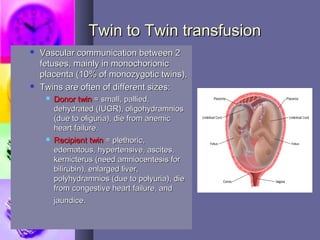
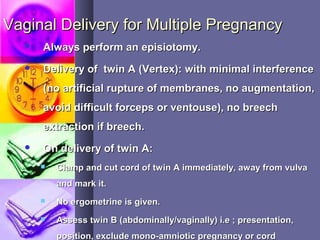
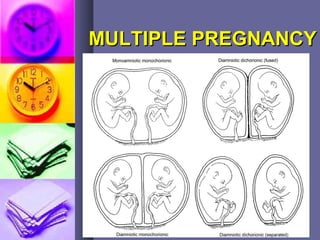
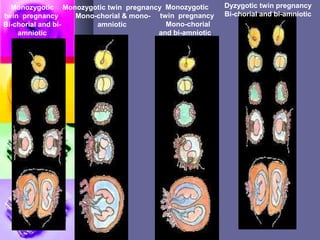
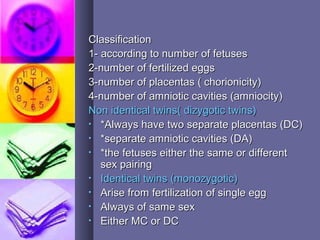
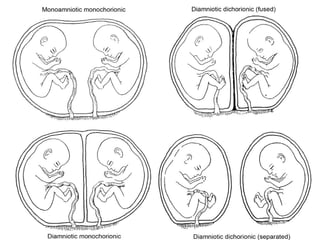
This document discusses multiple pregnancy, also known as twin or higher order pregnancies. It defines multiple pregnancy as the presence of more than one fetus in the abdomen of a pregnant woman. Multiple pregnancies can be categorized based on the number of fetuses as twins, triplets, quadruplets, etc. The document outlines risk factors, classifications, complications, diagnosis, and management of multiple pregnancies. It describes how multiple pregnancies can occur and the different types, and emphasizes the importance of preventing preterm birth in managing these high-risk pregnancies.


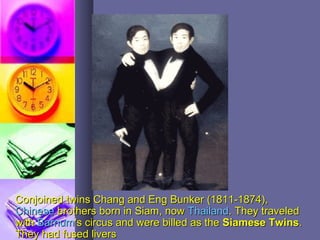
![Conjoined TwinsConjoined Twins
If the division occurredIf the division occurred
just after embryonic discjust after embryonic disc
formation, incomplete orformation, incomplete or
conjoined twins willconjoined twins will
occur. They may beoccur. They may be
joinedjoined
anteriorly [thoracopagus-anteriorly [thoracopagus-
commonest],commonest],
posteriorly [pyopagus]posteriorly [pyopagus]
cephalad [craniopagus] orcephalad [craniopagus] or
caudal [ischiopaguscaudal [ischiopagus].].](https://image.slidesharecdn.com/multiplepregnancy-170921101236/85/Multiple-pregnancy-9-320.jpg)