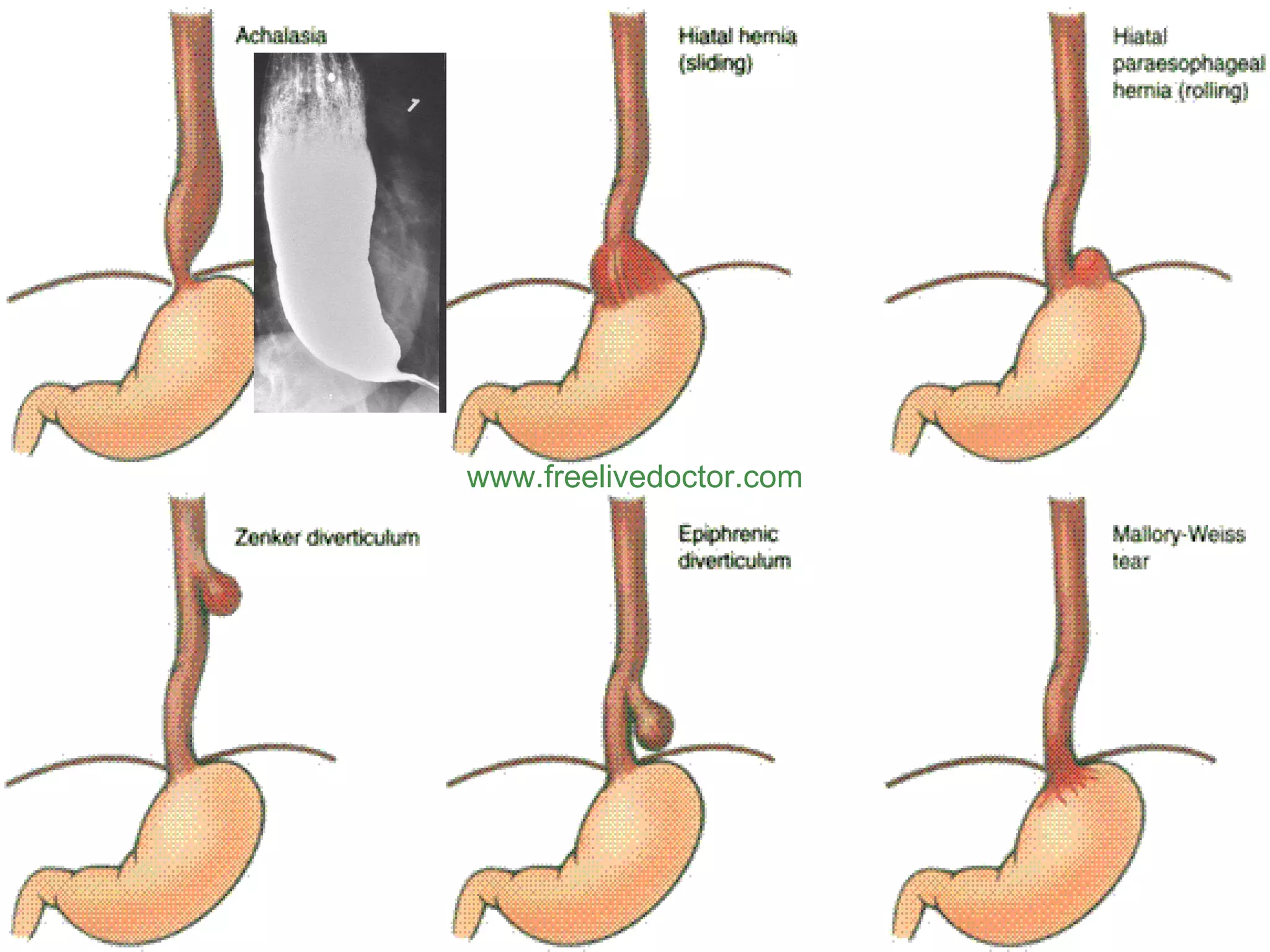
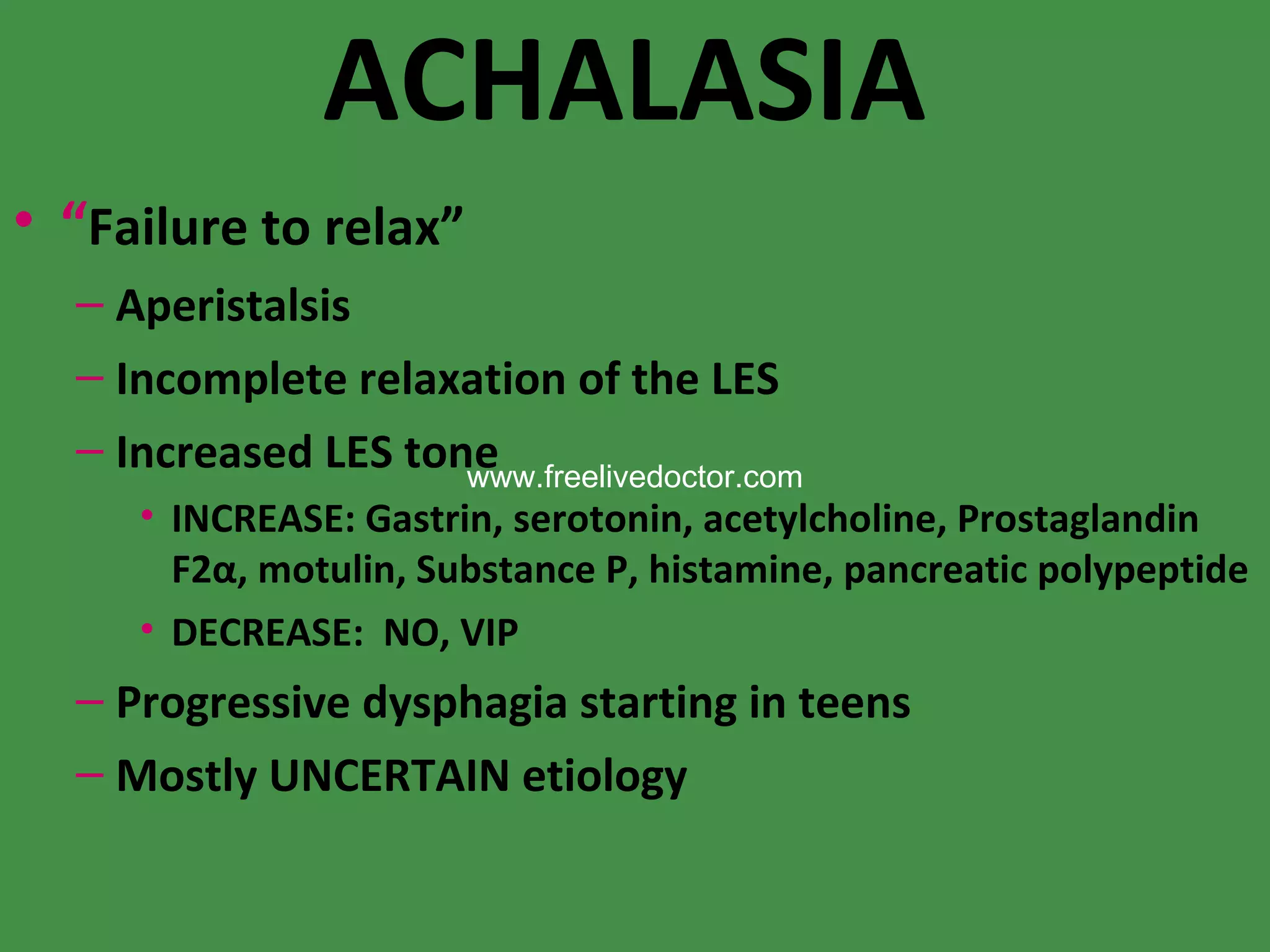
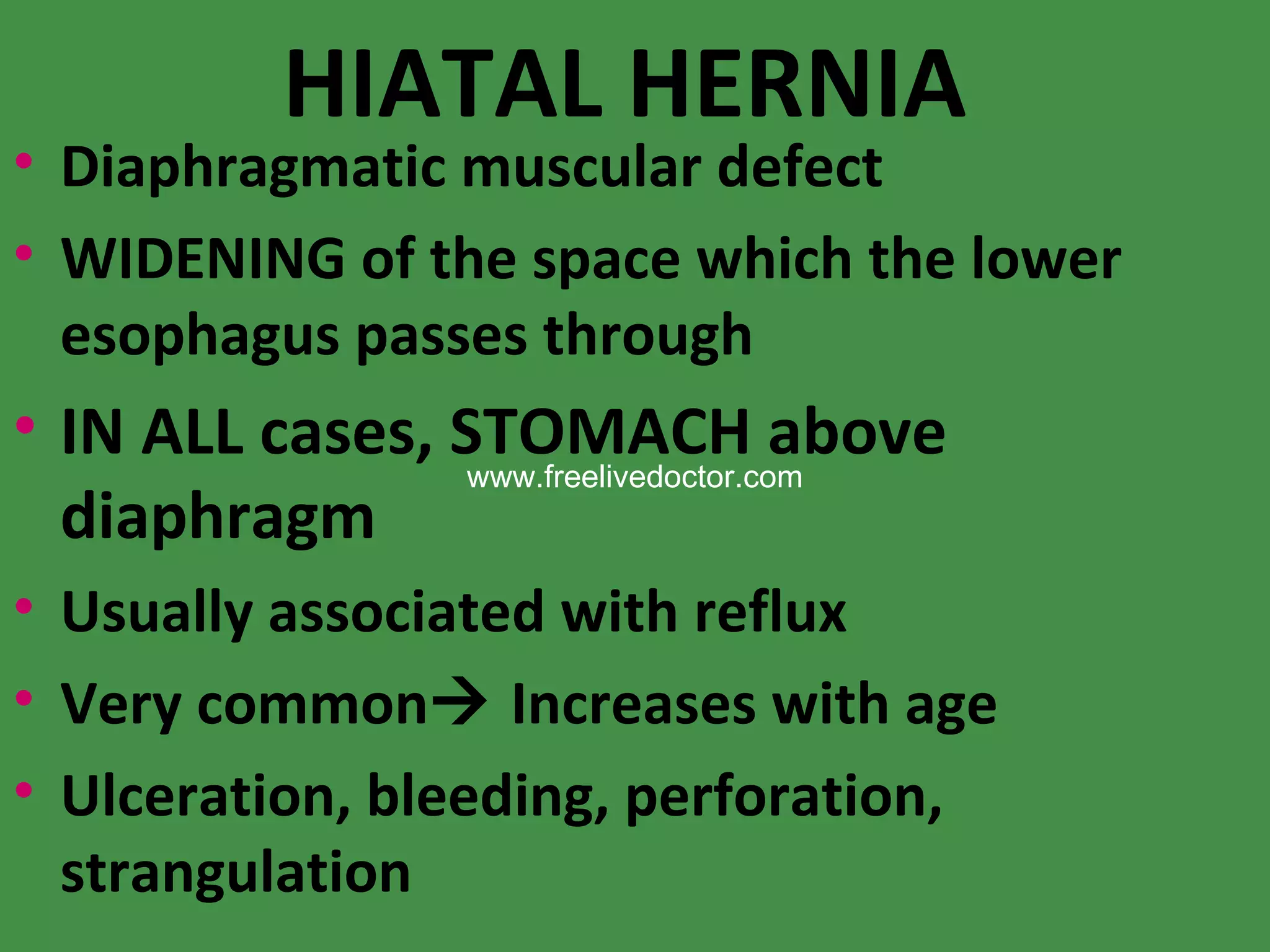
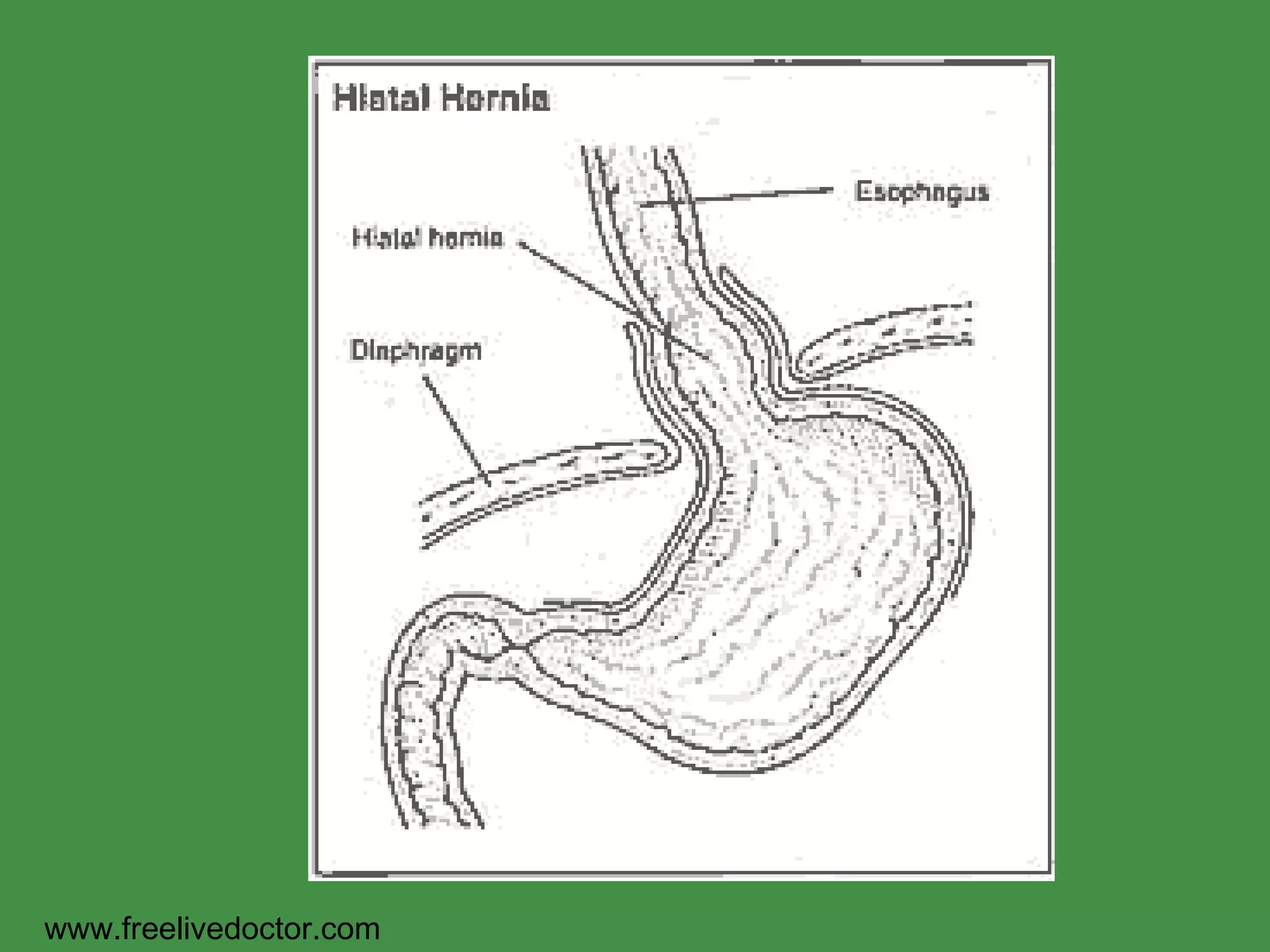
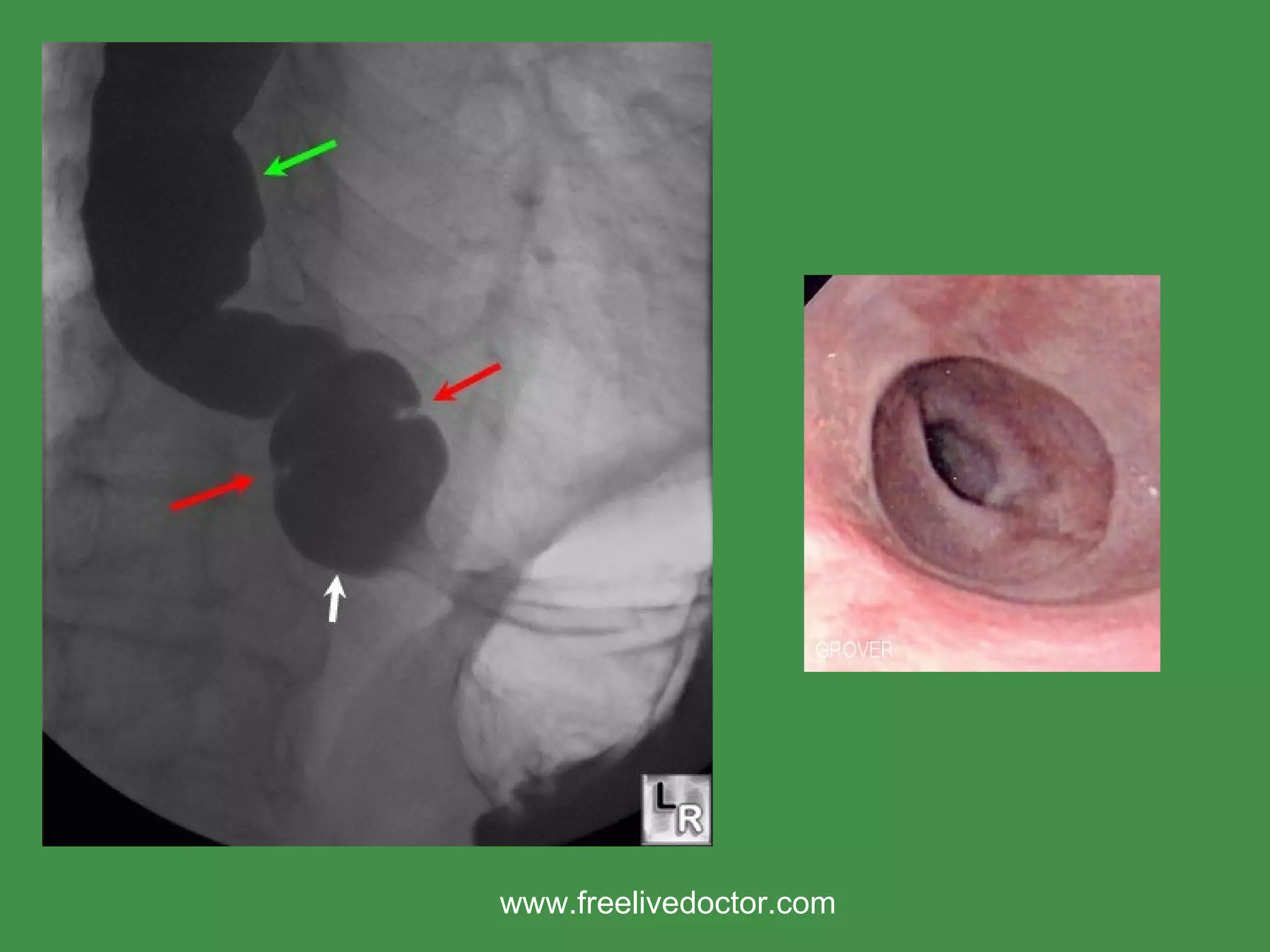
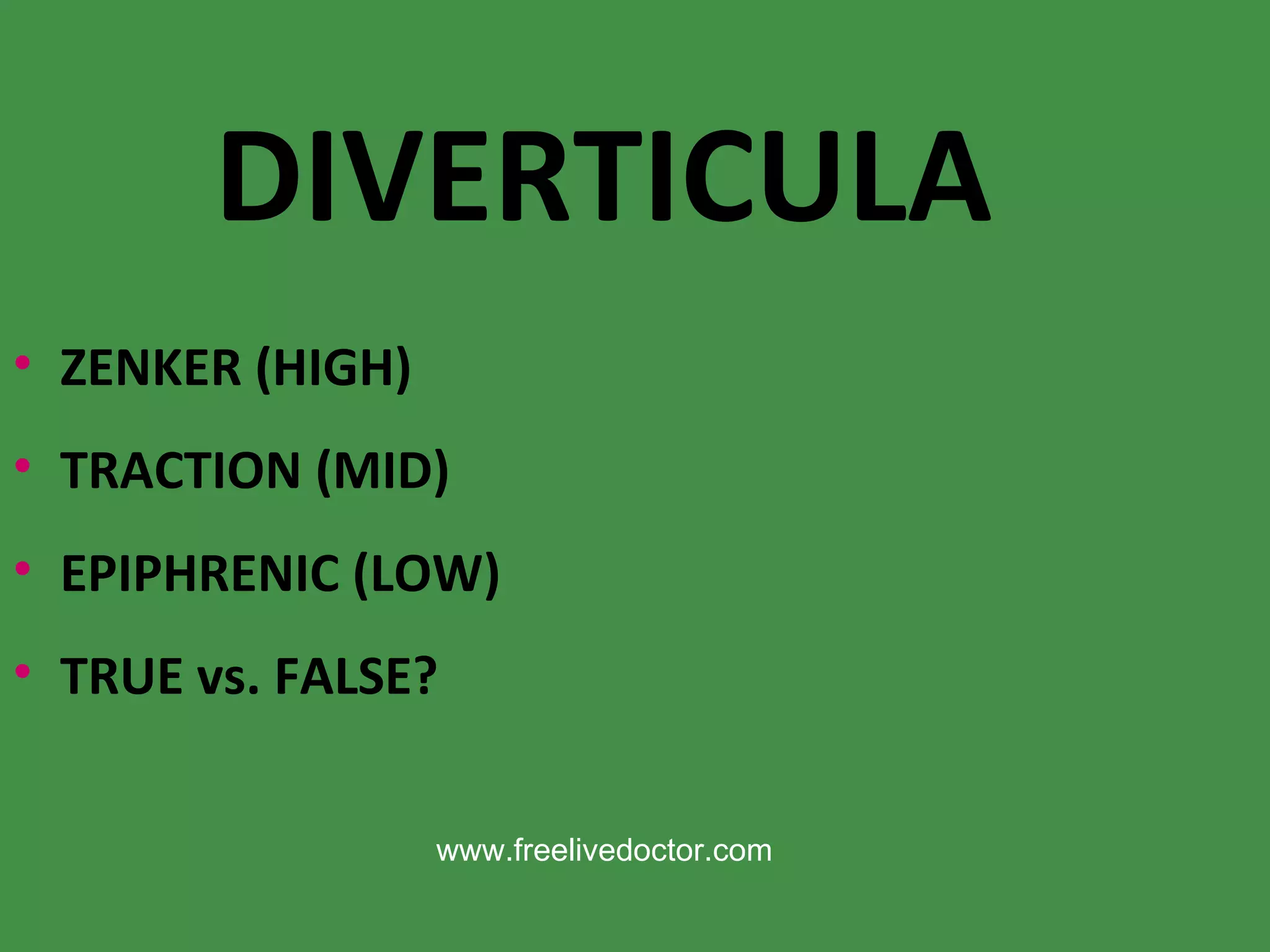
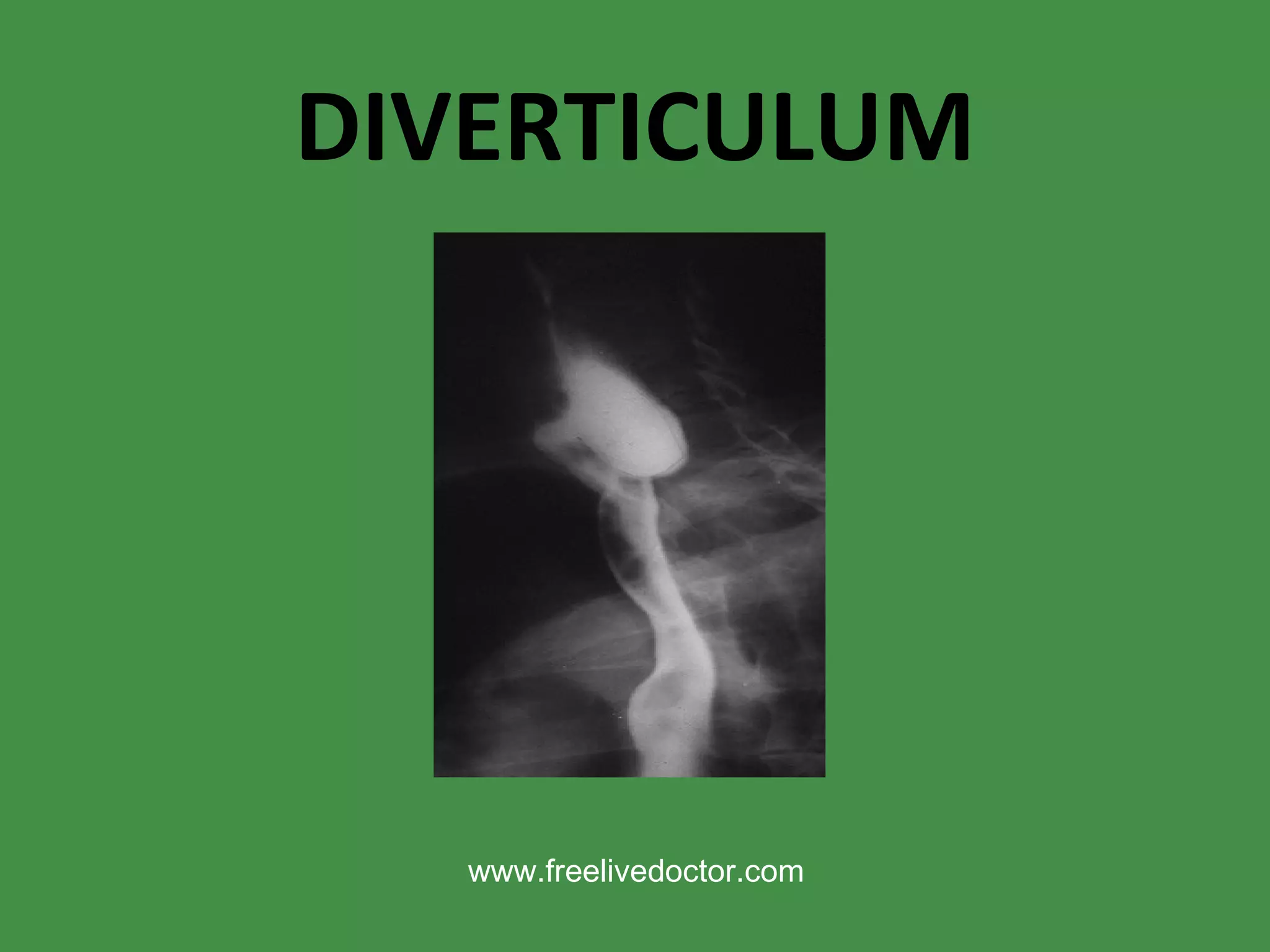
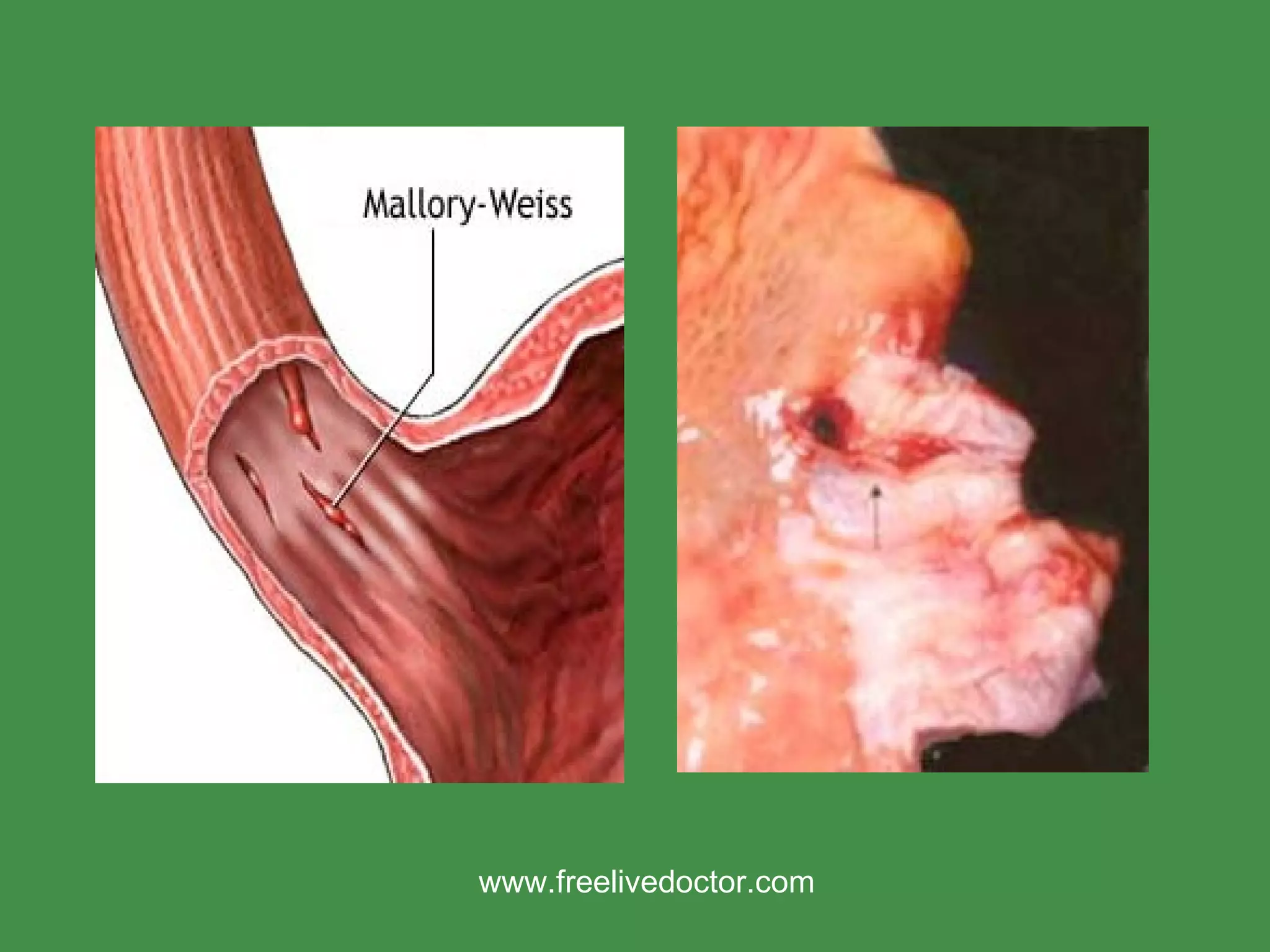
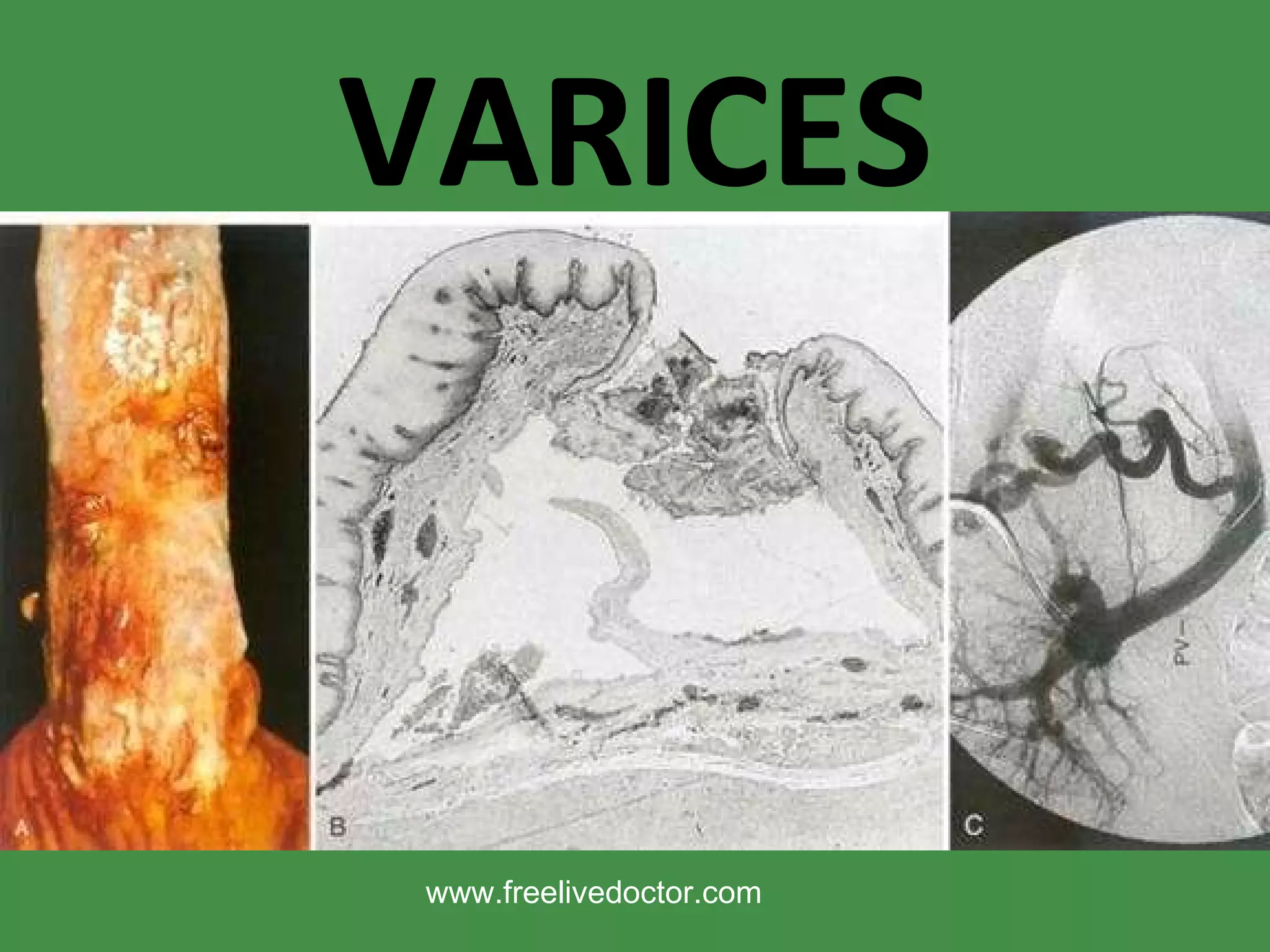
