28-2048.jpg)
![Lidocaine
• Belongs to amide class
– Trade name Xylocaine
• Most popular local anesthetic agent
• First modern local anesthetic [since 1940]
• Injected through the skin directly to the
targeted body parts to be numbed
• Contraindications in:
– Cardiac arrythmias [heart block]
– Liver, kidney and coronary artery diseases](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-29-2048.jpg)

![• Drug interactions: simultaneous use with the
following drugs causes drug interactions. So,
extreme cautions is required:
– Antidepressants [triptyline, imipramine]
– Antipsychotics [phenothiazines, butyrophenones]
– lidocaine has additive effect on CNS depression with
sedatives
– When used in a pt who is using propanolol [beta
blocker], the anesthetic effect of lidocaine is severely
reduced to 47%, 7& co-administered use reduced its
effect to 30%](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-31-2048.jpg)
![Dosage of Lidocaine
• Retrobulbar block: 2%
– Each dose consists of 4 ml [80mg]
– Anesthesia onsets after 3-5 min
– Duration without epinephrine: 1.5 to 2 min
• Peribulbar: 1%
– Each dose 10-15 ml [100-150mg]
– Anesthesia onsets after 3-5 min
– Duration without epinephrine: 1.5 to 2 min](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-32-2048.jpg)
![Retrobulbar Block
• Surgery involving cornea, AC, lens regional
anesthetic block
• Local anesthetic is introduced into the muscle
cone. So, it blocks:
– Ciliary nerves
– Ciliary ganglions
– Cranial nerves III, IV and VI
• Does not anesthetize CN VII [7th Nerve]
– Pt is able to close the eye with orbicularis oculi
– But not open with LPS](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-33-2048.jpg)
![Peribulbar Block
• Local anesthetic introduced into the
orbicularis oculi muscle
• Blocks
– Ciliary nerves
– CN III and VI
– Does not affect optic nerve [CN II]
• Lower complication rate than retrubulbar but
difficult to get complete dense block](https://image.slidesharecdn.com/anestheticagents-190725152732/75/Anesthetic-agents-General-and-Local-34-2048.jpg)