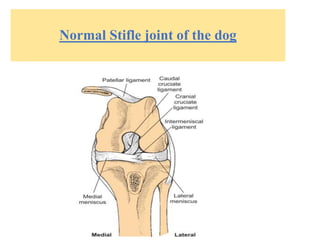
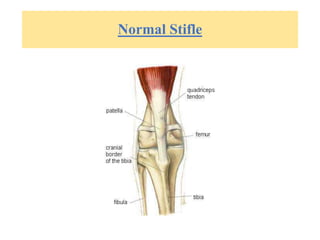
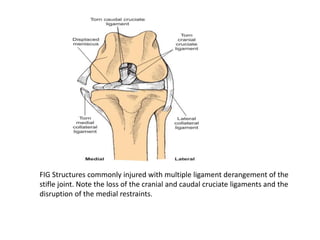
The document provides information on ligament injuries, specifically cranial cruciate ligament rupture in dogs. It discusses the pathophysiology, diagnosis, and treatment of cranial cruciate ligament rupture. Key points include:
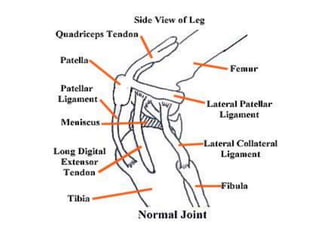
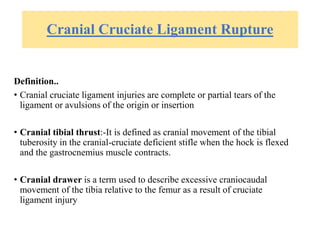
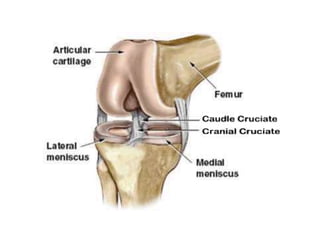
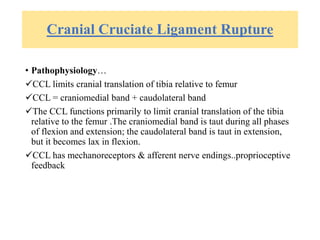
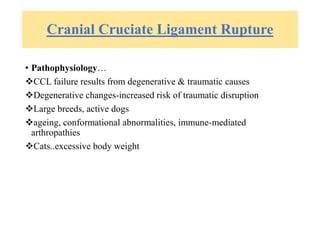
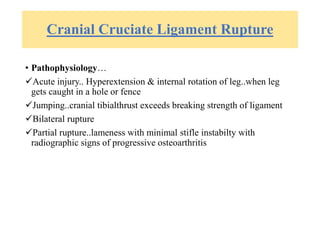
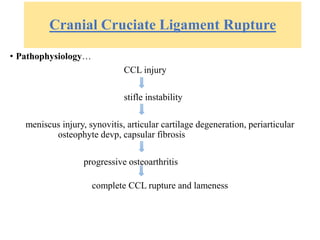
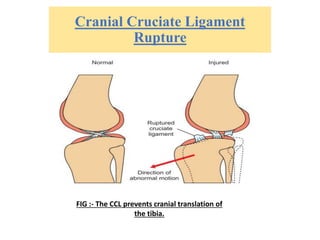
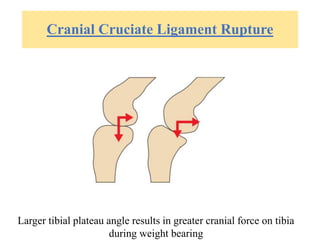
- The cranial cruciate ligament limits cranial translation of the tibia and controls internal rotation of the tibia. Rupture can be caused by traumatic injury or degeneration.
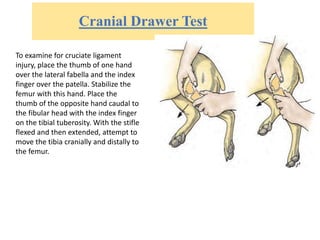
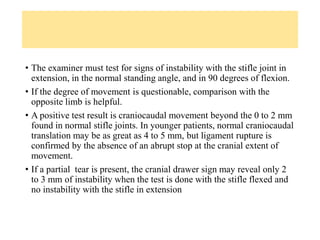
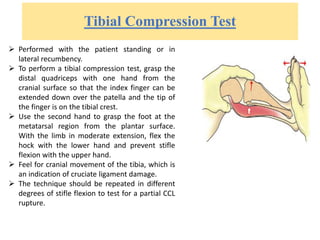
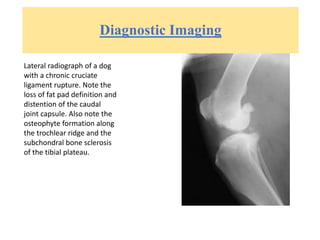
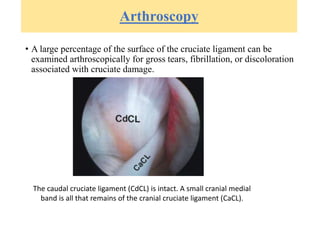
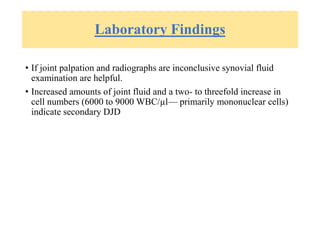
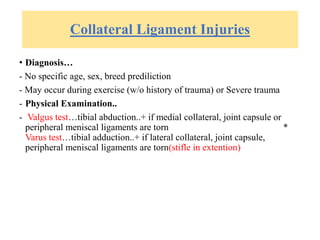
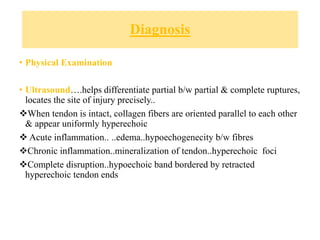
- Diagnosis involves physical exam tests like the cranial drawer test and tibial compression test, as well as diagnostic imaging like radiography and arthroscopy.