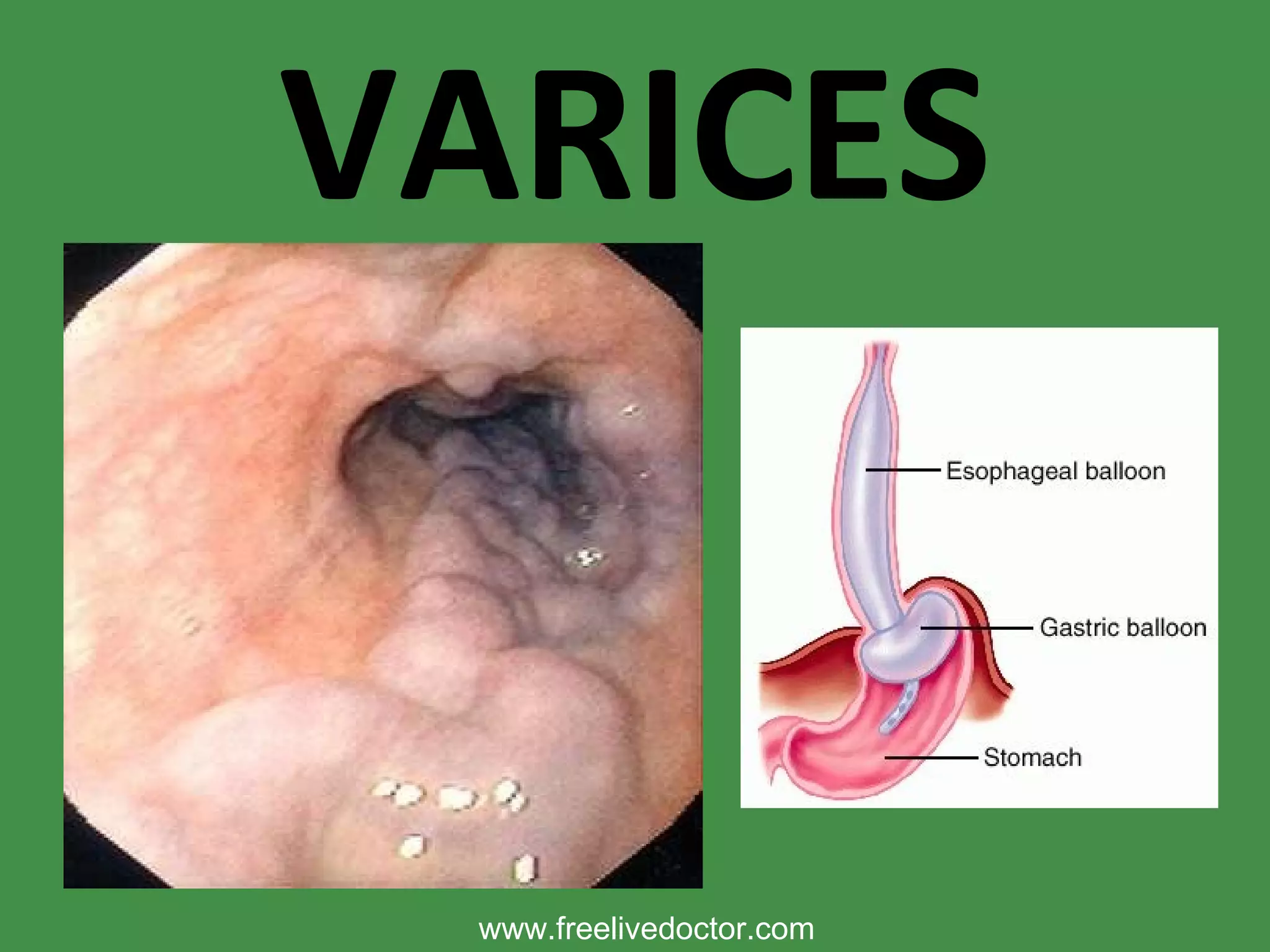
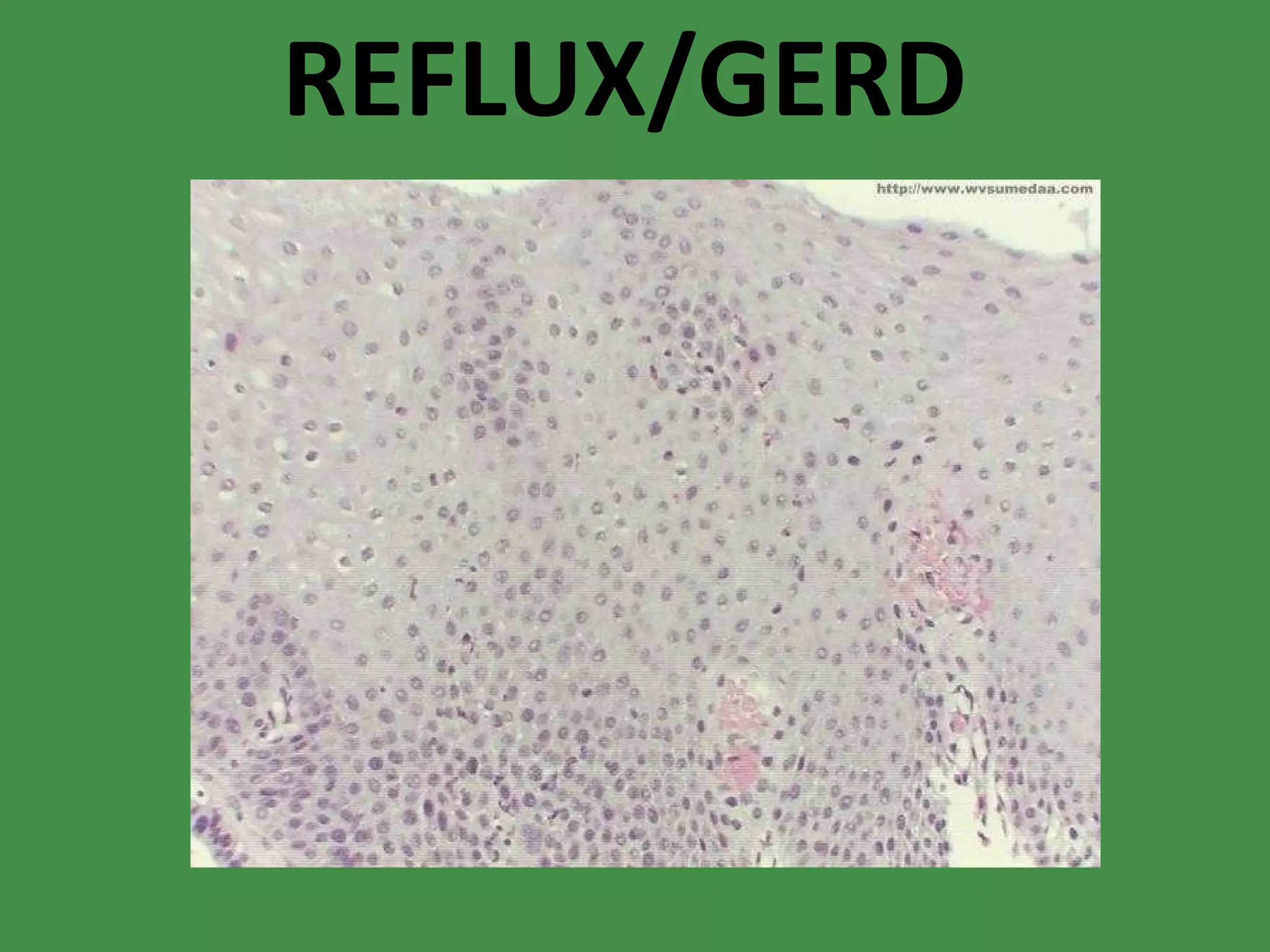
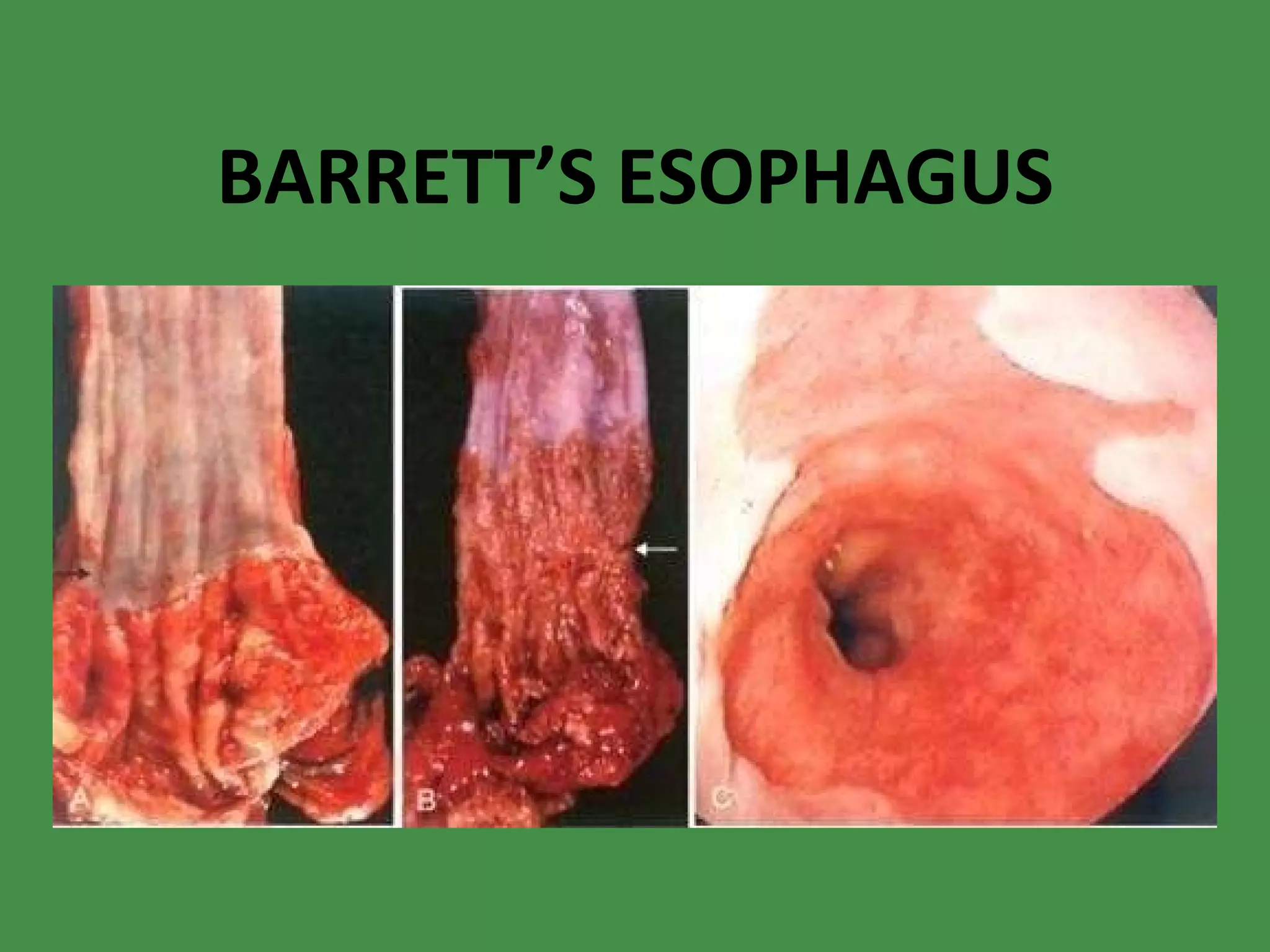
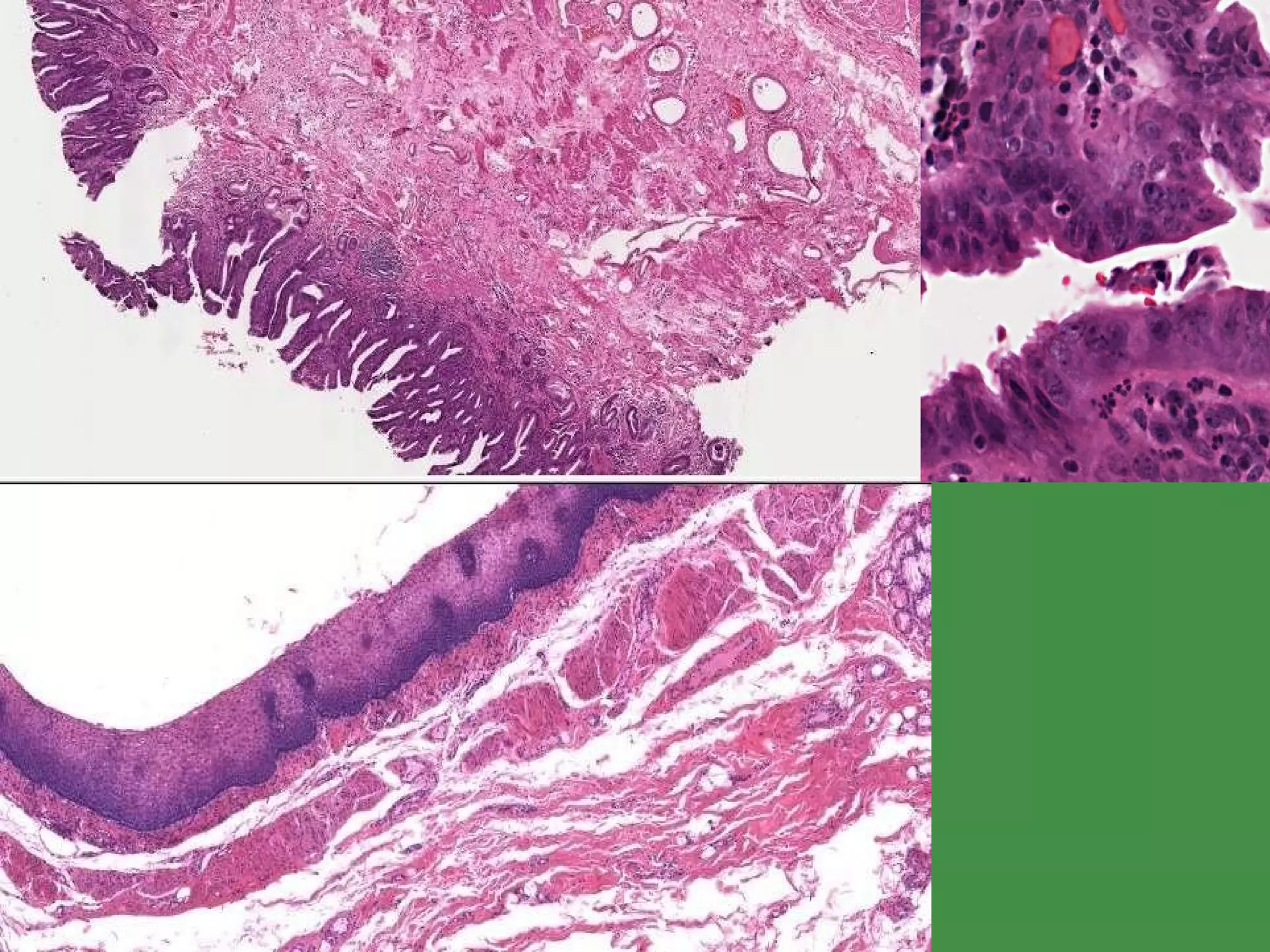
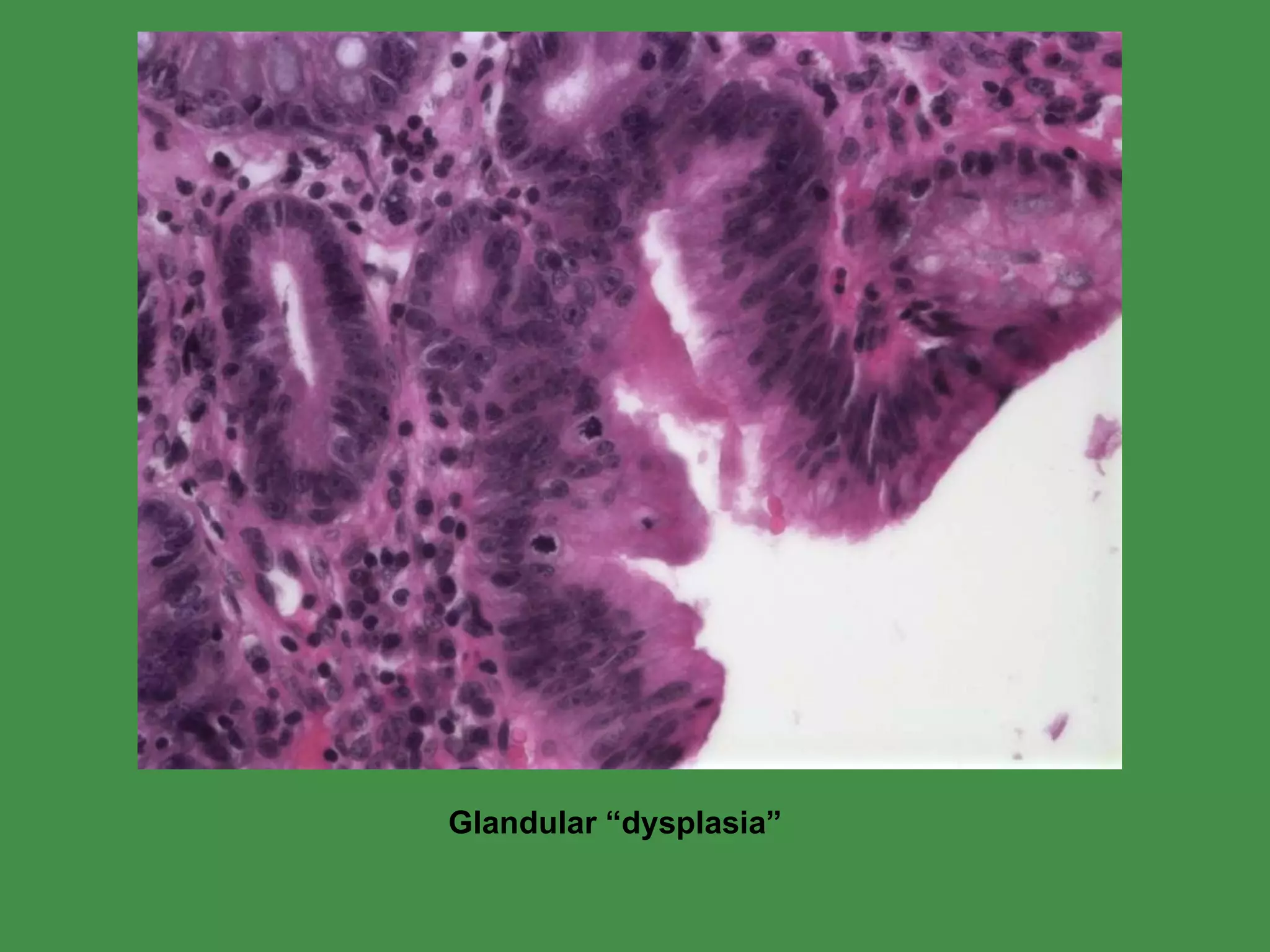
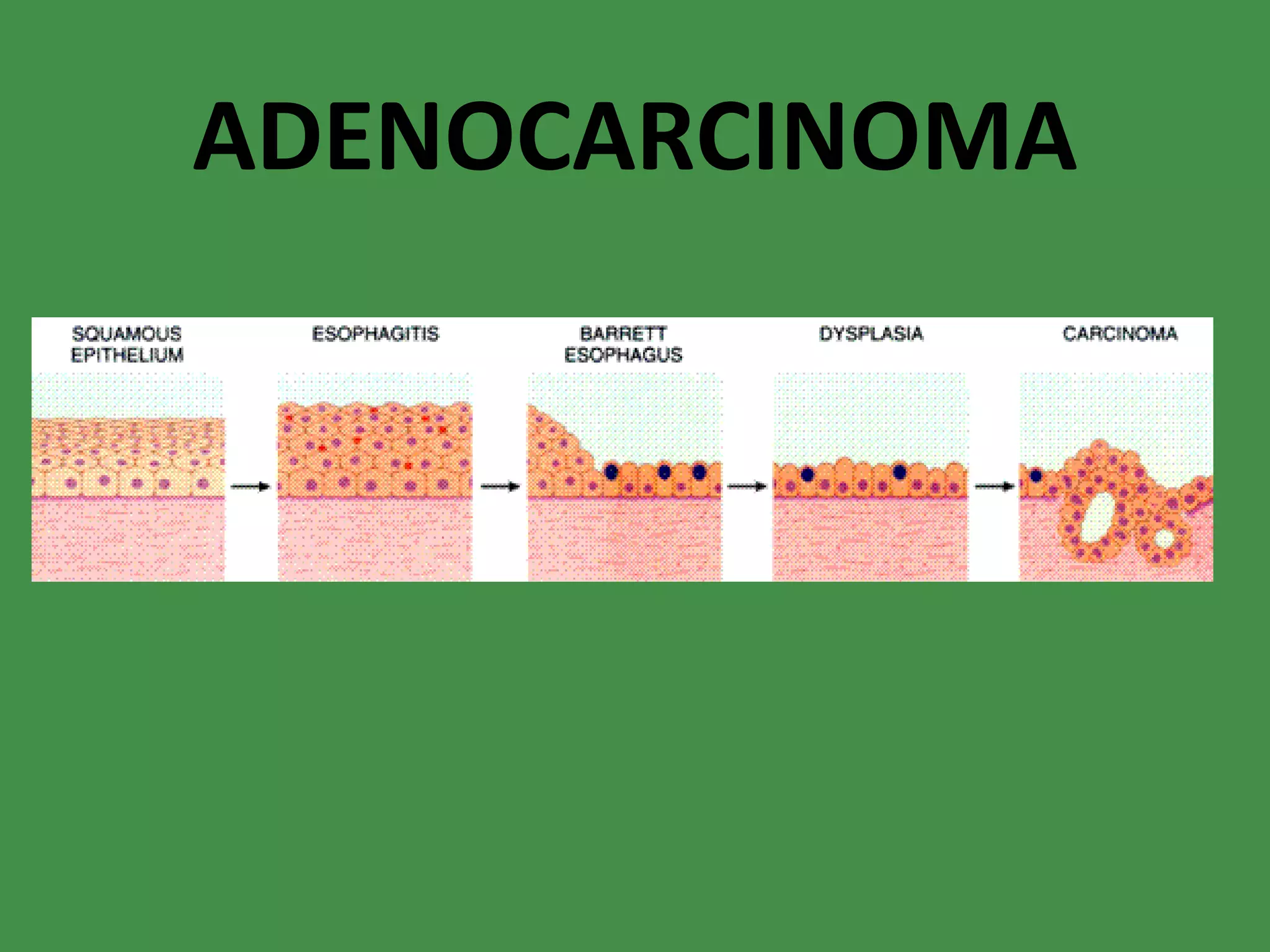
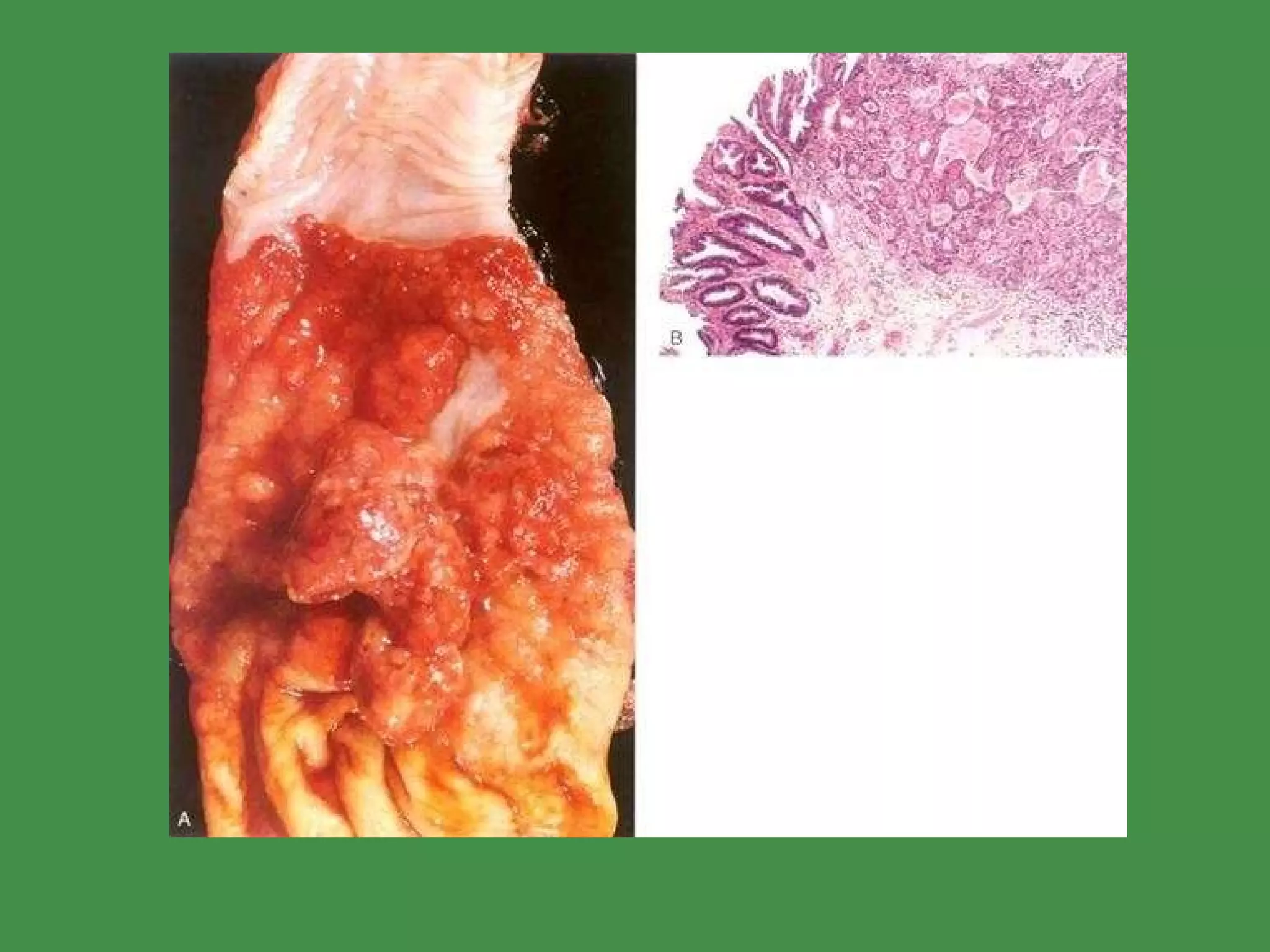
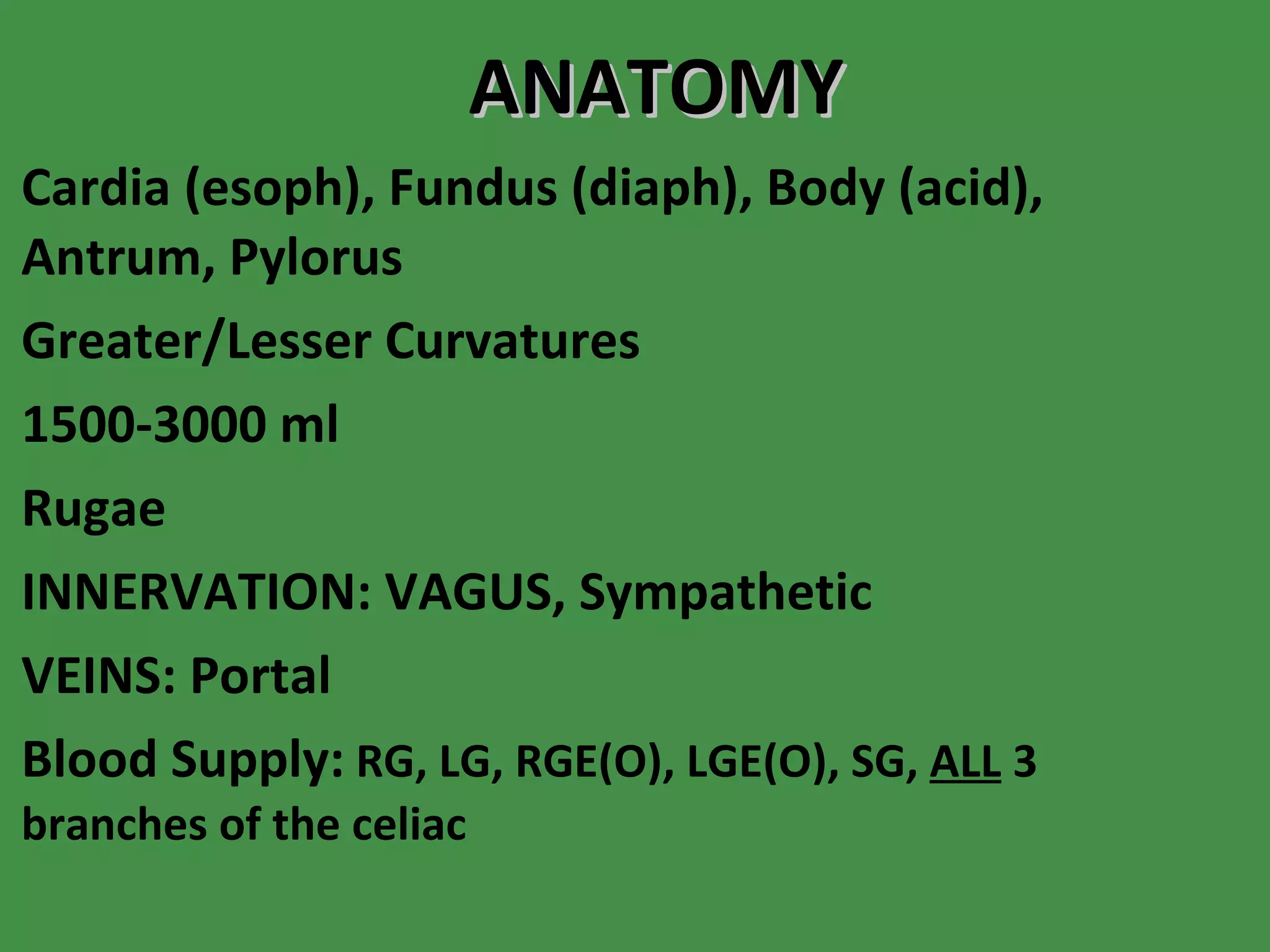
