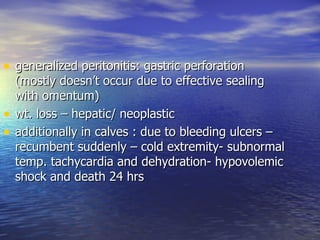
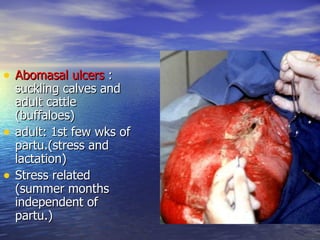
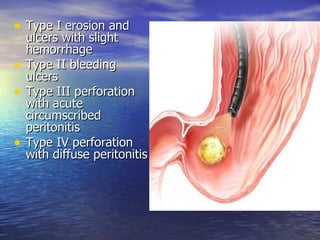
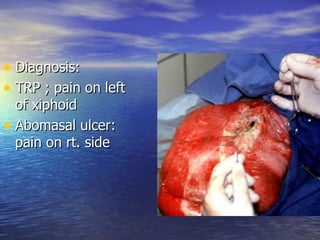
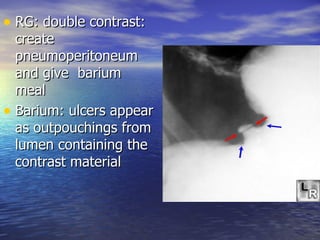
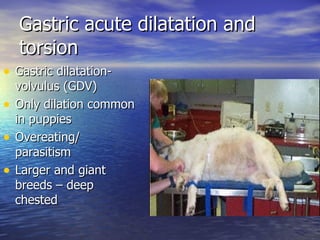
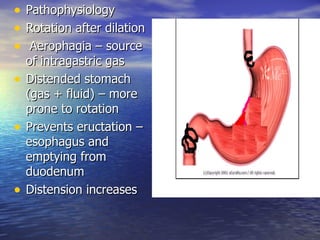
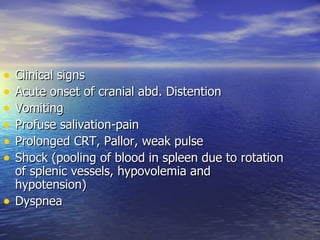
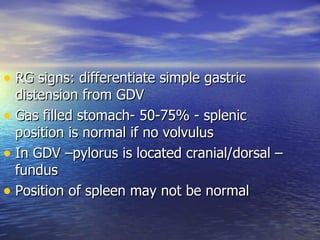
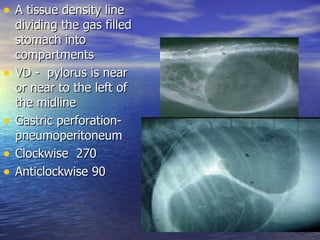
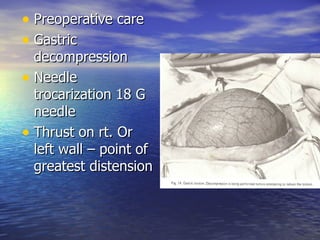
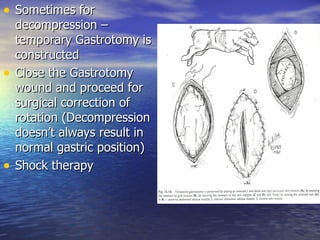
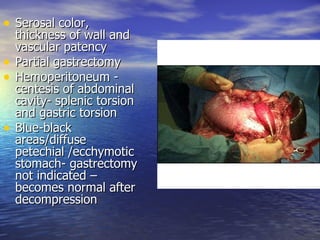
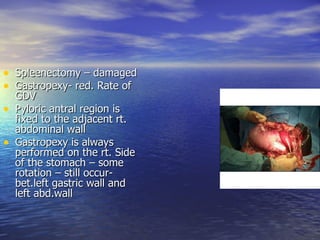
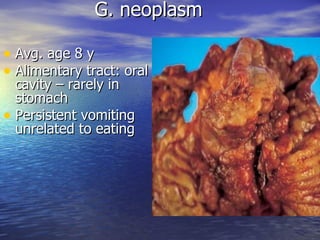
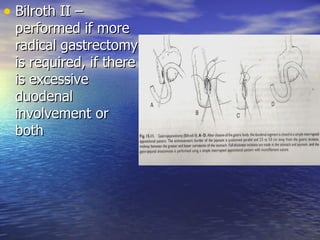
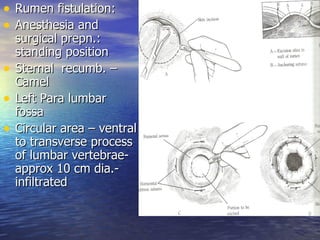
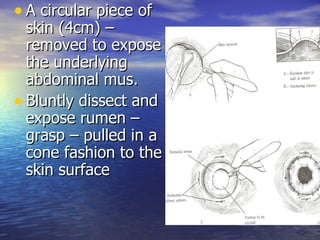
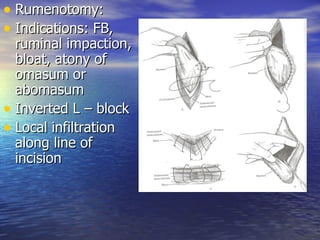
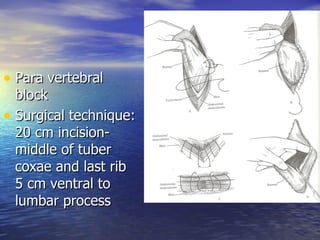
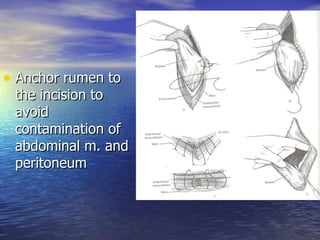
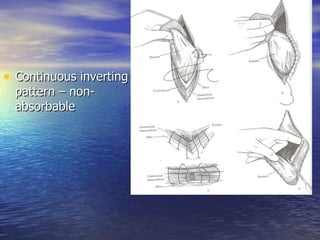
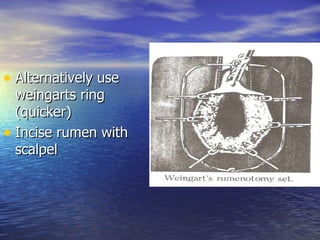
The document presents a comprehensive overview of veterinary gastrointestinal surgery focusing on conditions such as gastric ulcers, abomasal ulcers, and gastric dilatation-volvulus (GDV) in animals. It details the causes, pathophysiology, diagnosis, and surgical treatment approaches, emphasizing the complexity of gastrointestinal diseases in both calves and adult cattle. Additionally, it discusses interventions like rumenotomy and gastropexy, highlighting the surgical techniques and post-operative care required for effective management of these conditions.