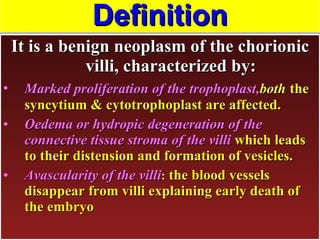
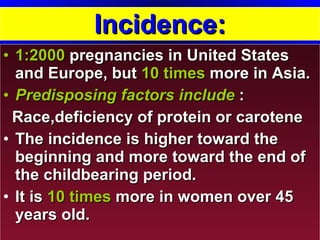
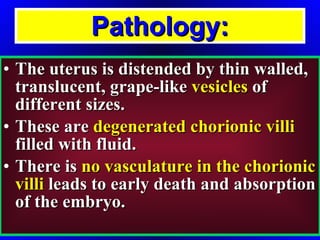
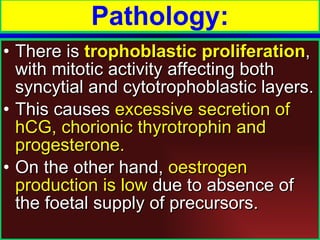
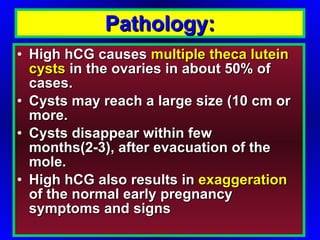
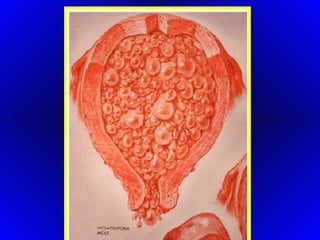
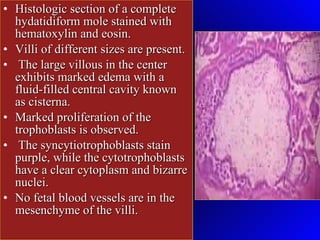
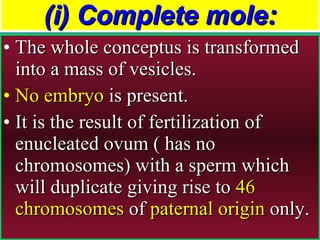
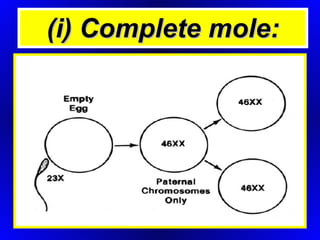
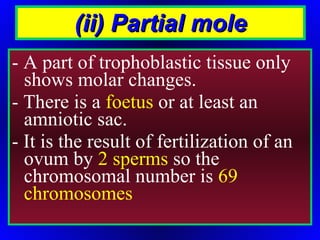
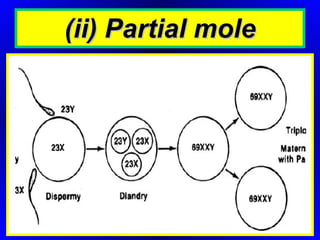
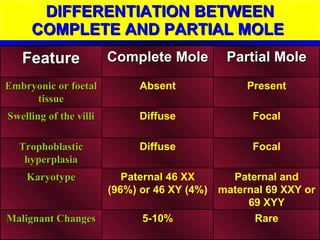
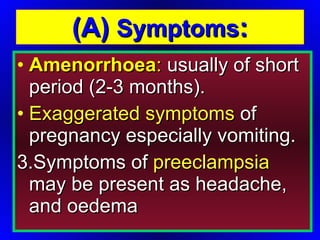
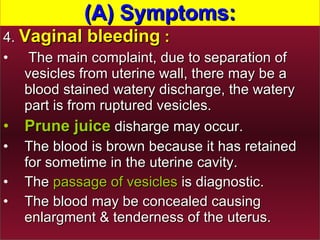
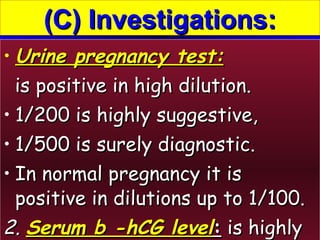
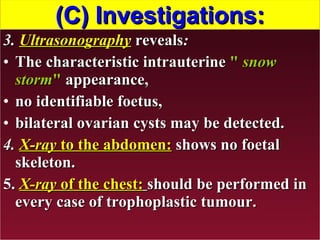
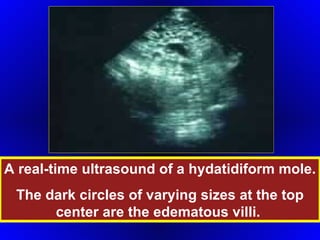
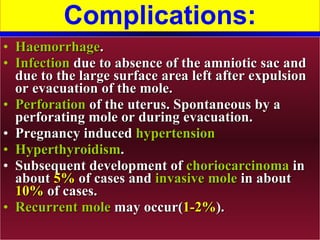
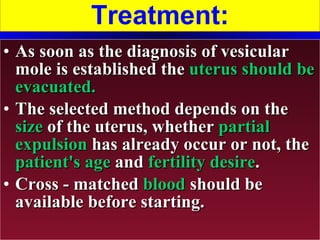
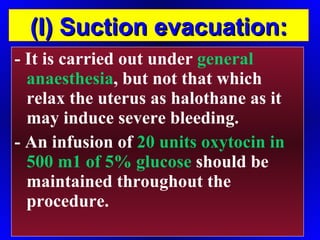
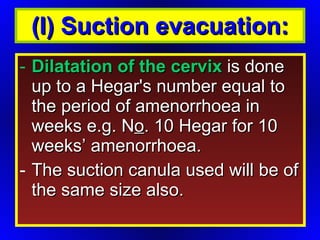
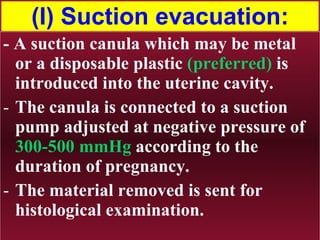
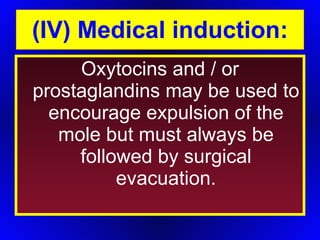