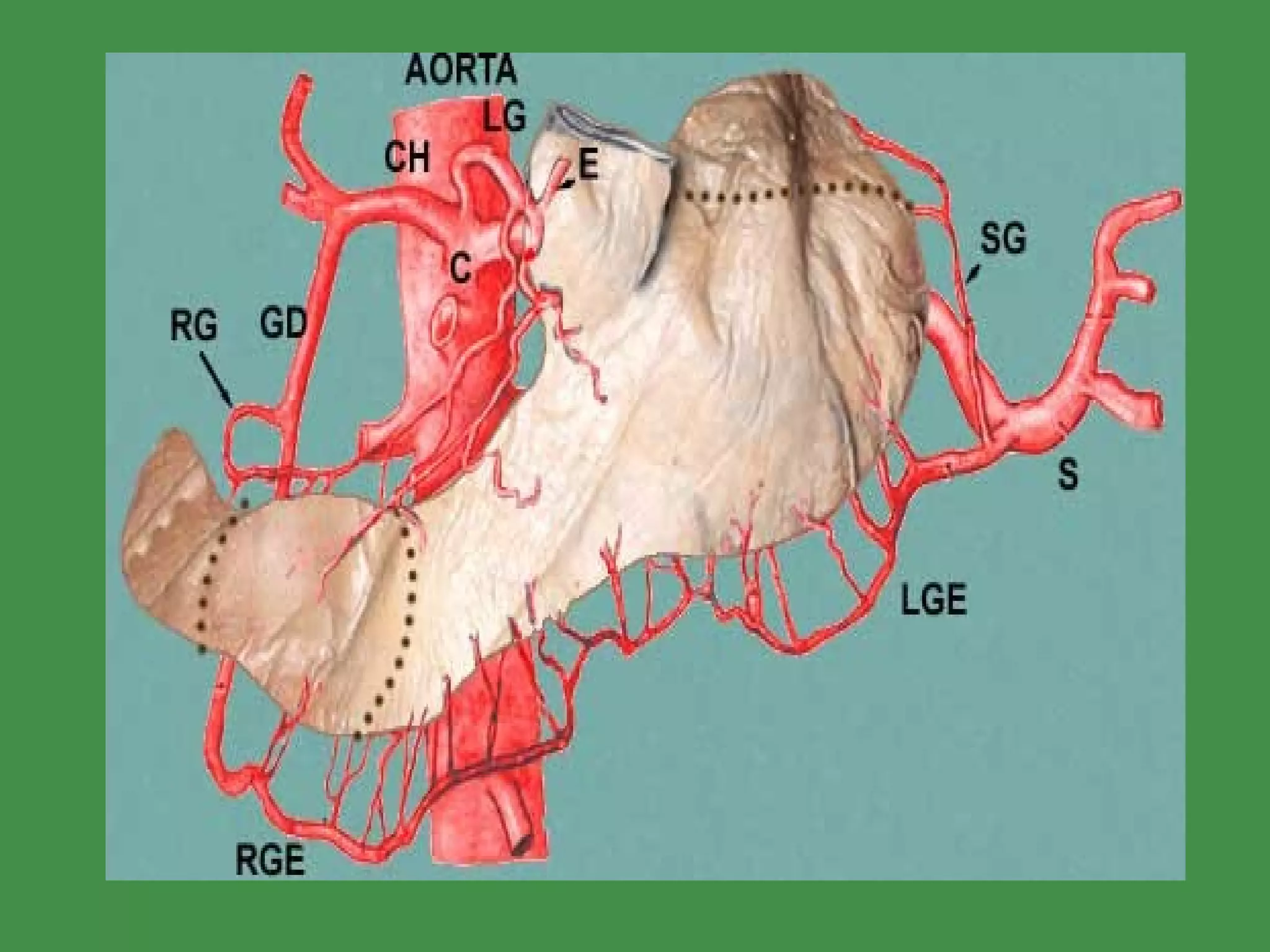
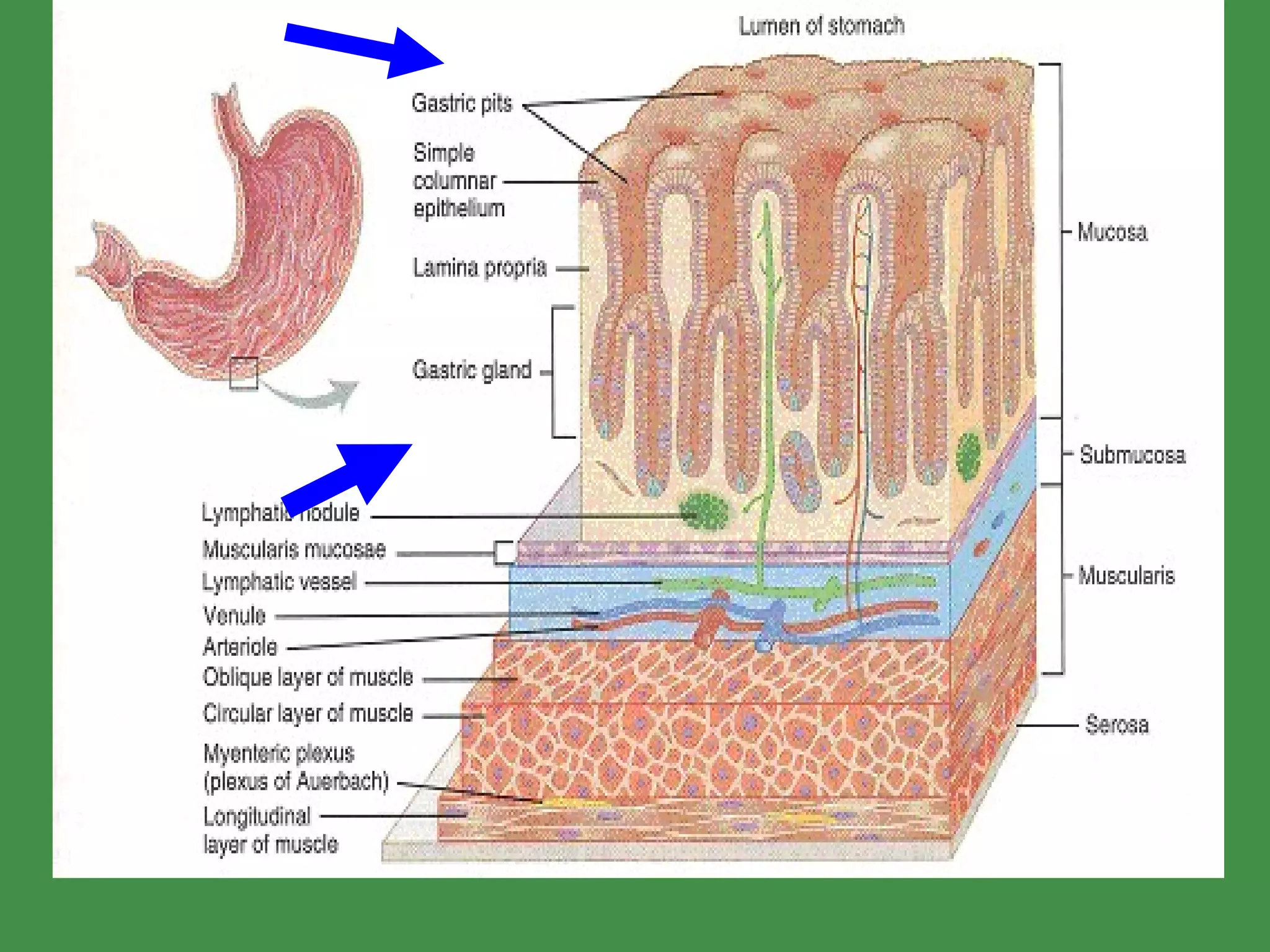
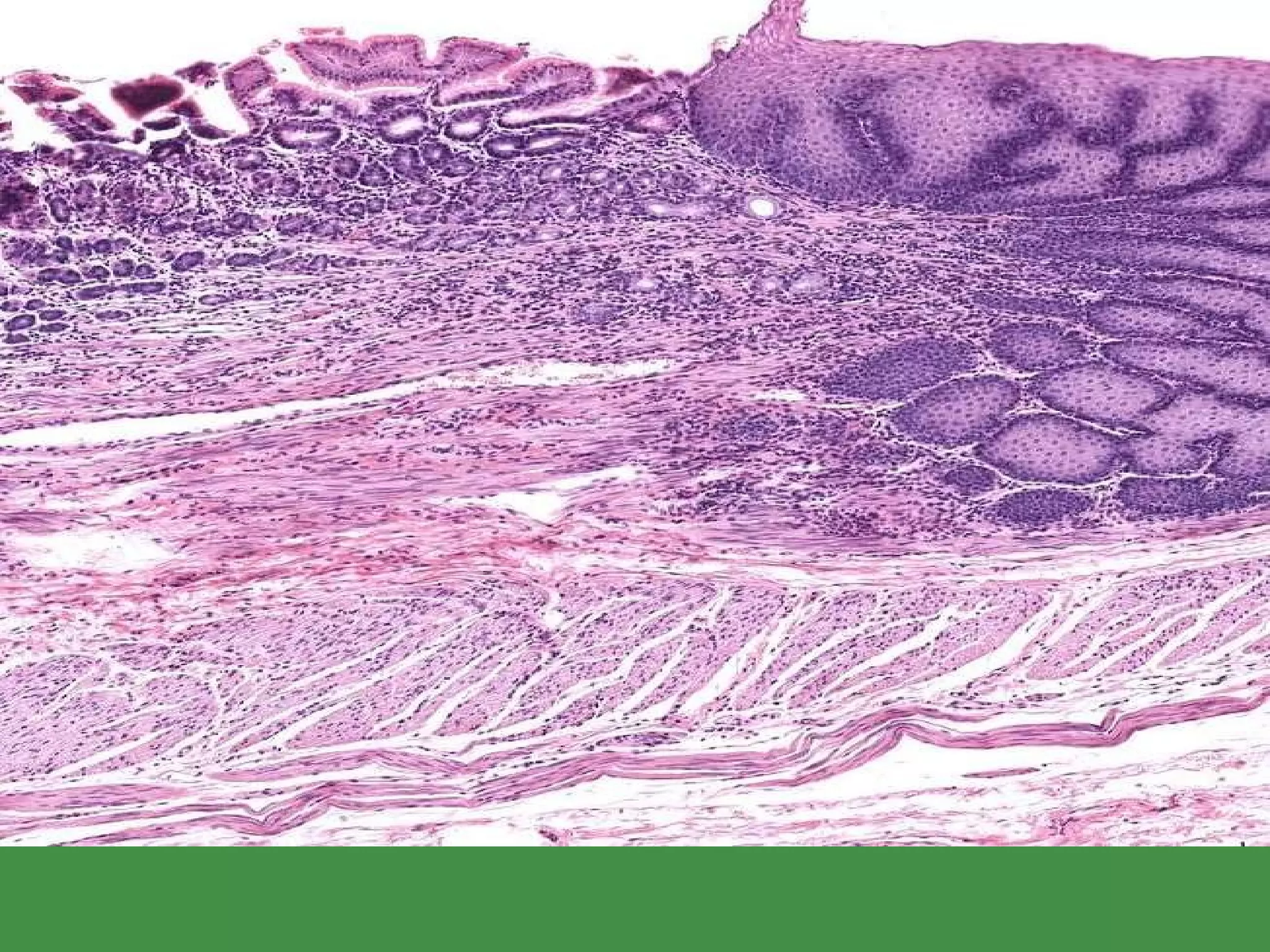
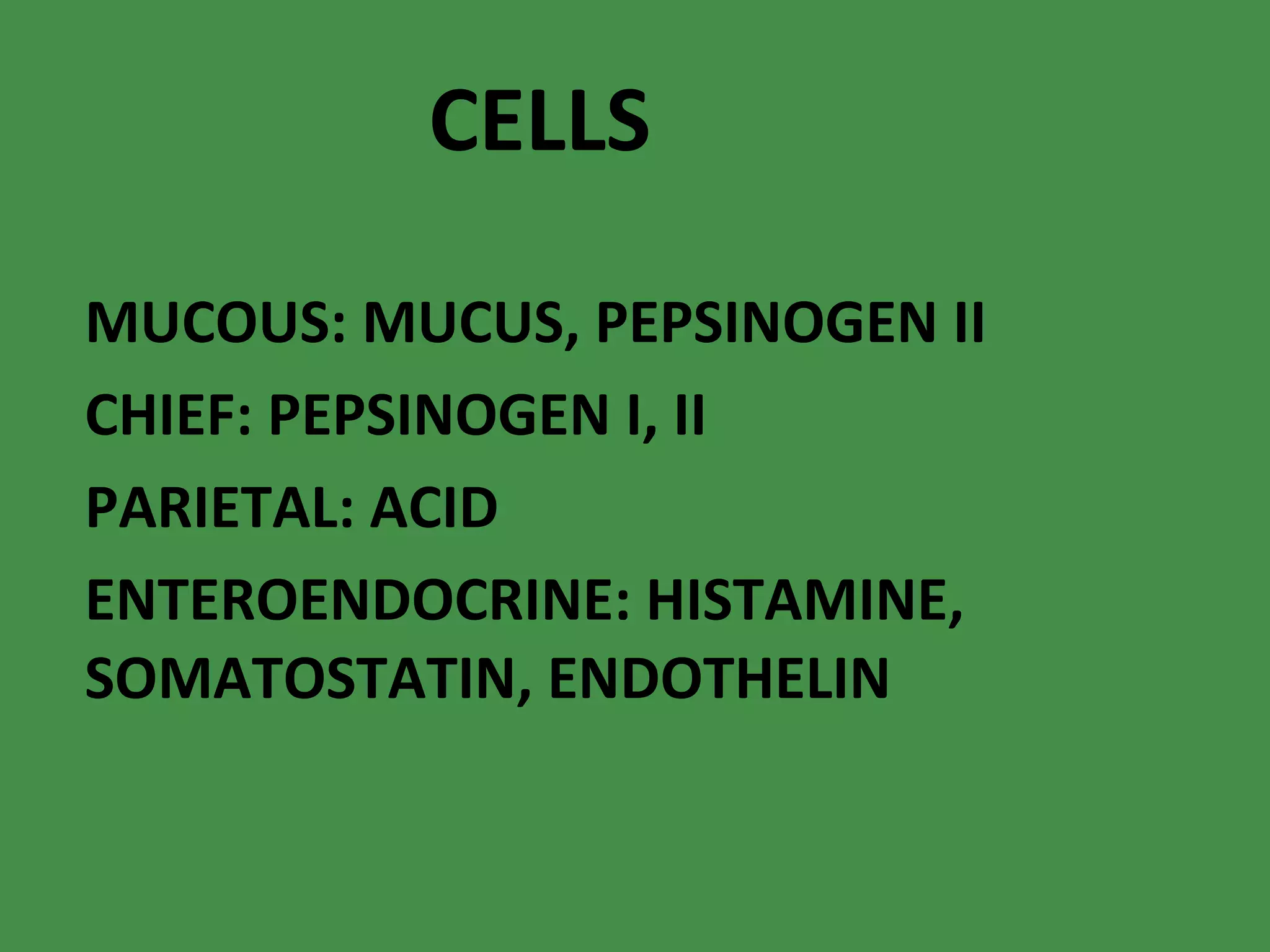
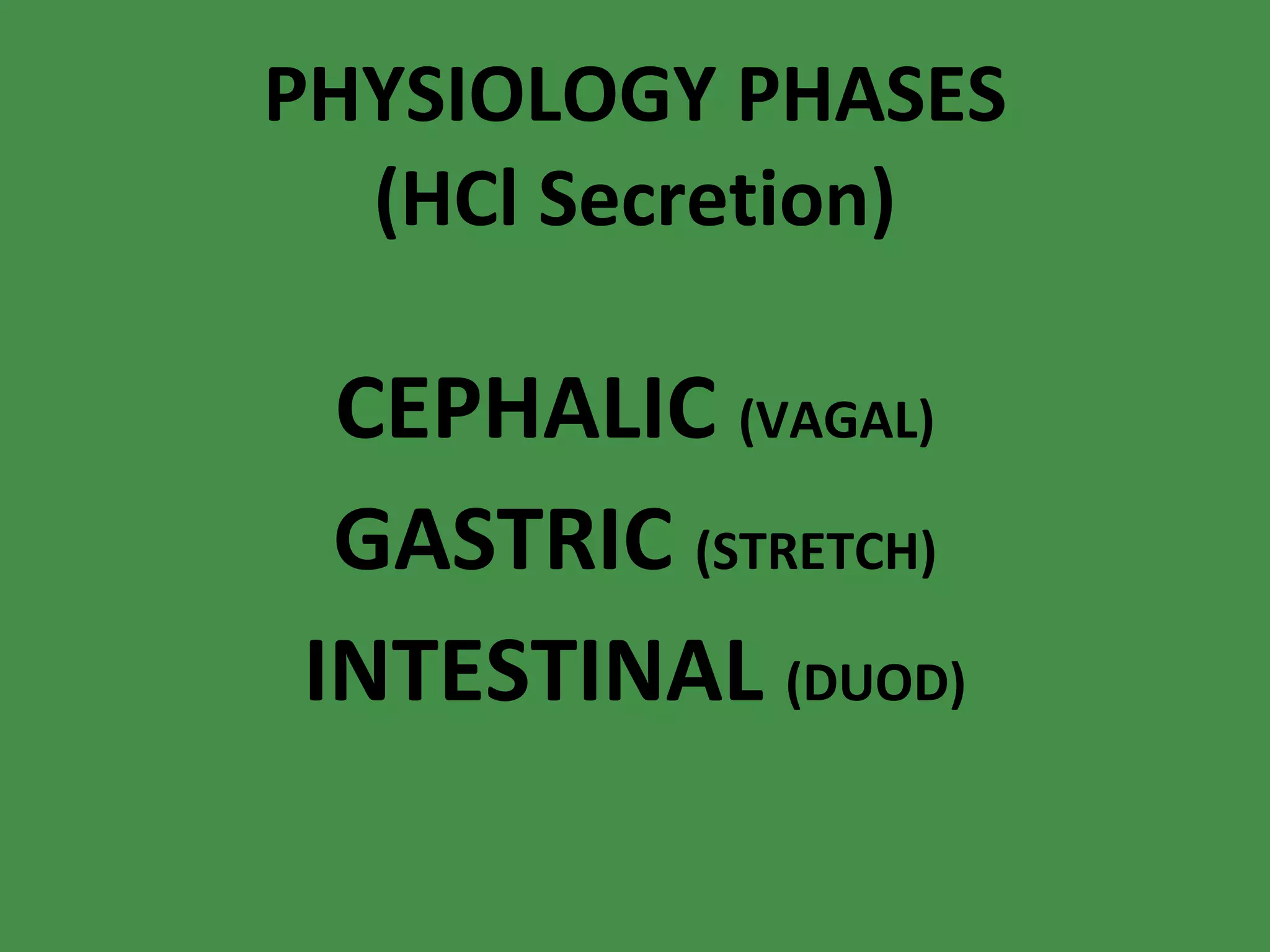
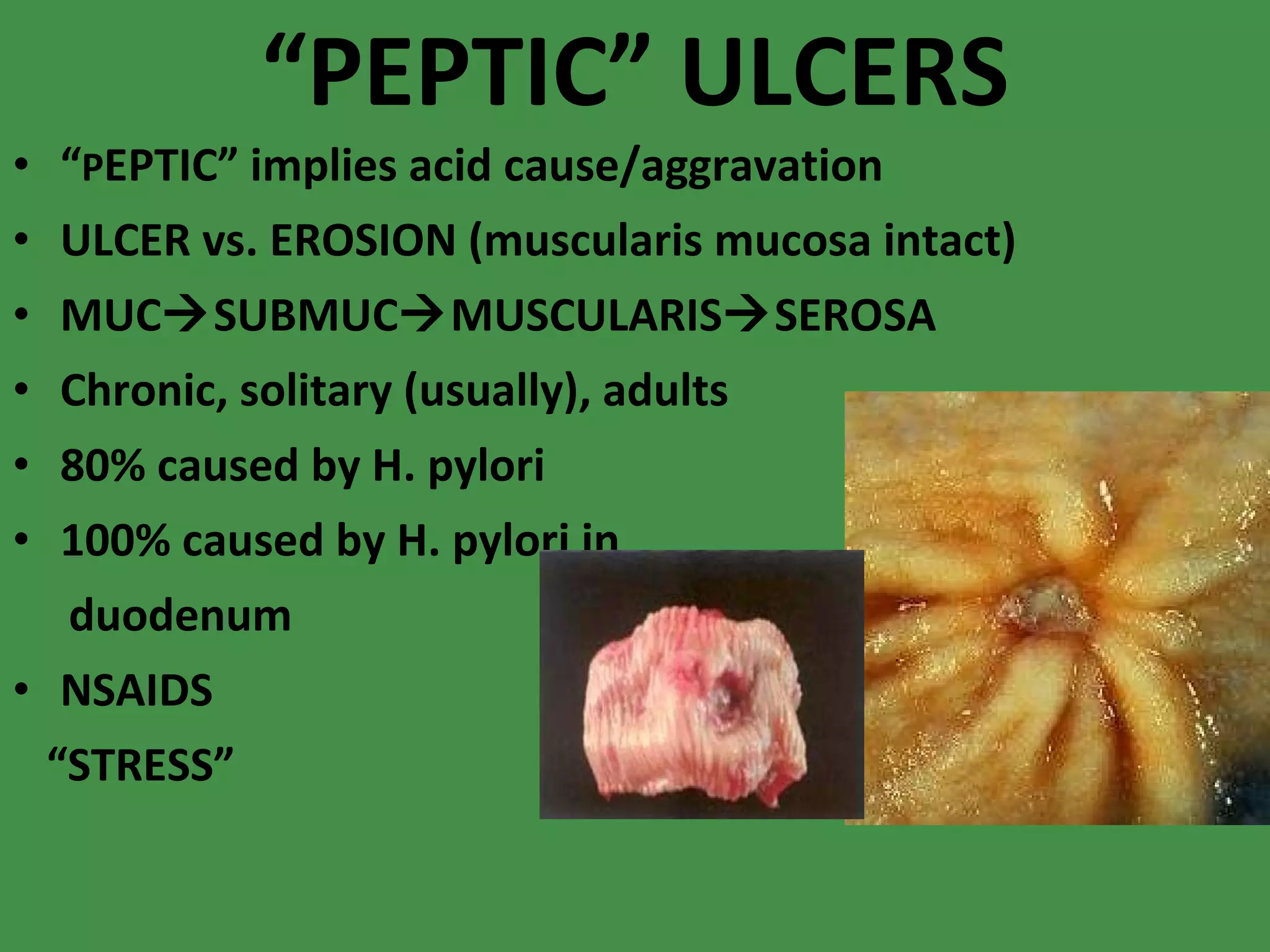
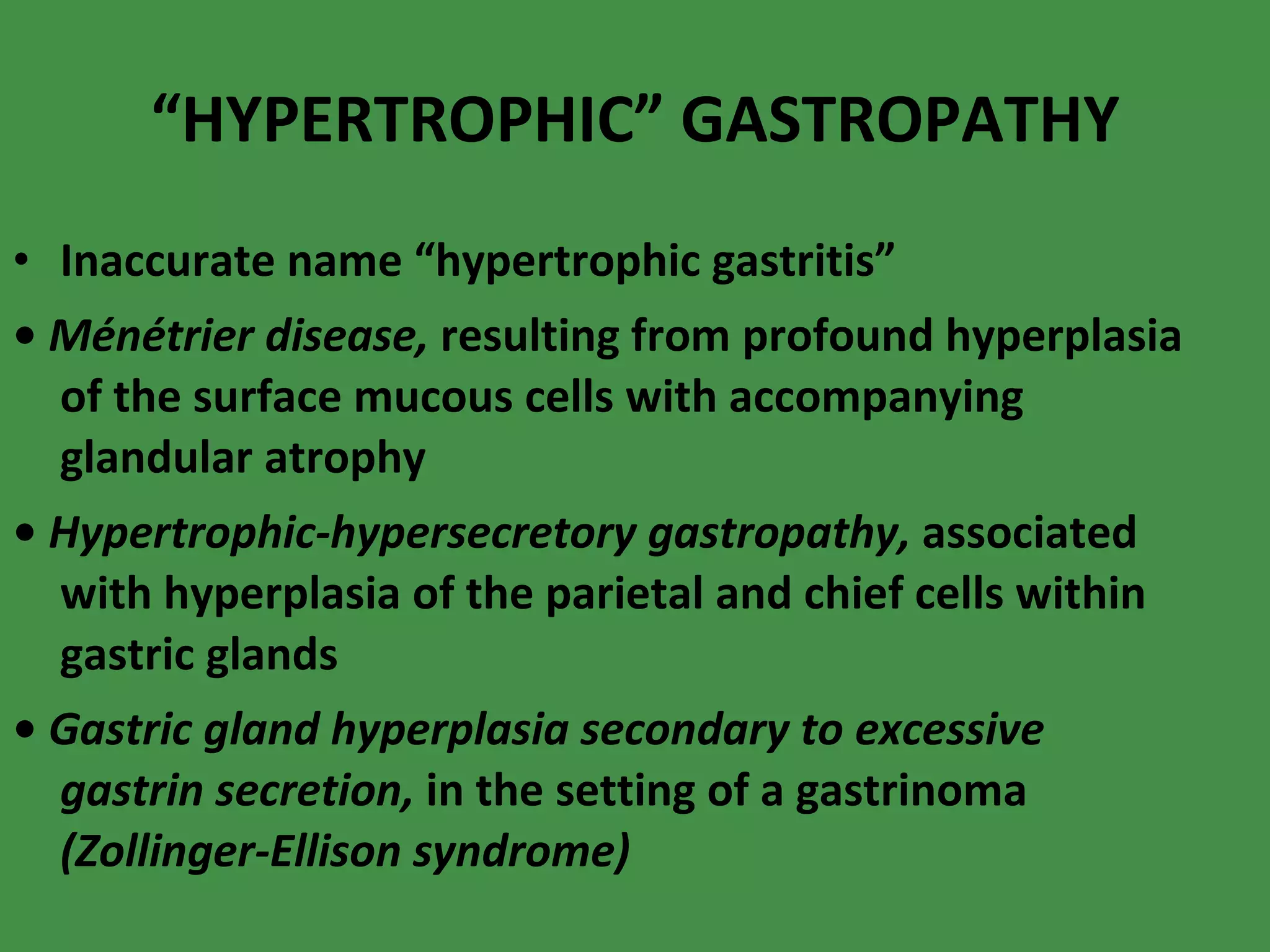
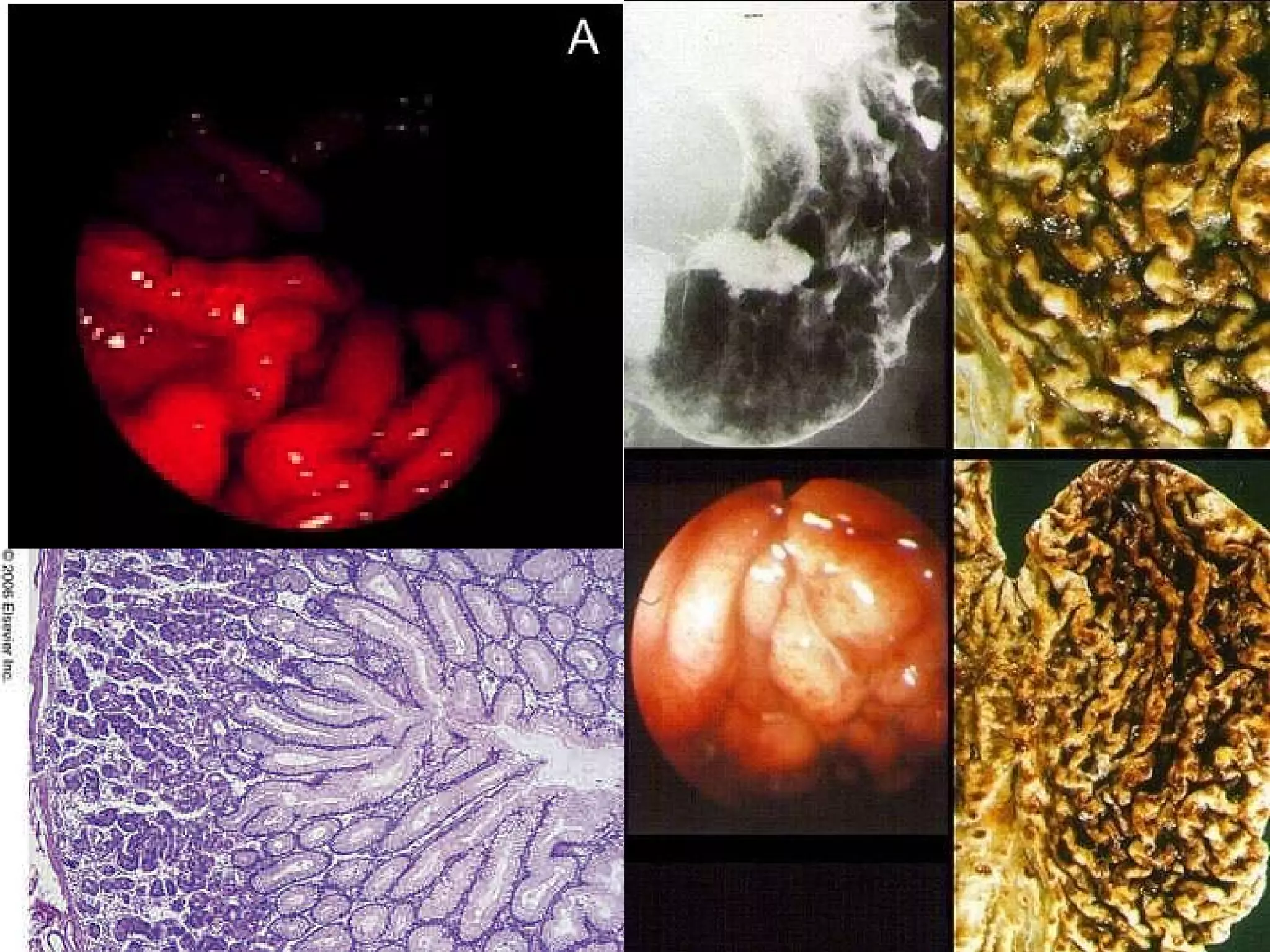
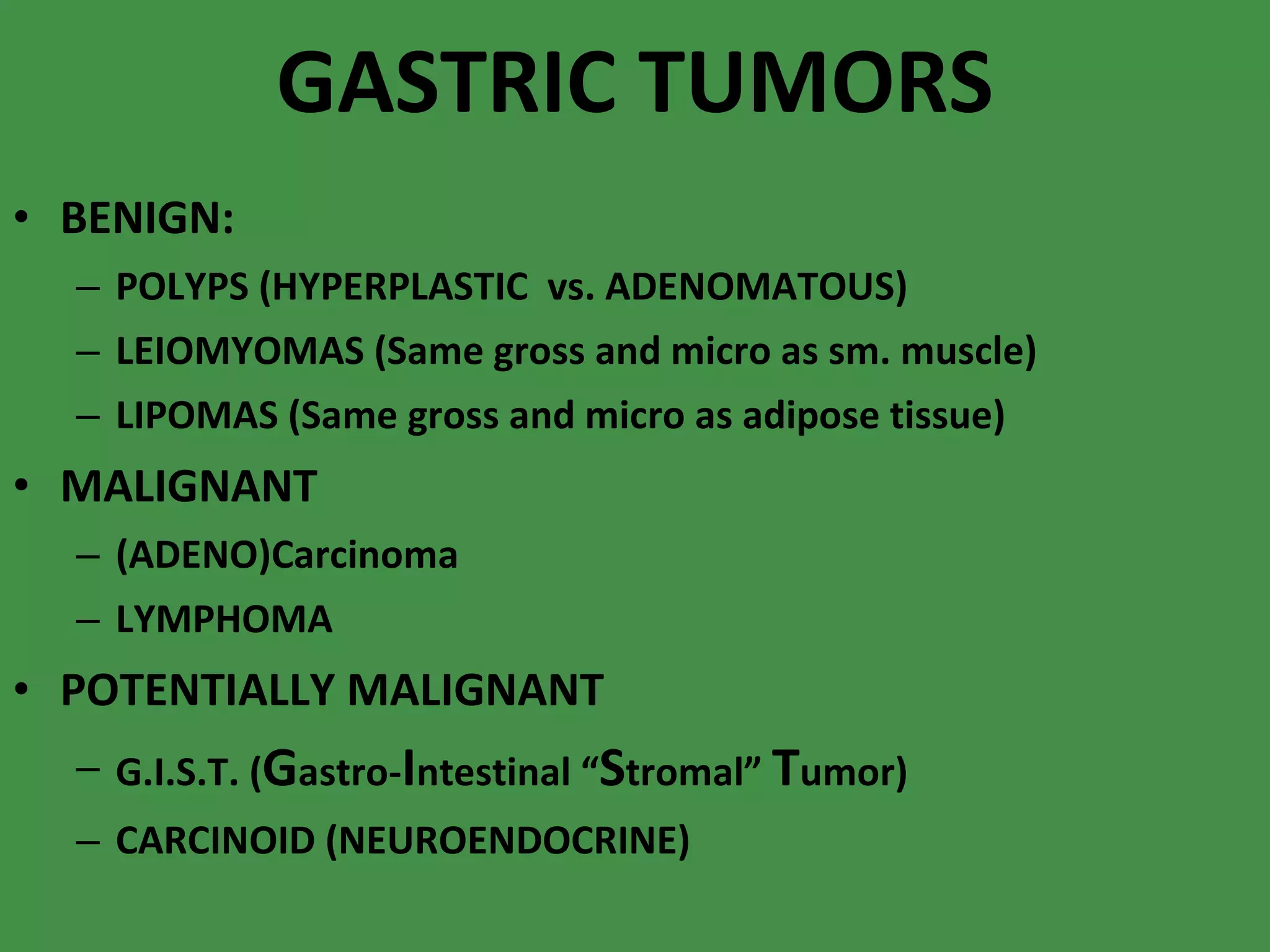