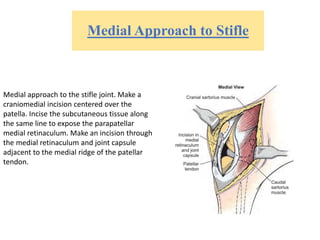
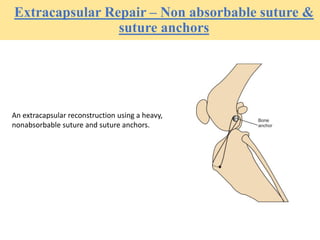
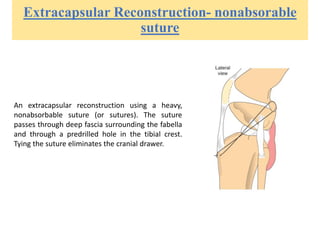
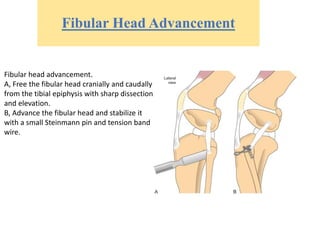
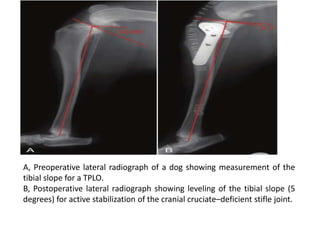
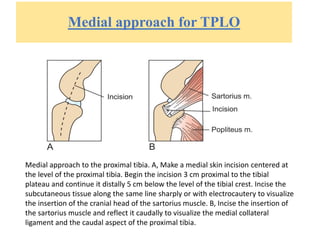
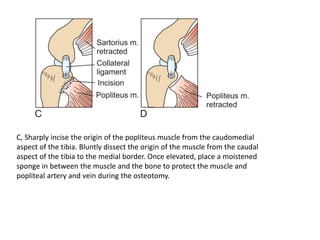
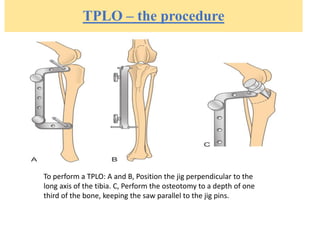
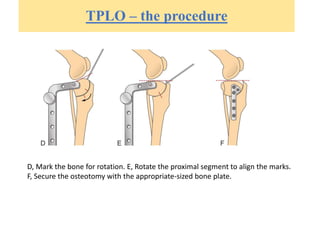
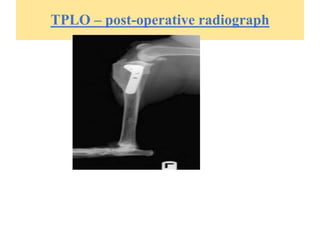
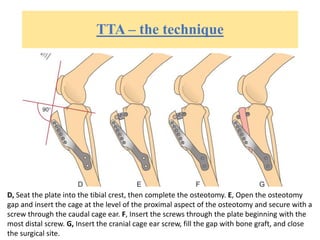
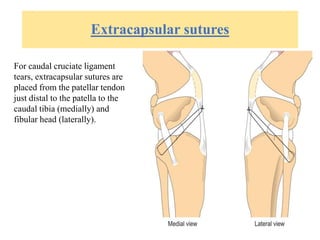
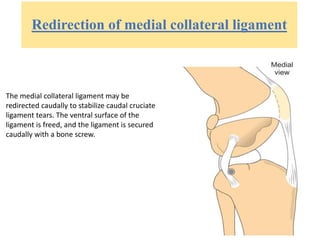
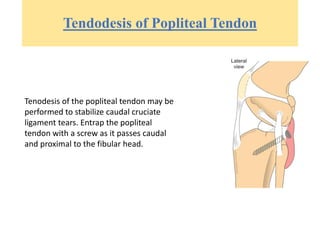
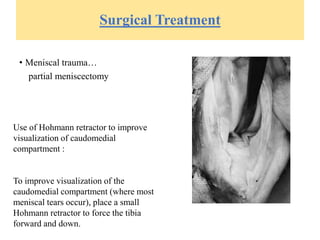
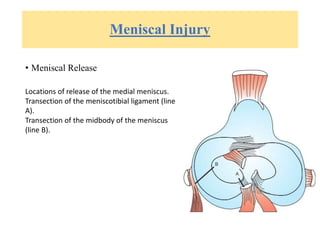
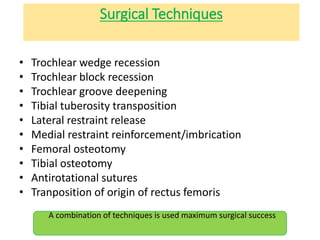
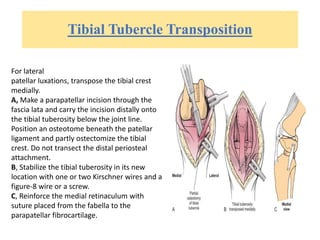
- Surgical treatment options aim to stabilize the stifle joint and include intracapsular reconstruction, extracapsular reconstruction, imbr