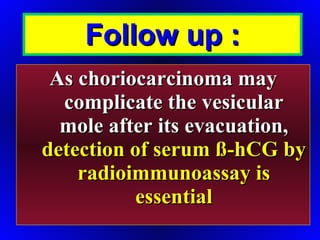
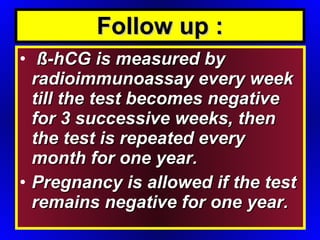
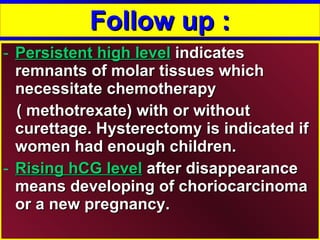
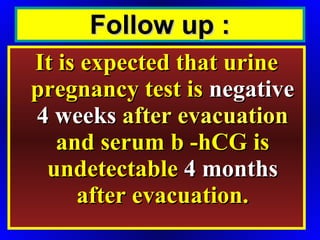
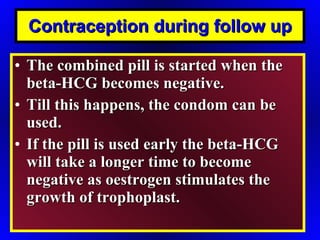
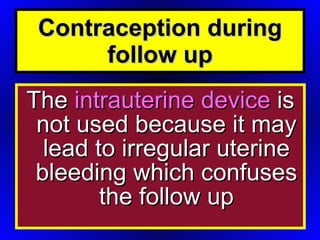
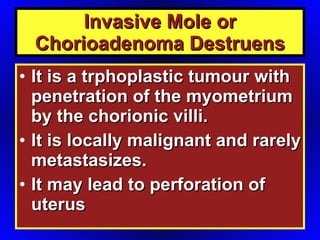
Gestational trophoblastic disease refers to a spectrum of conditions that result from abnormal proliferation of trophoblast tissue. This includes complete and partial hydatidiform moles, as well as invasive moles and choriocarcinoma. Complete moles are characterized by marked trophoblastic proliferation and swelling of the chorionic villi, resulting in vesicles within the uterus. The document discusses the incidence, pathology, diagnosis, treatment and follow up of molar pregnancies. Surgical evacuation is usually performed, and long term follow up is needed to monitor for recurrence and the potential development of choriocarcinoma.