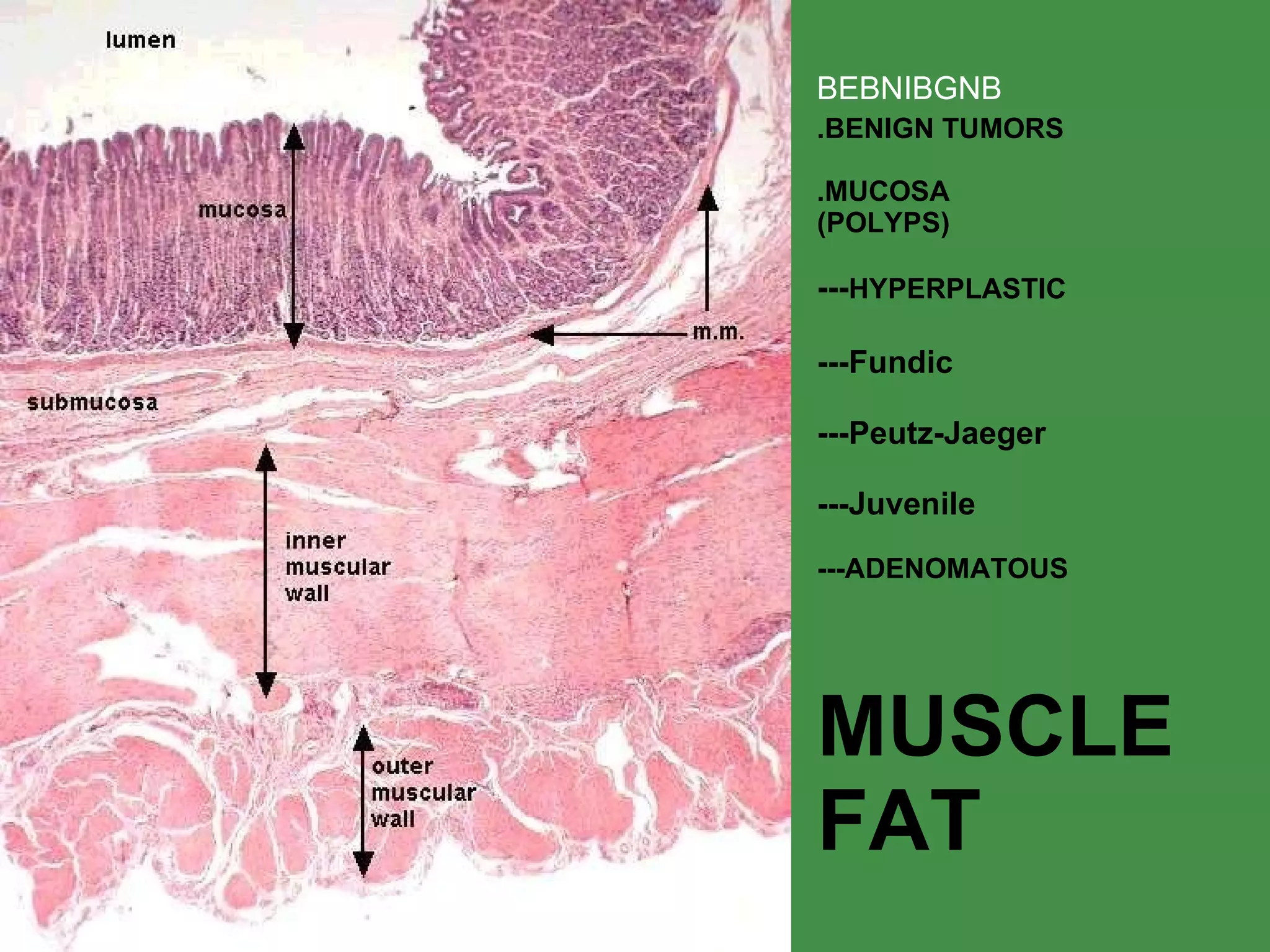
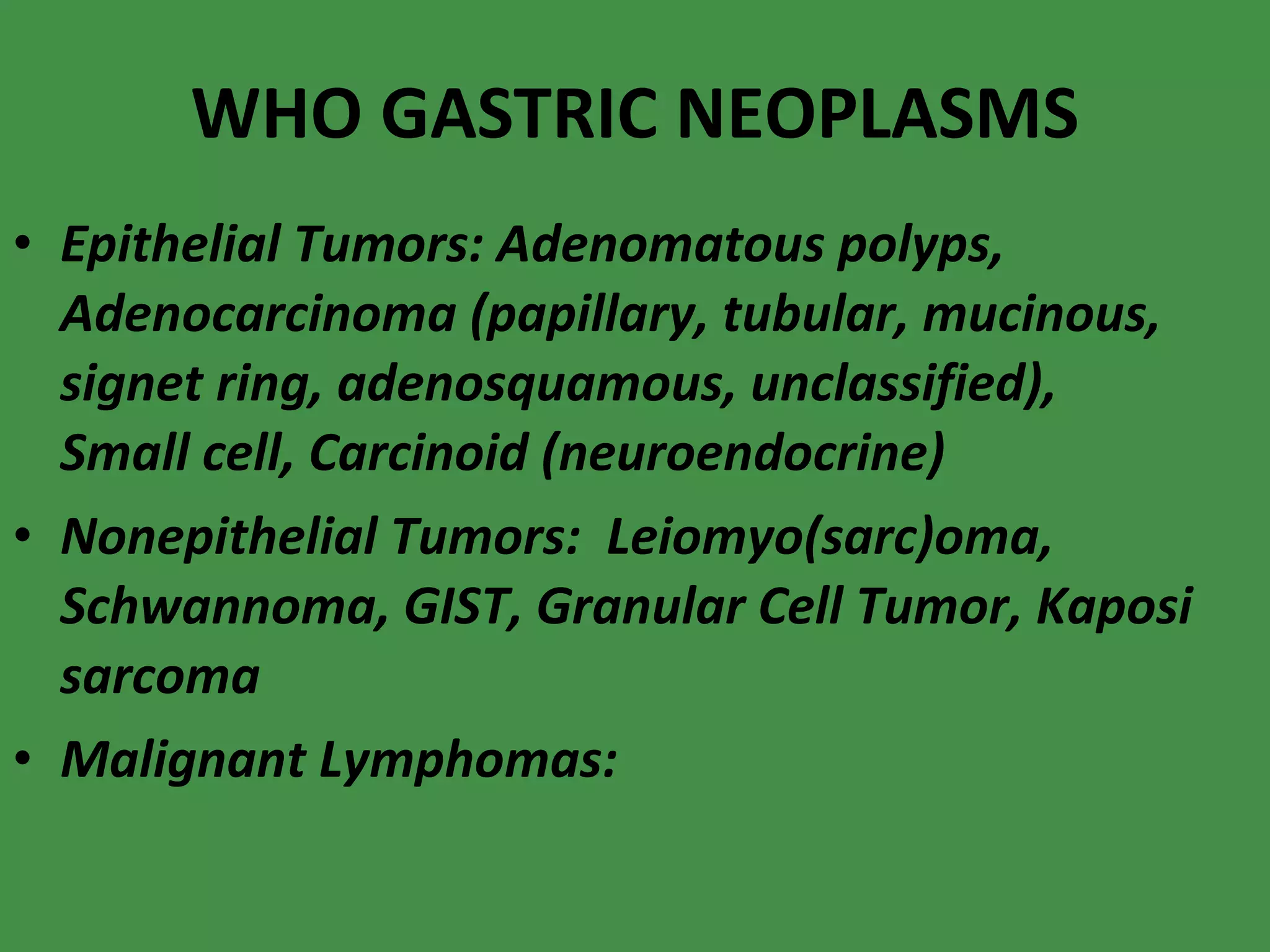
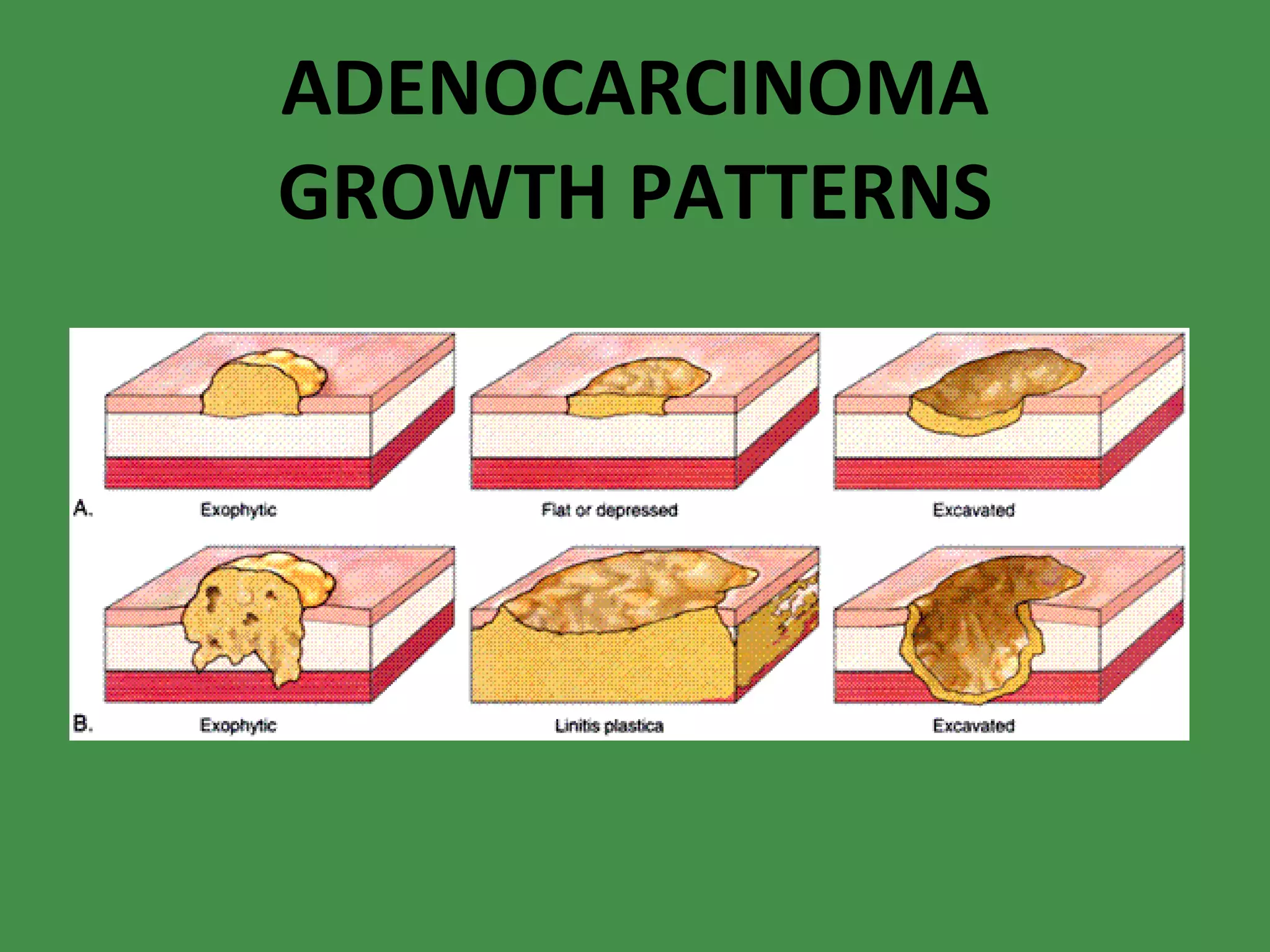
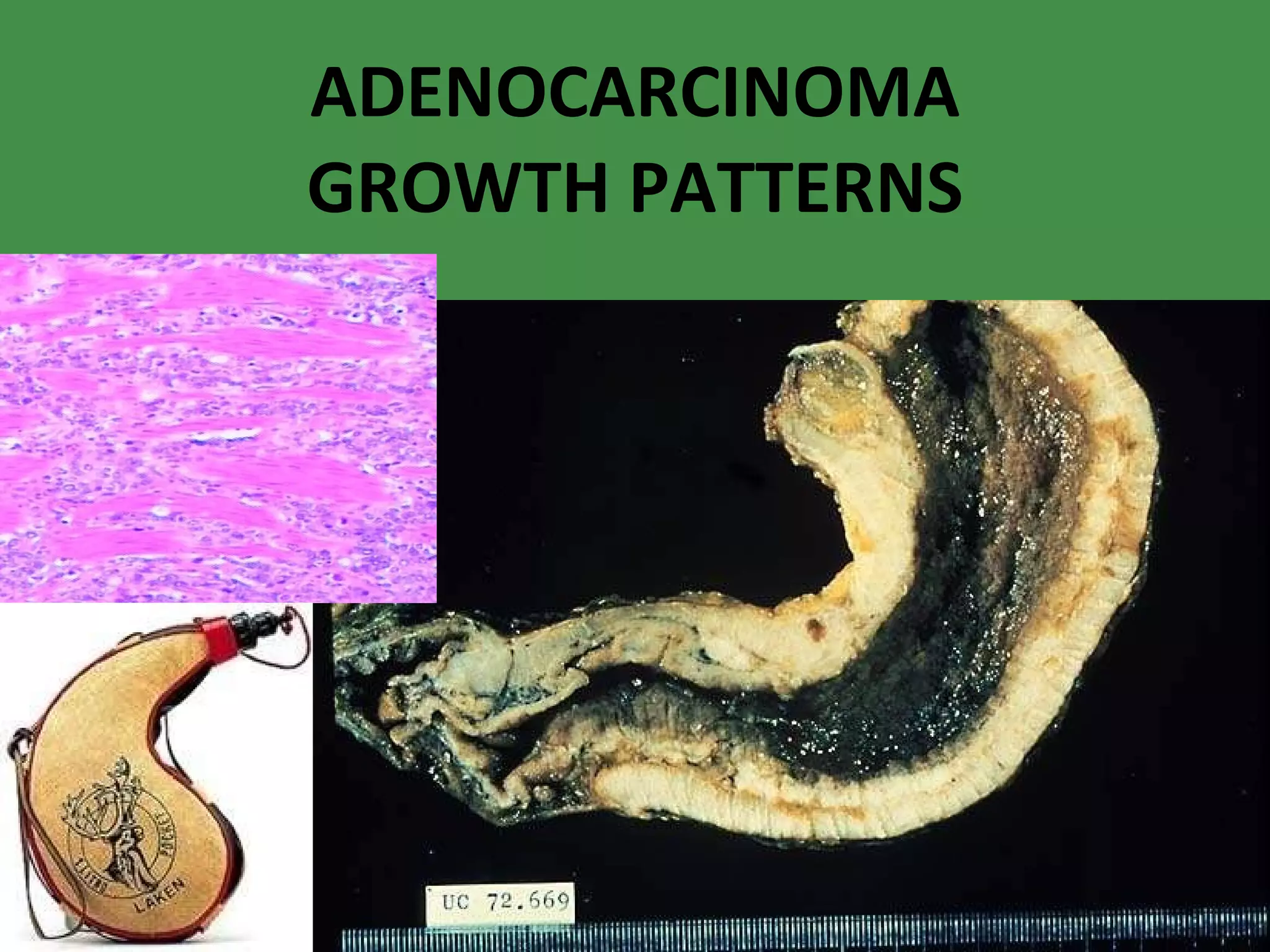
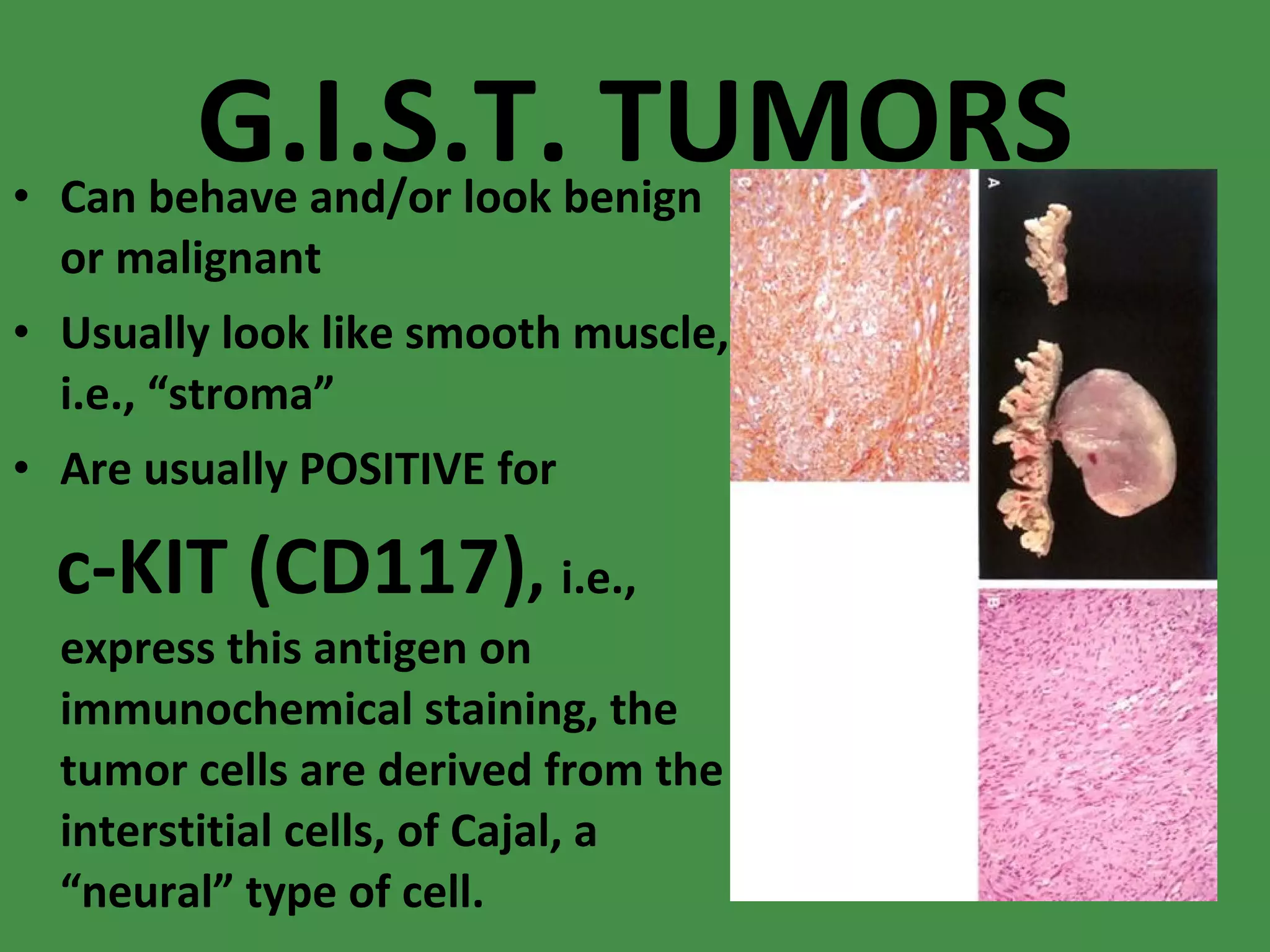
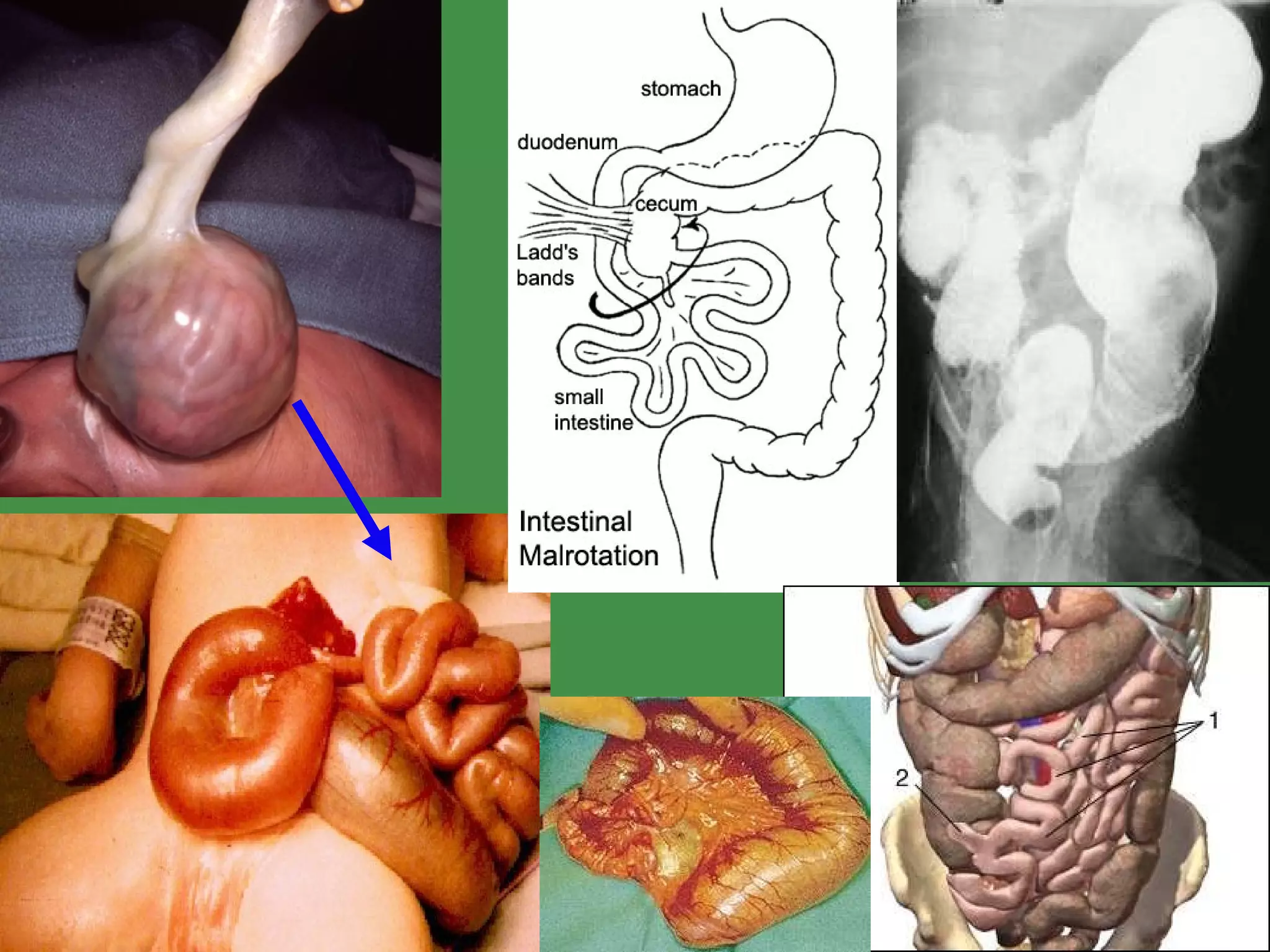
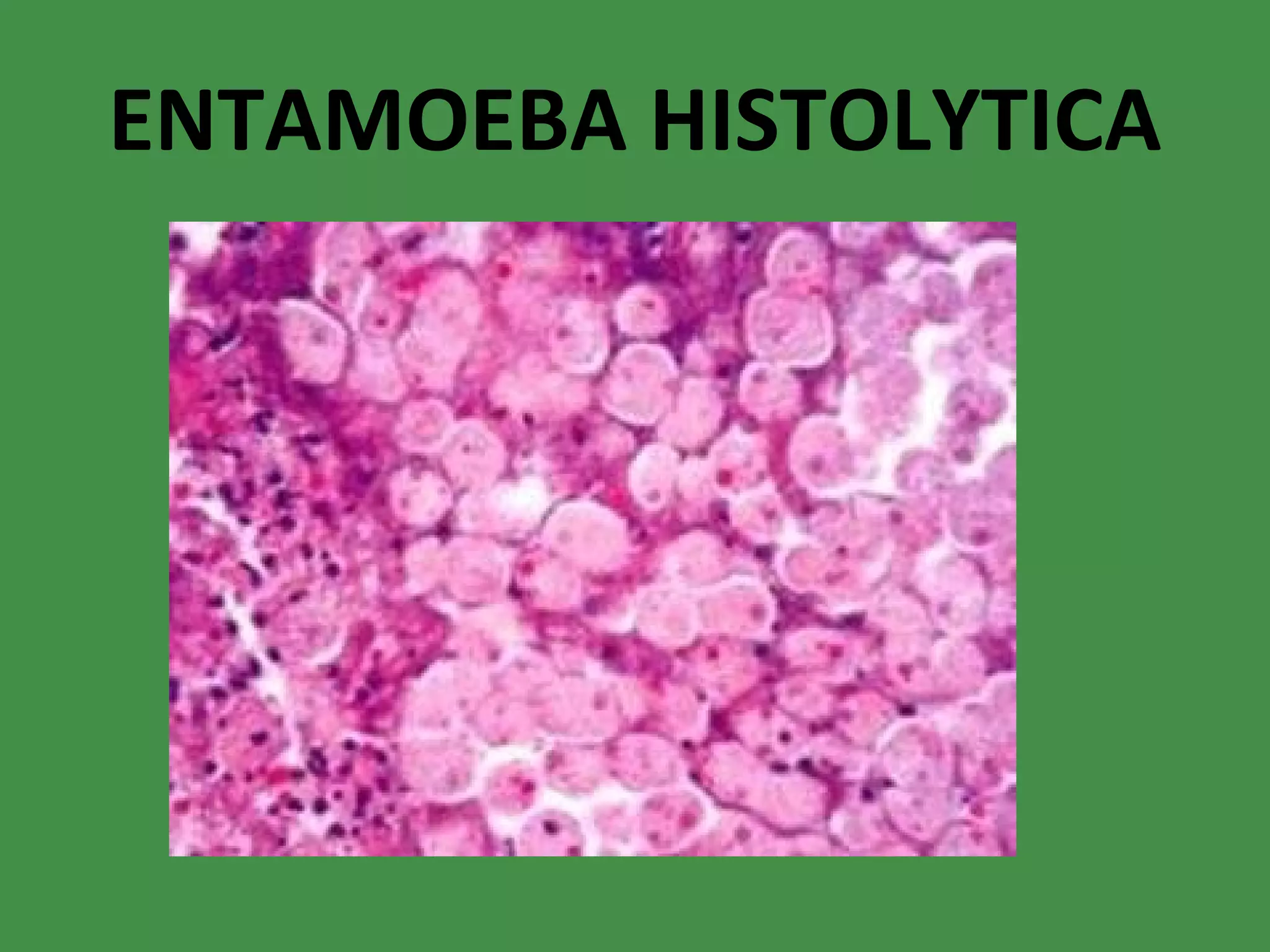
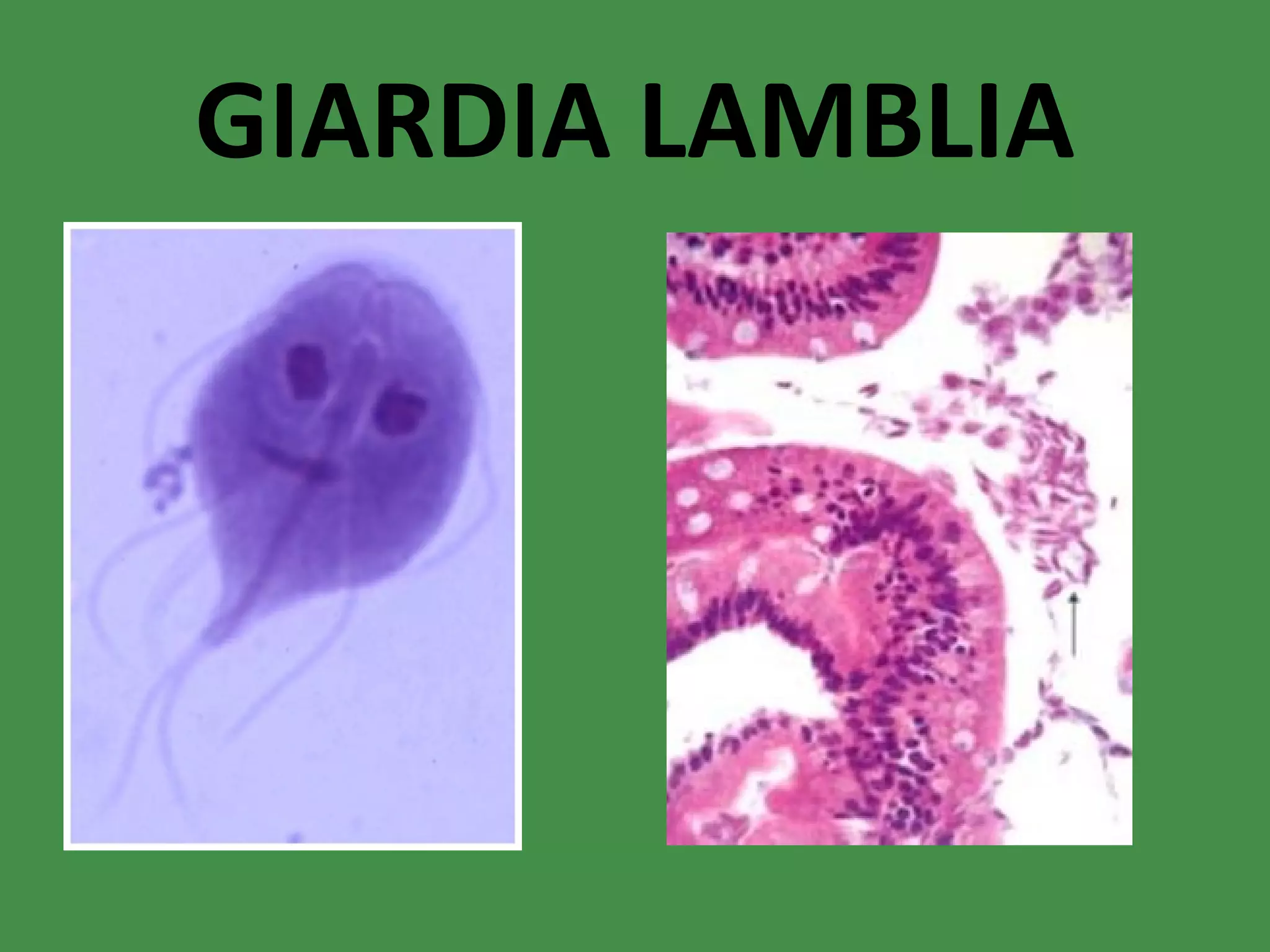
