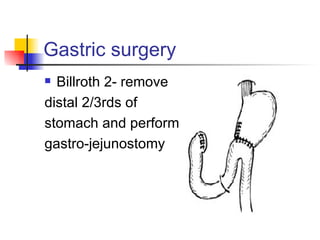
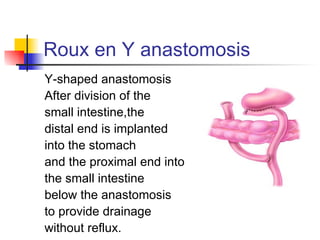
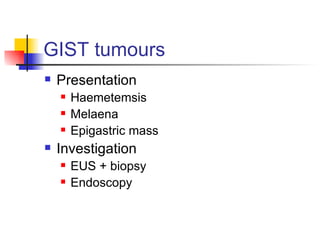
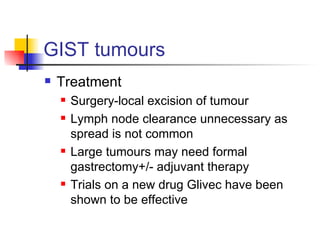
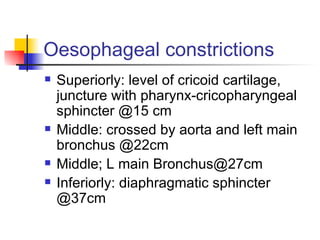
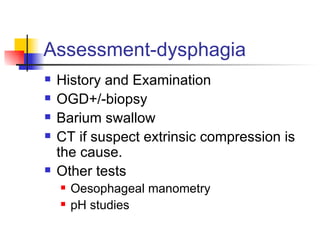
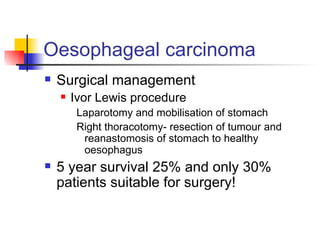
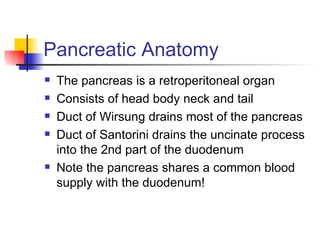
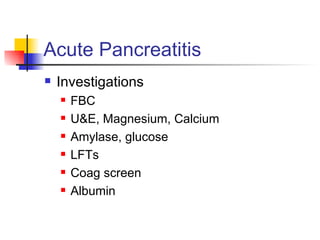
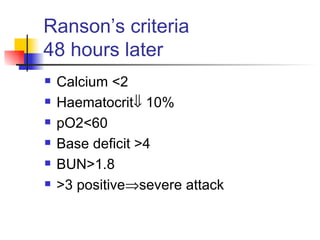
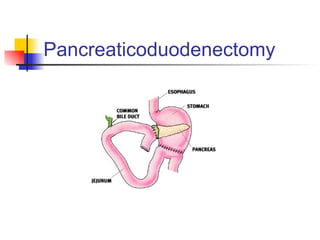
The document discusses upper gastrointestinal surgery, focusing on conditions like peptic ulcer disease, gastric and duodenal ulcers, and various surgical treatments including vagotomy and gastrectomy. It outlines diagnostic methods, treatment options, and the complications associated with different gastrointestinal cancers, especially gastric and esophageal cancers. Additionally, it covers the anatomy of the stomach, pancreas, and esophagus, along with conditions like achalasia and pancreatitis, providing an extensive overview of management strategies and patient care.