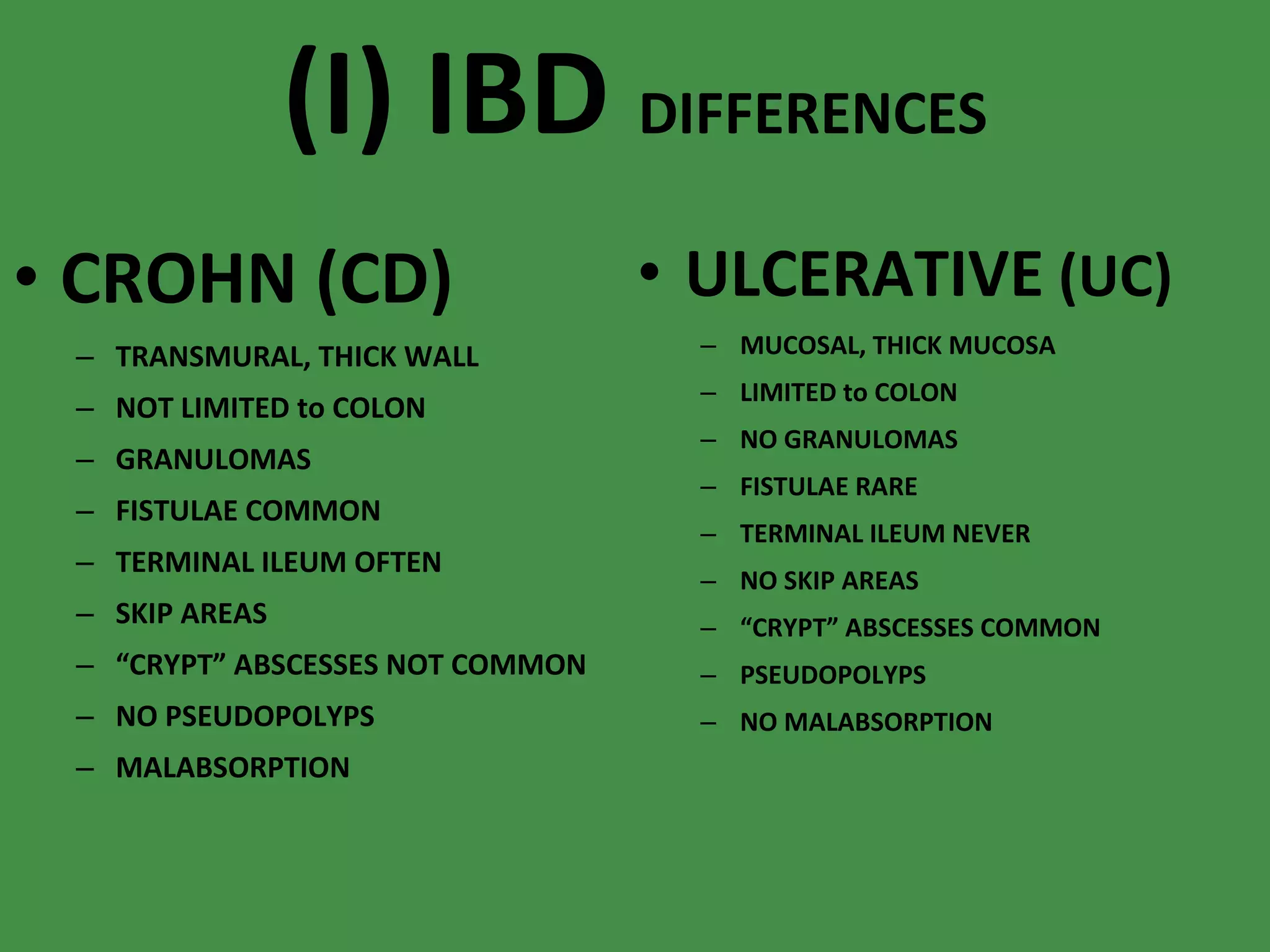
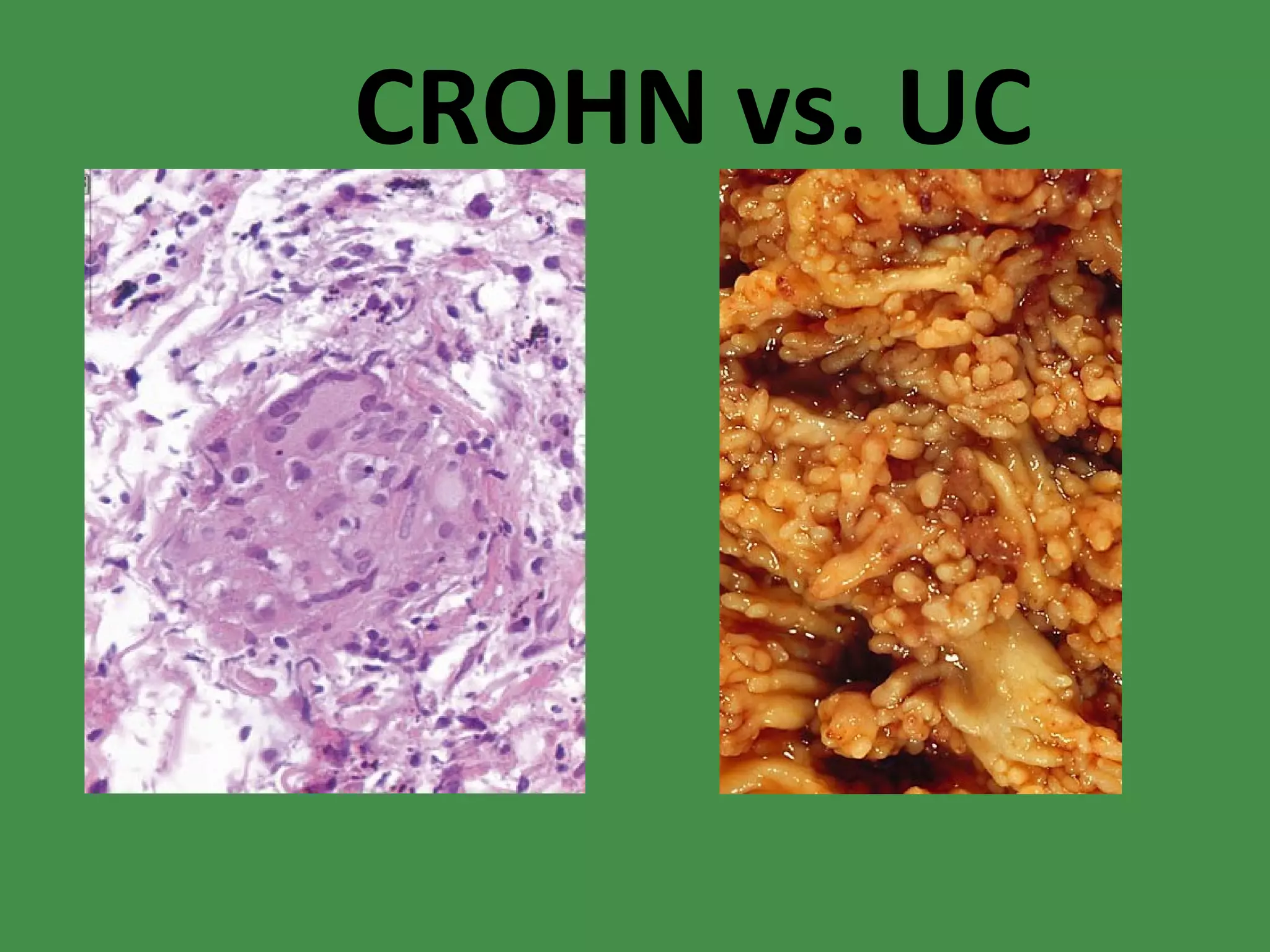
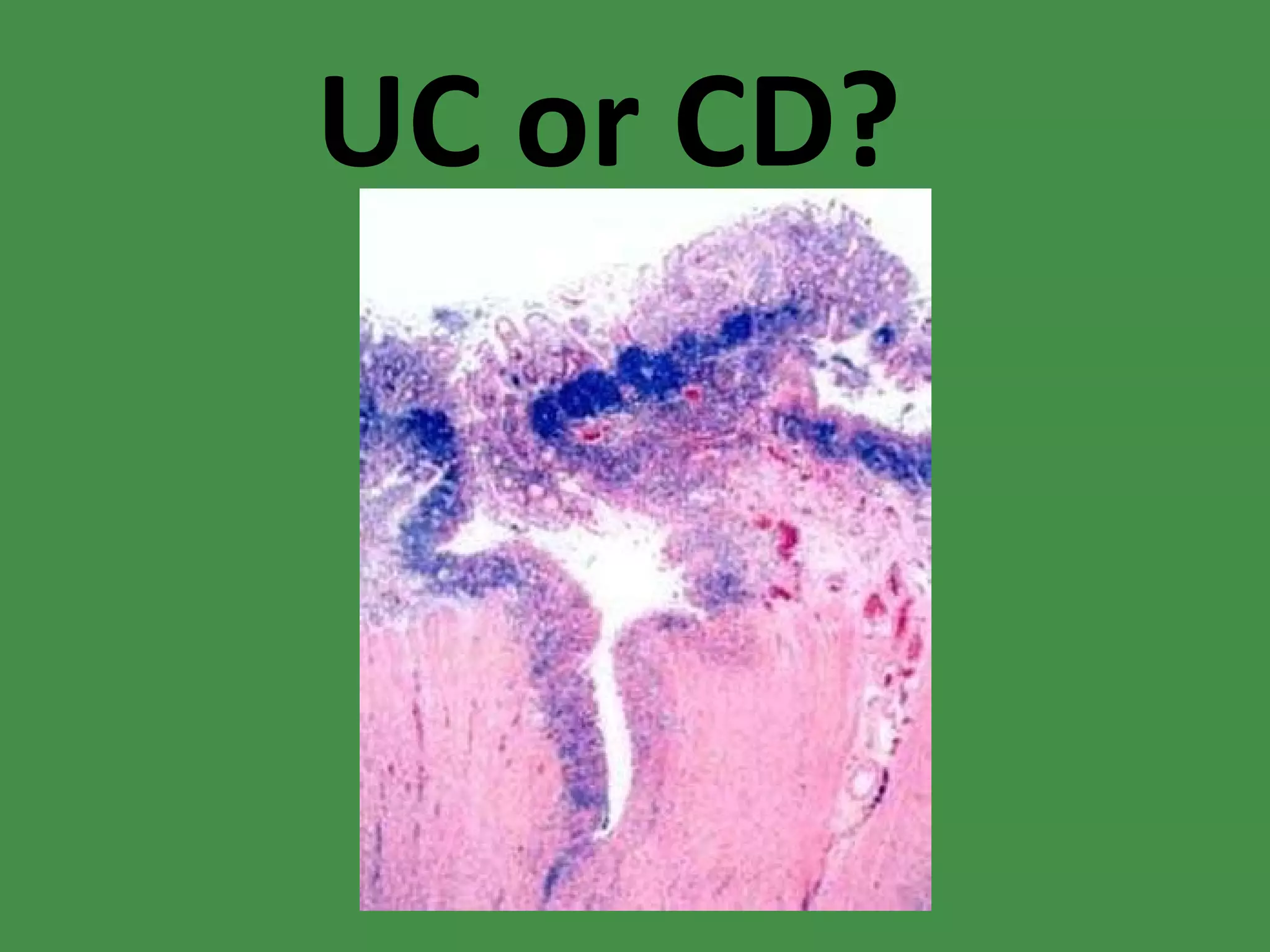
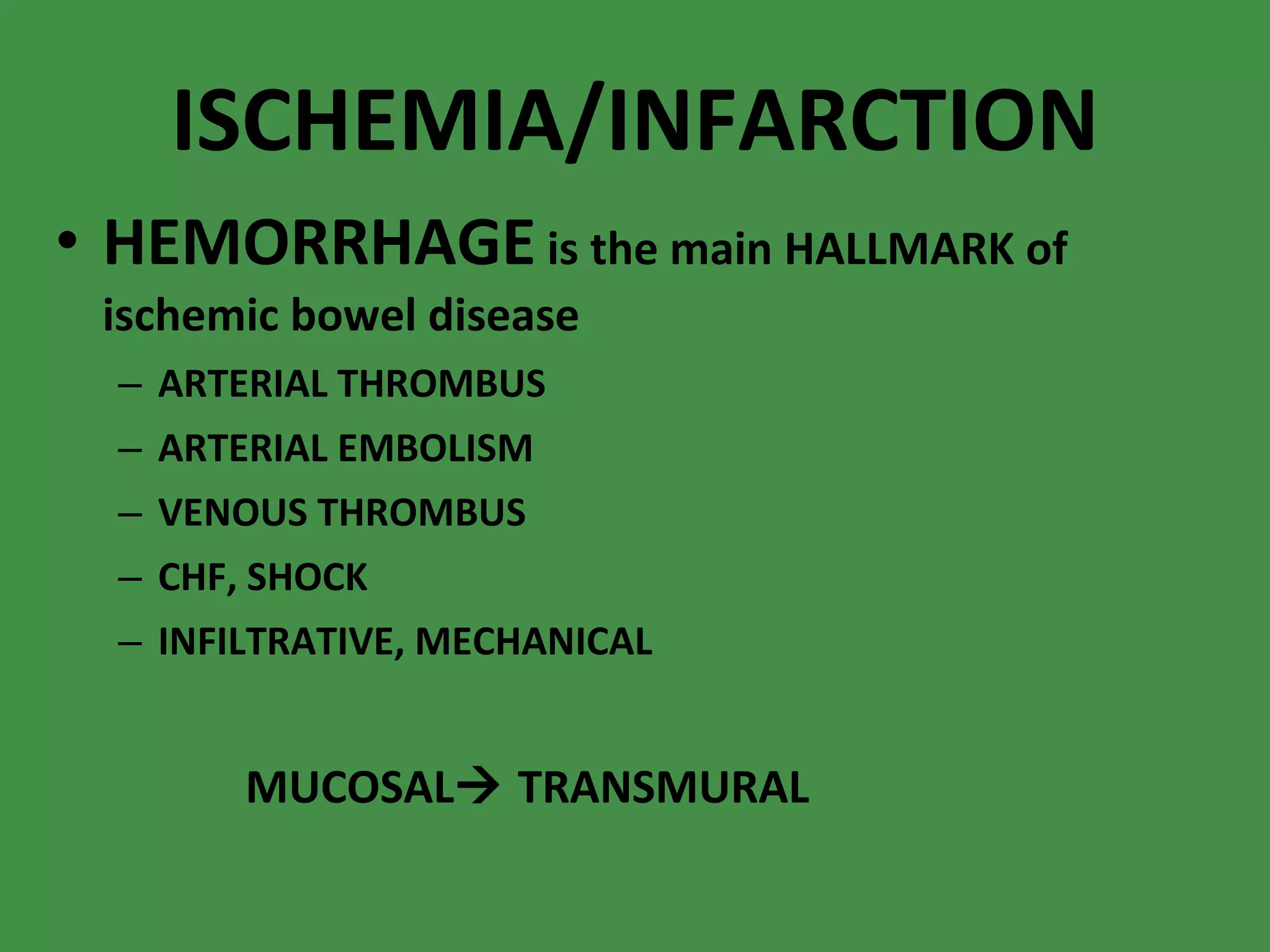
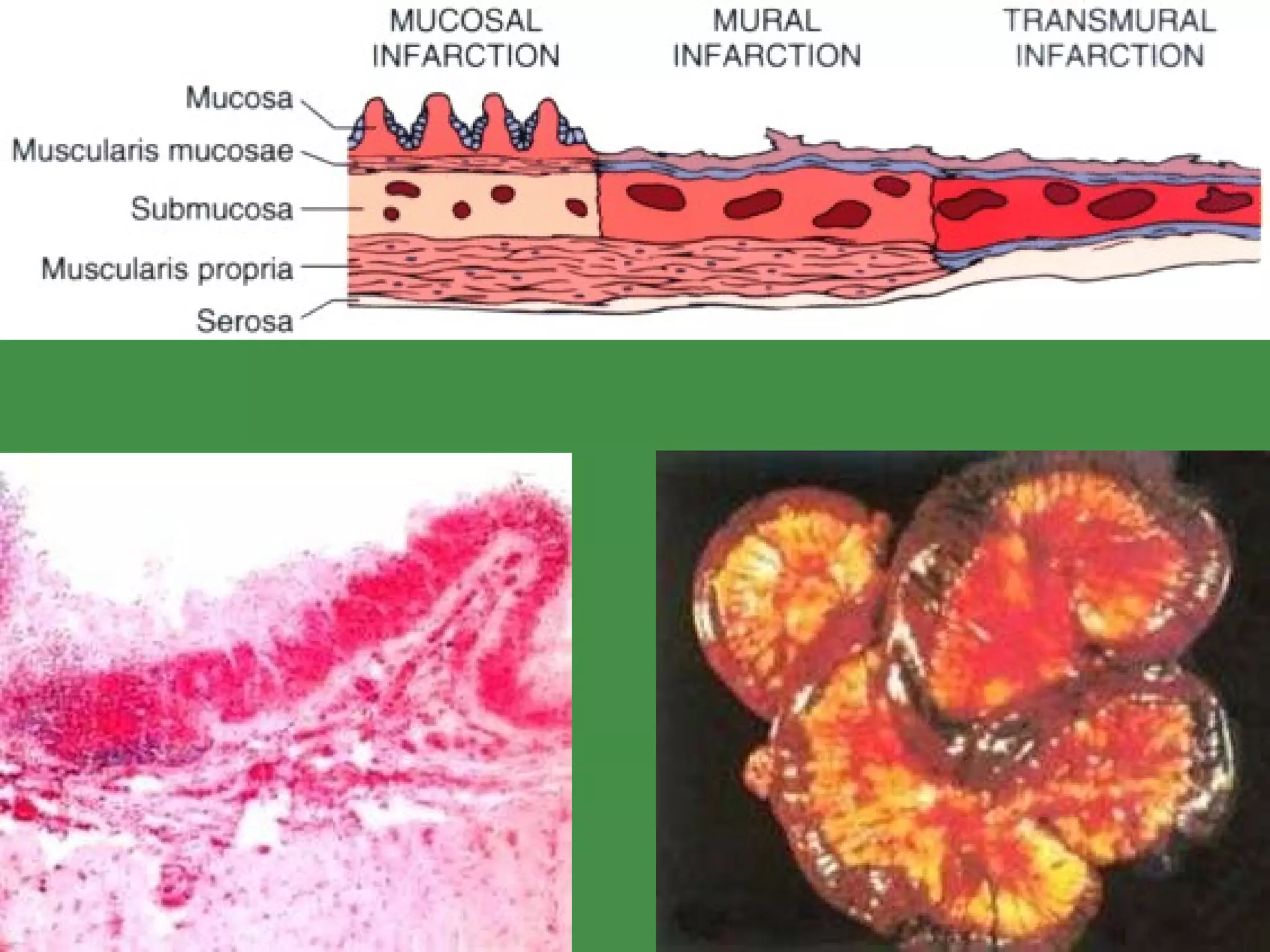
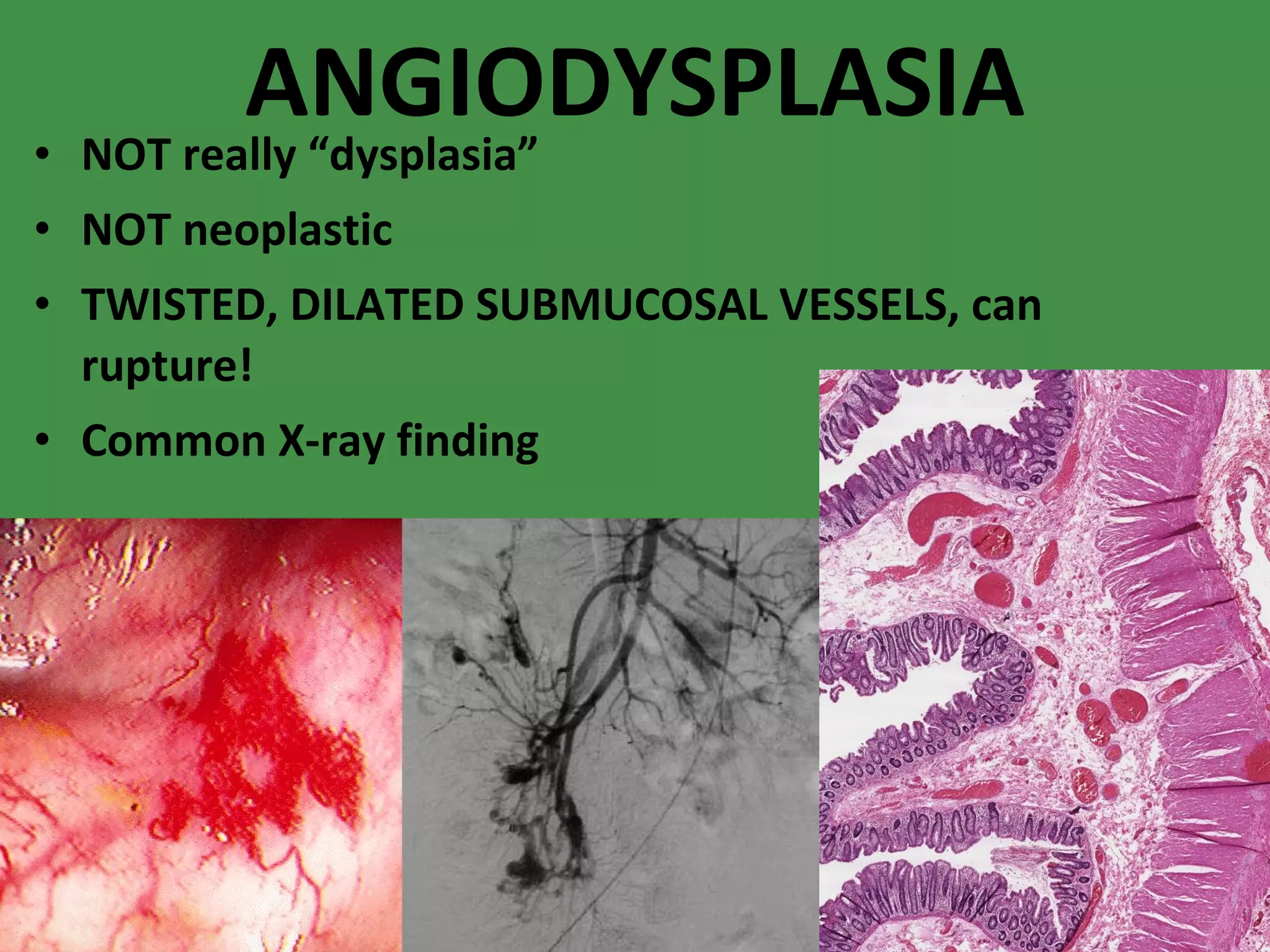
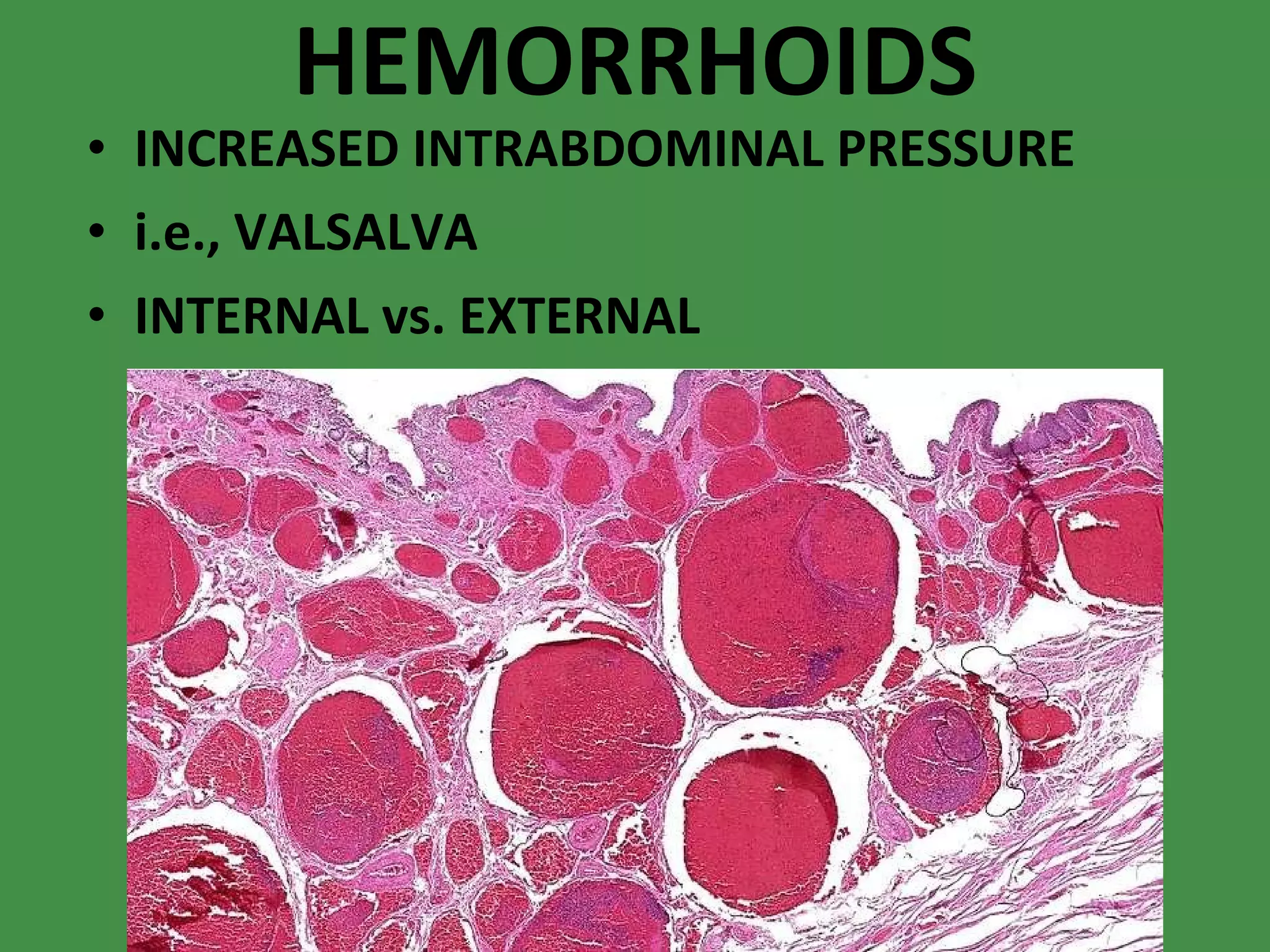
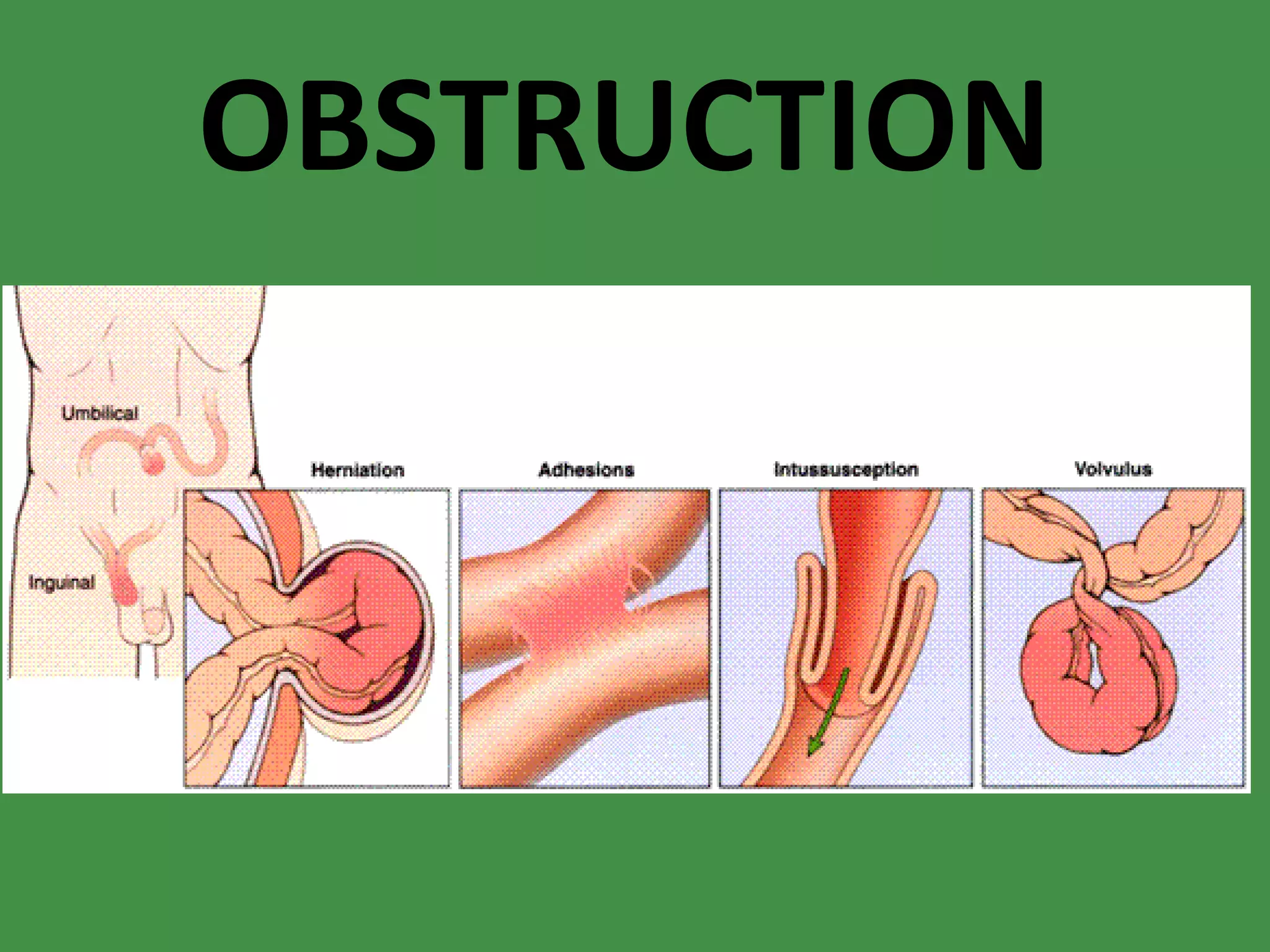
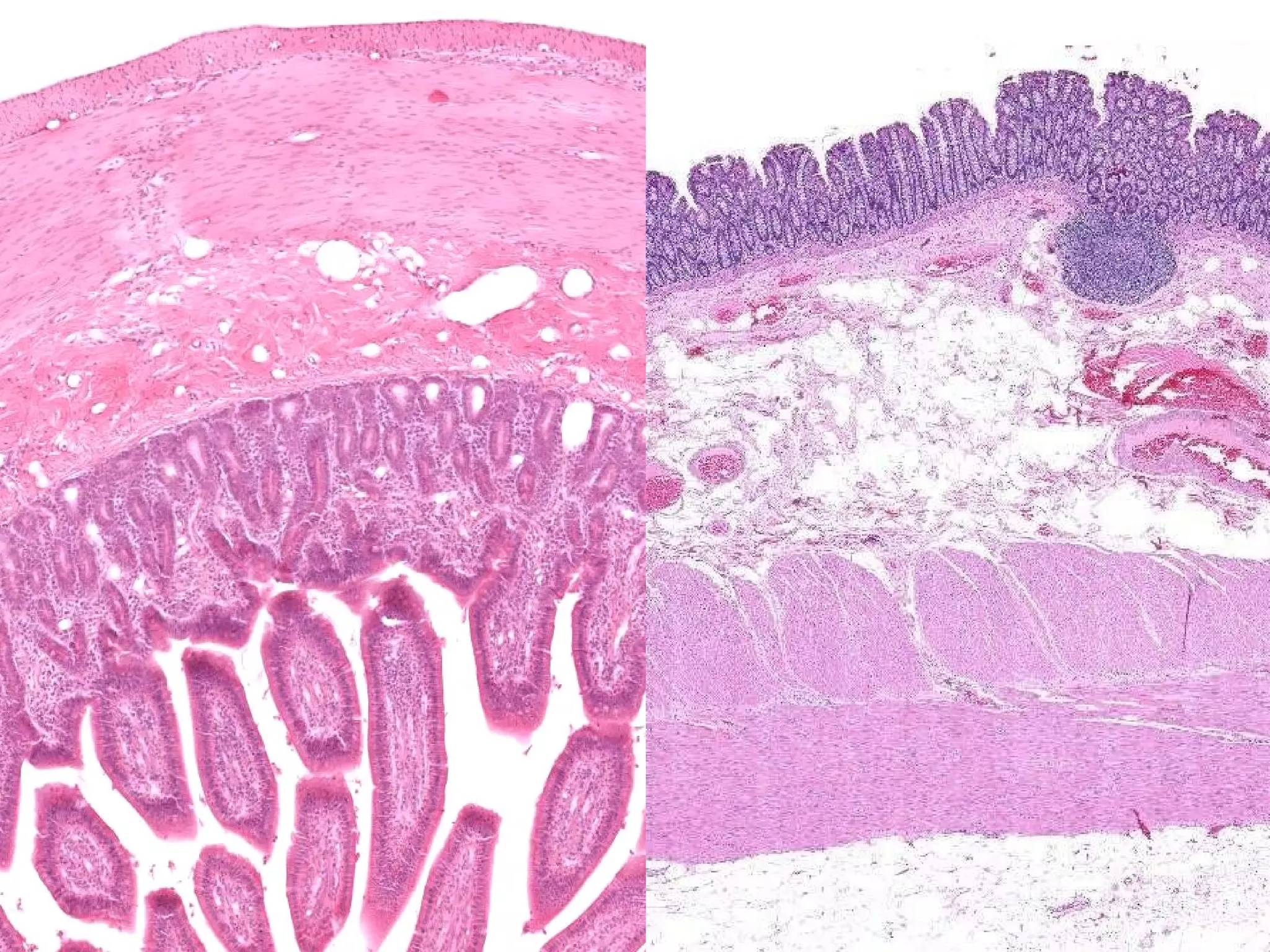
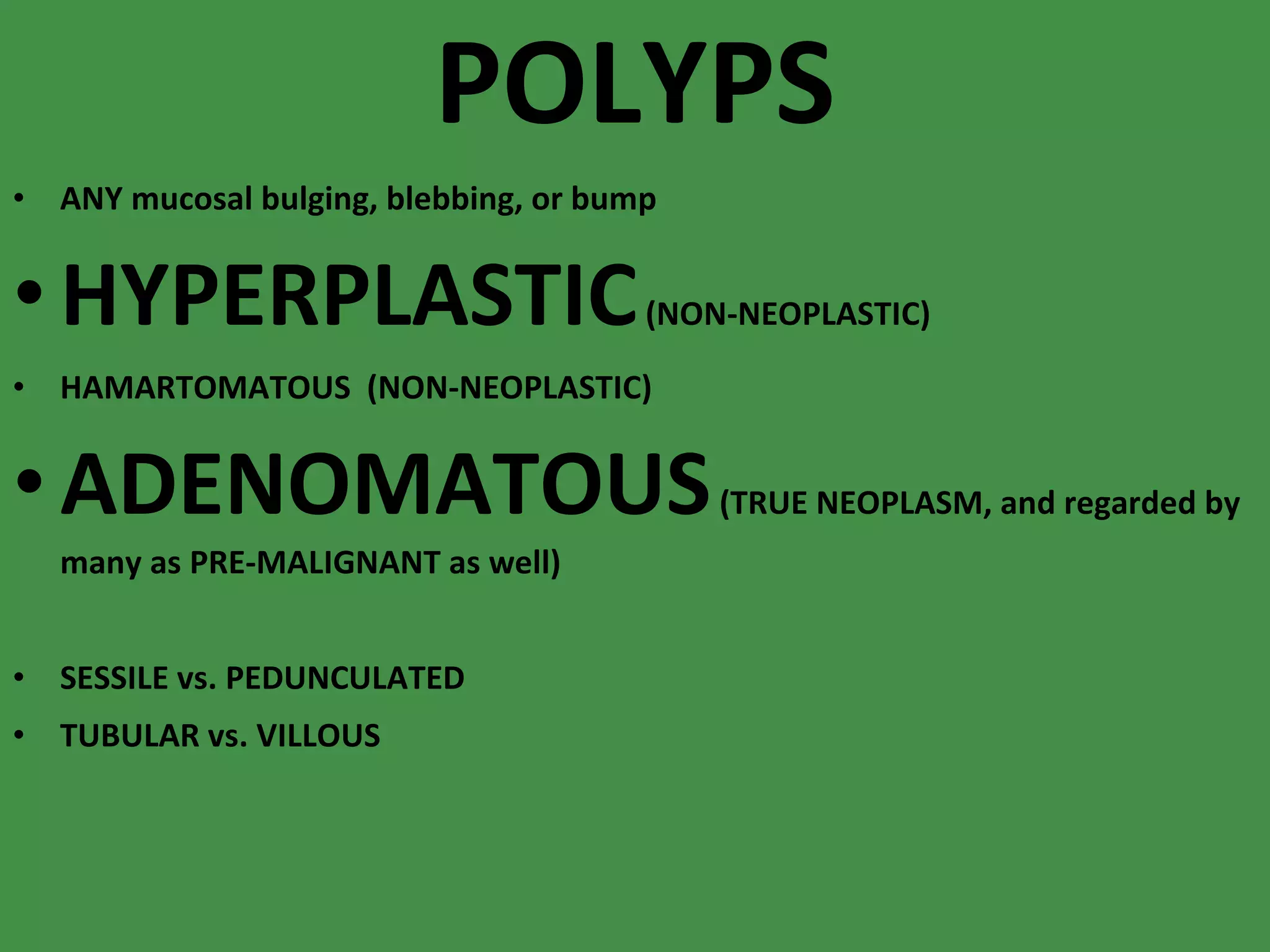
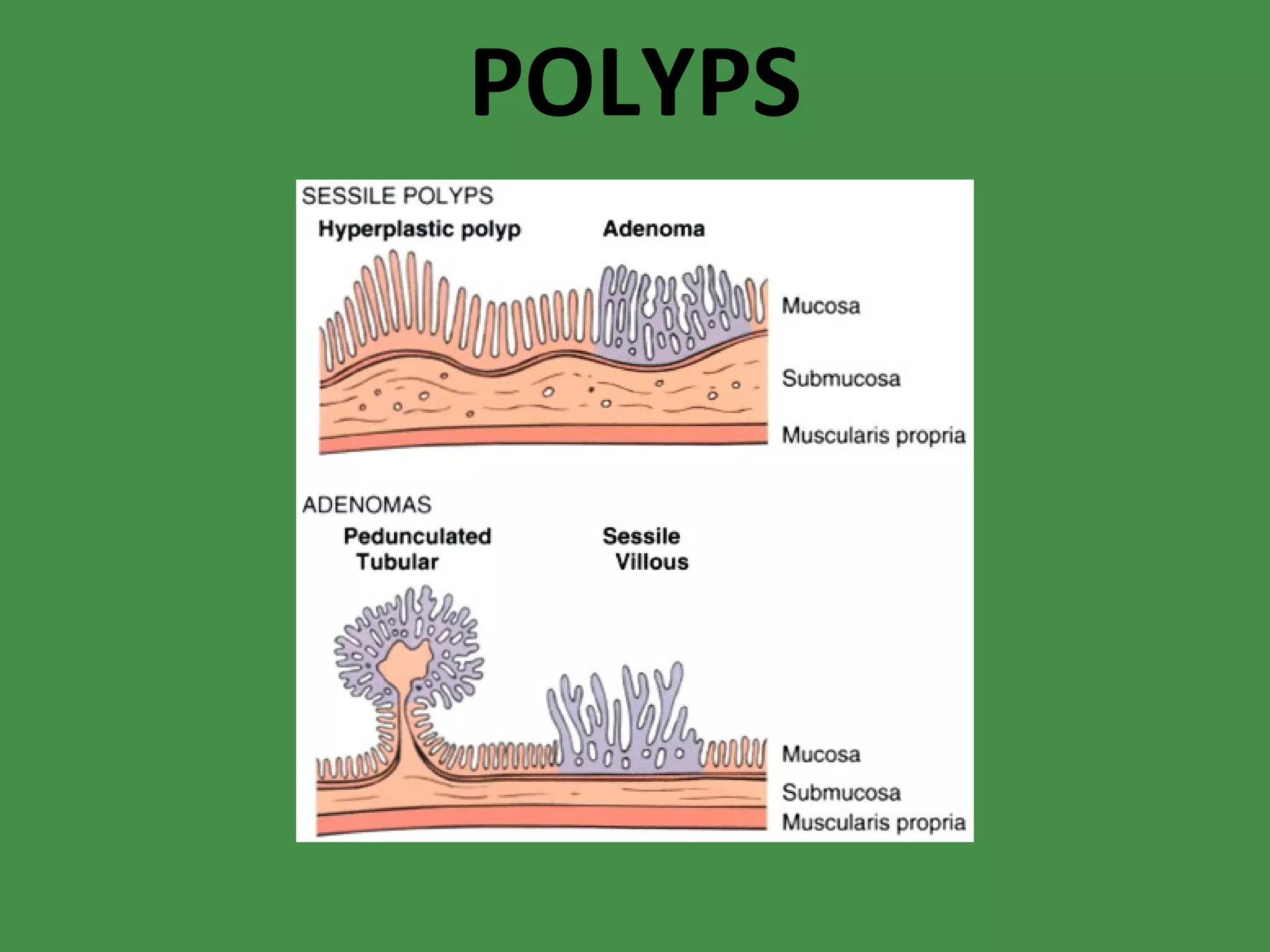
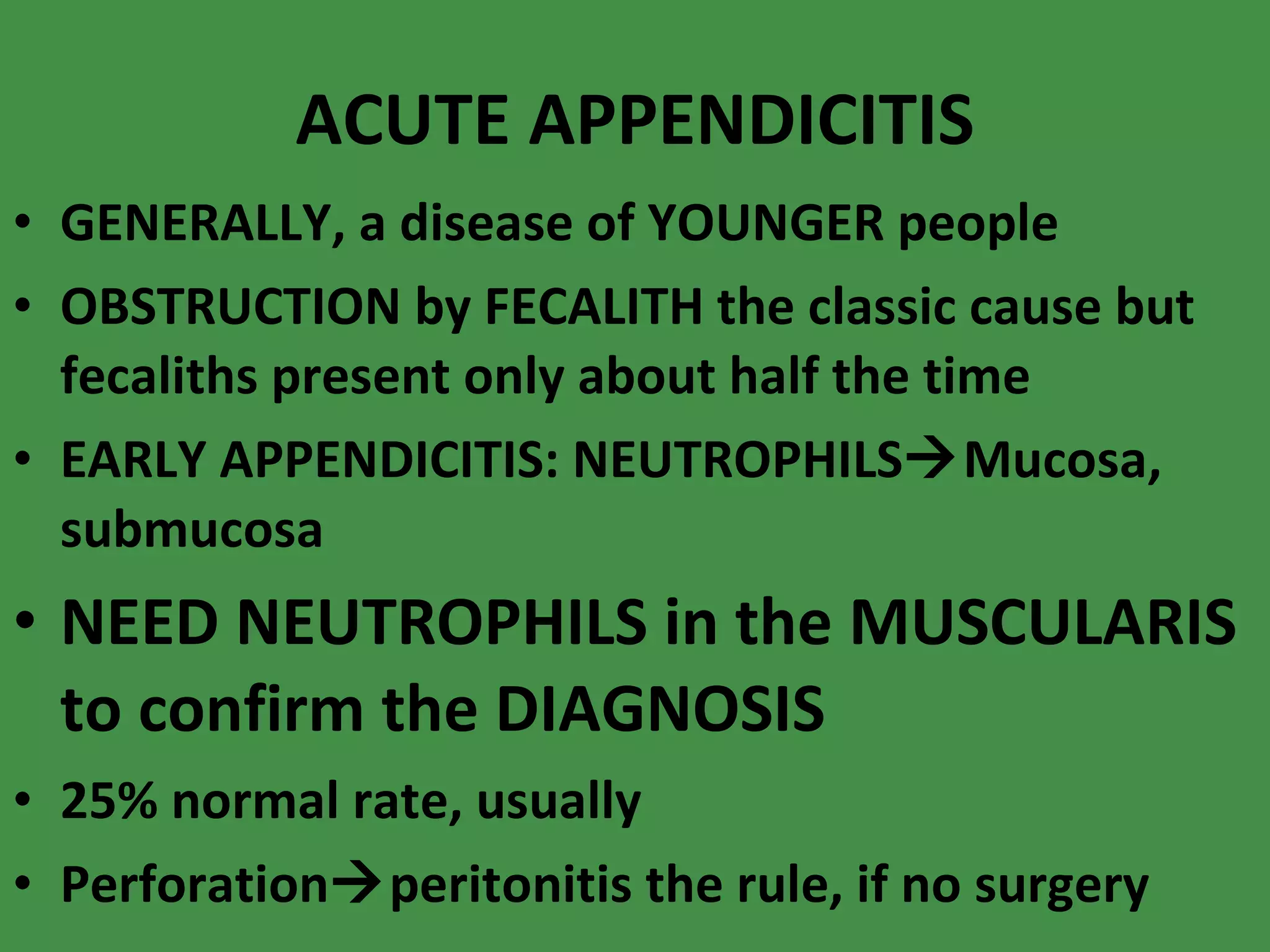
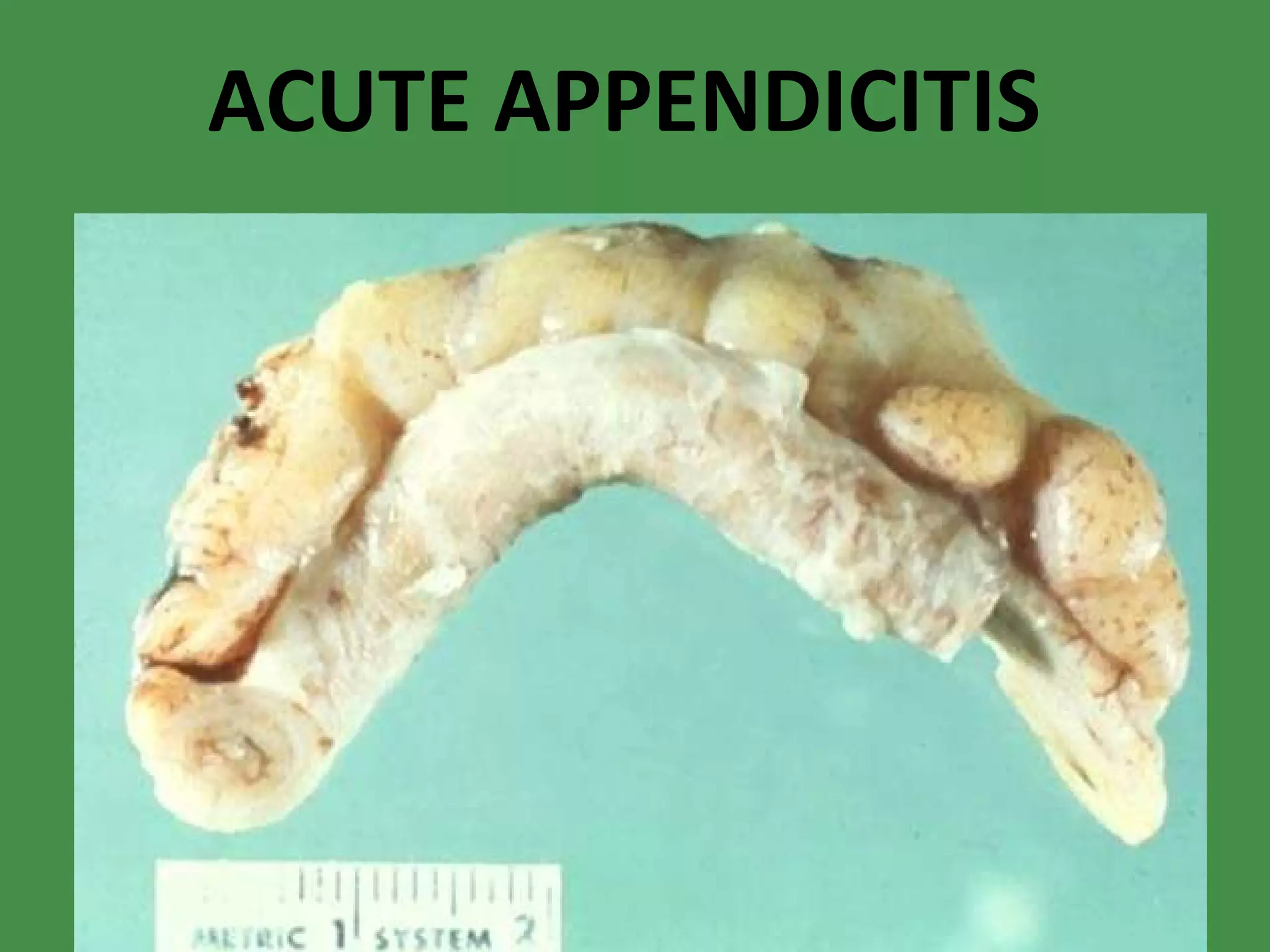
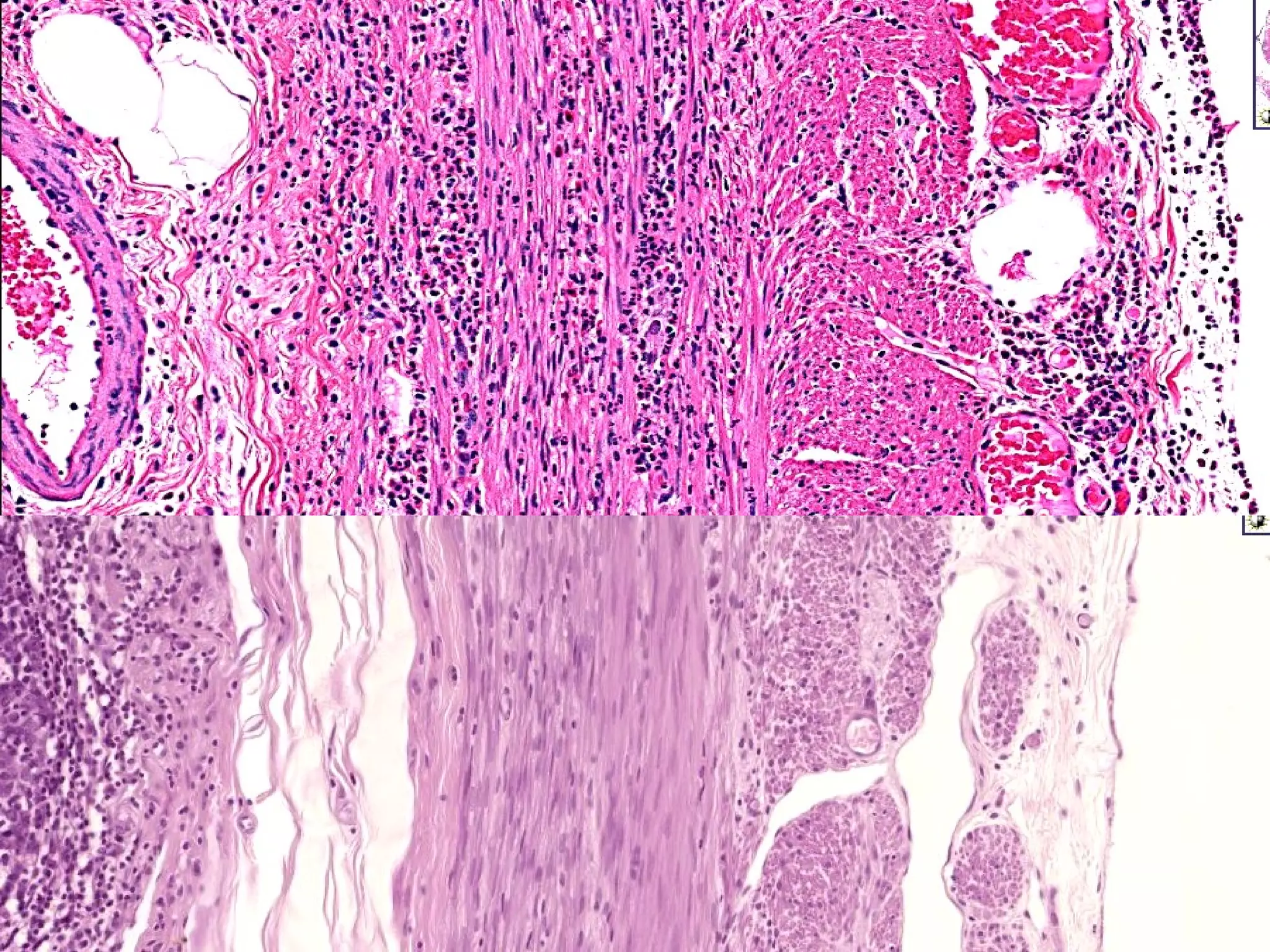
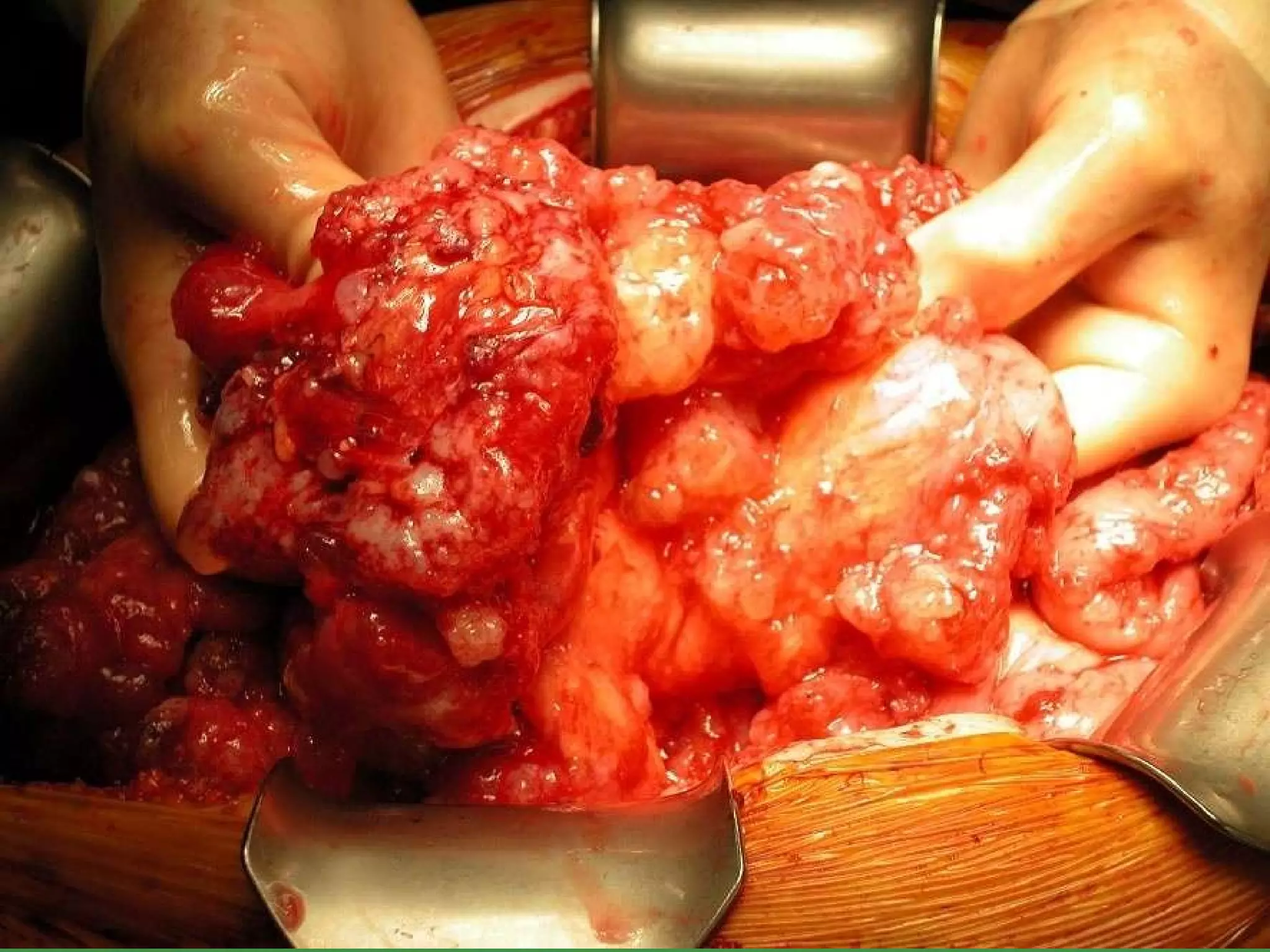
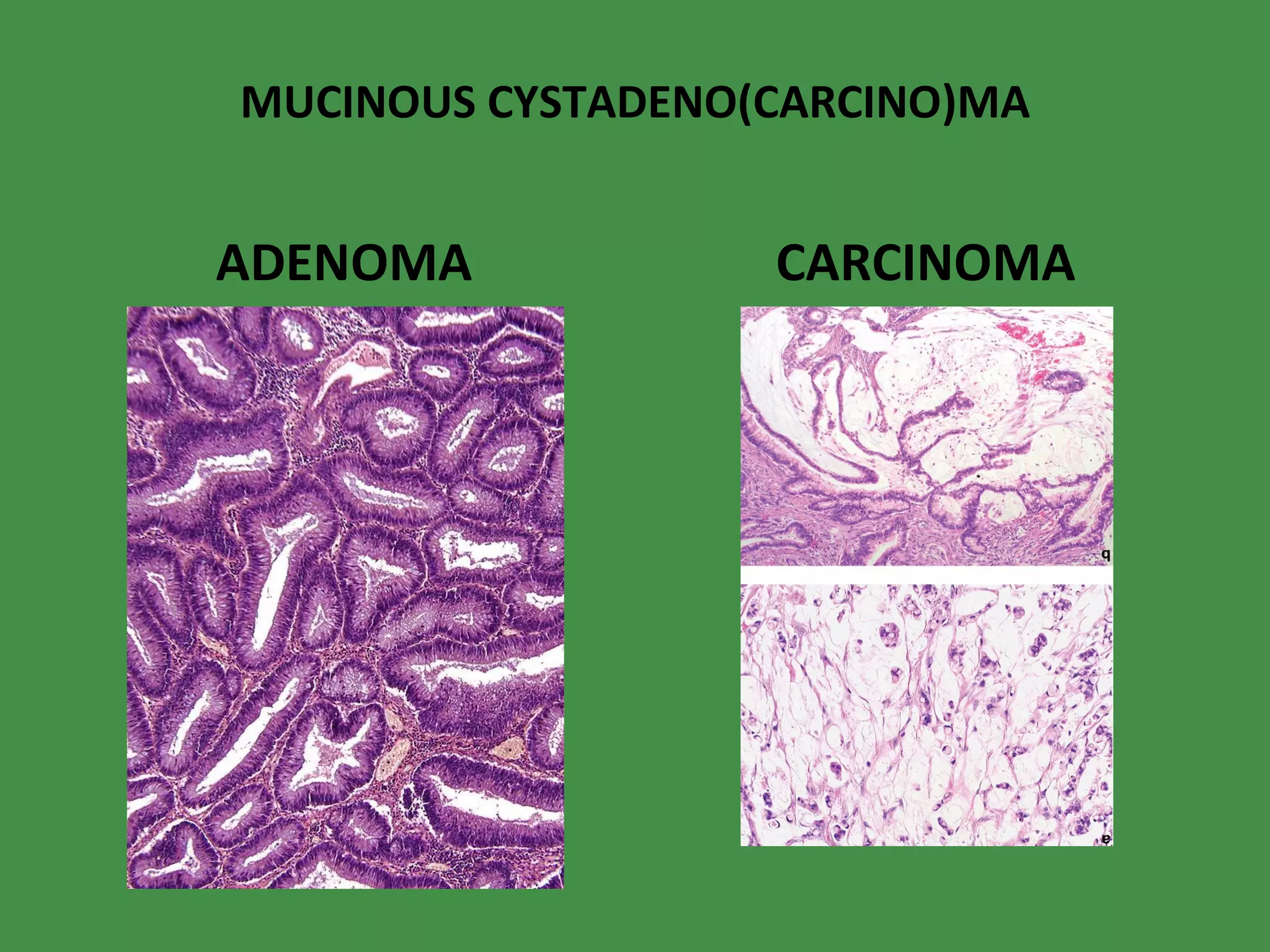
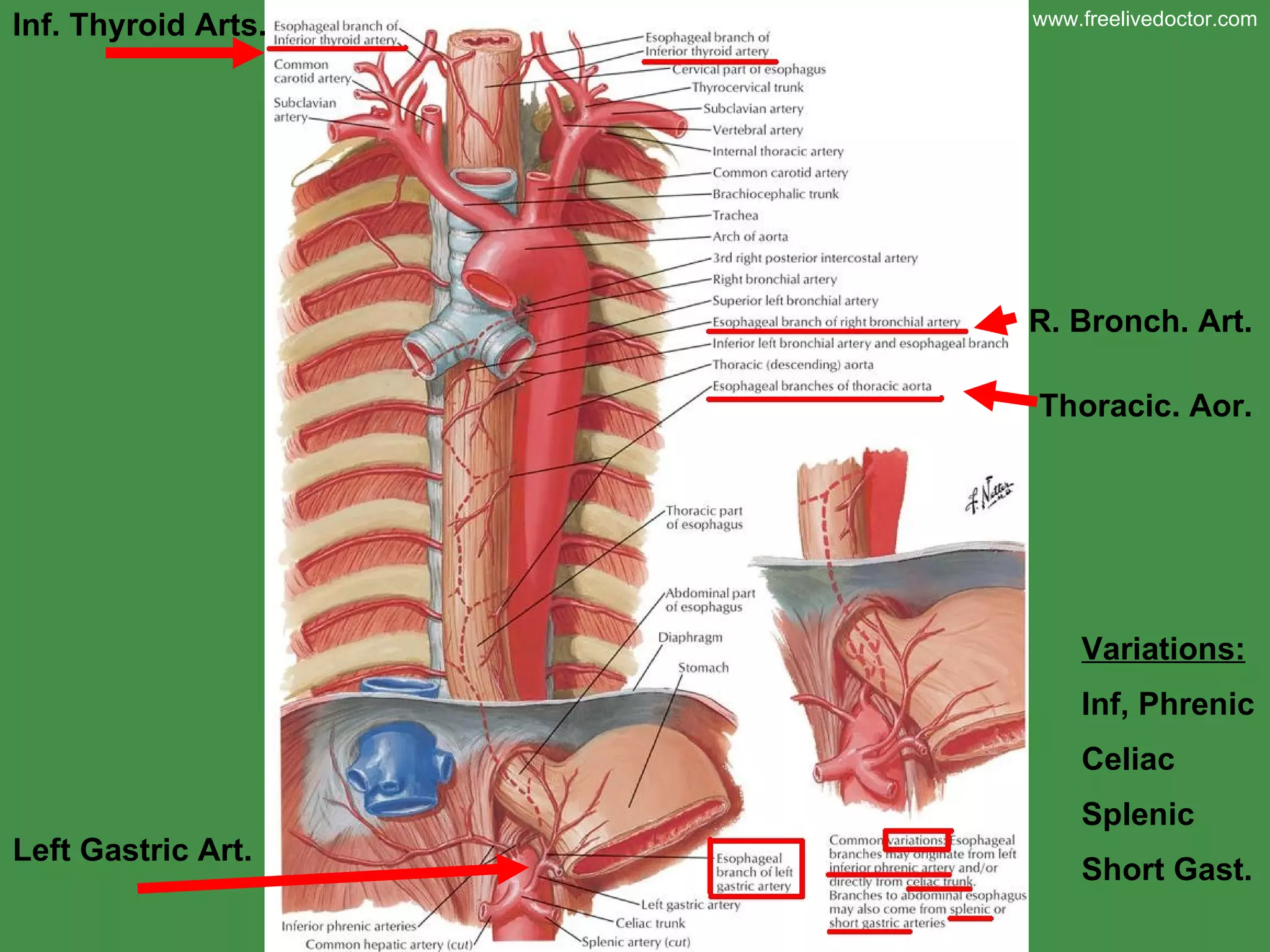
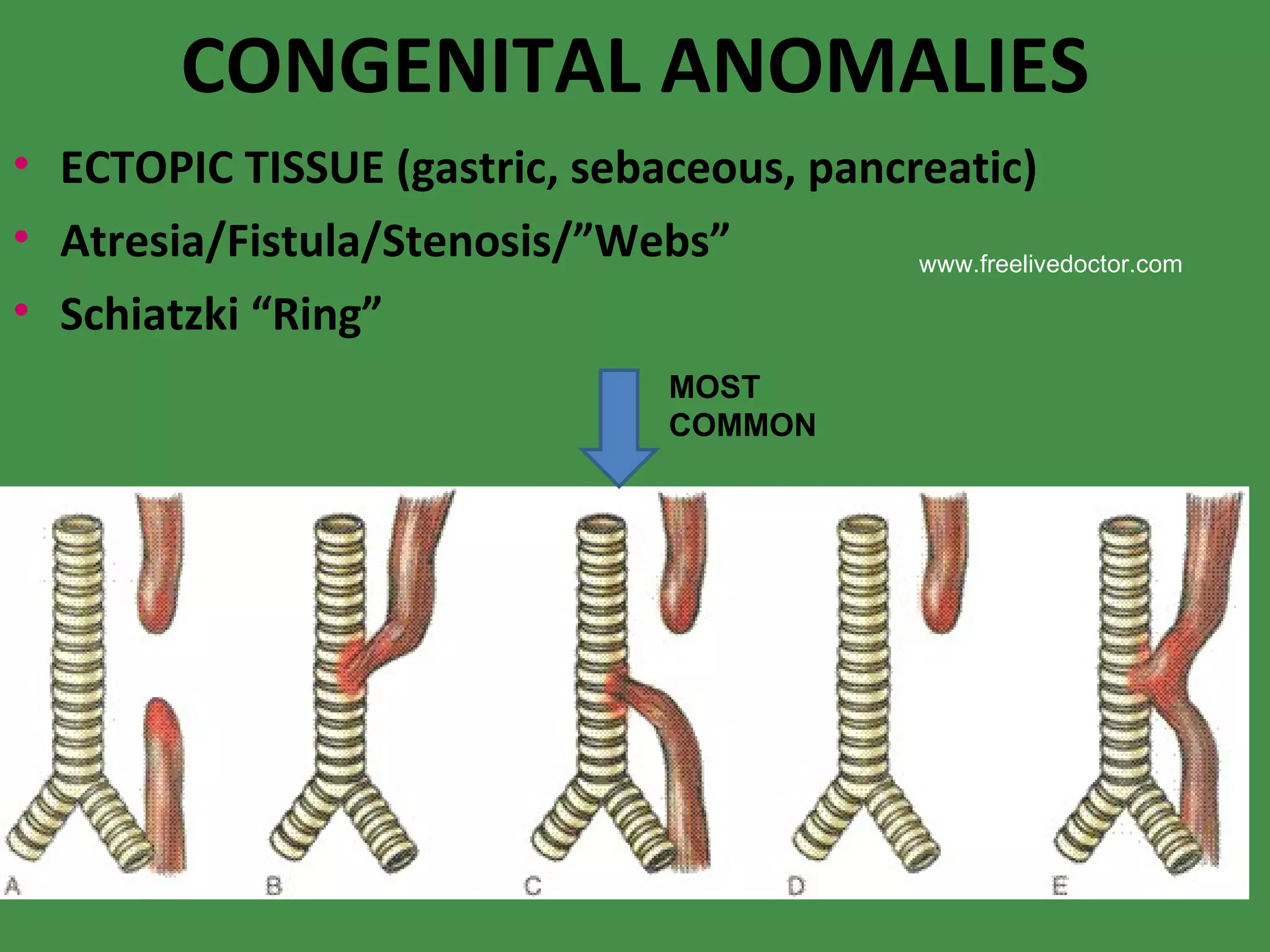
This document provides an overview of the gastrointestinal (GI) tract, including the esophagus, stomach, and small and large intestines. It discusses the normal anatomy, physiology, and various pathologies that can affect these organs. Some key points mentioned include congenital anomalies, infections, inflammatory conditions like gastritis and IBD, vascular issues, obstructions, and benign and malignant tumors.
![MOTOR DISORDERS Achalasia Hiatal Hernia (sliding [95%], paraesophageal) “ ZENKER” diverticulum Esophagophrenic diverticulum Mallory-Weiss tear www.freelivedoctor.com](https://image.slidesharecdn.com/diseasesofgit-100416234728-phpapp01/75/Diseases-of-git-8-2048.jpg)